Infection control in residential care homes for the elderly in Hong Kong (2005-2014)
Hong
Kong Med J 2019 Apr;25(2):113–9 | Epub 10 Apr 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Infection control in residential care homes for the
elderly in Hong Kong (2005-2014)
Grace CY Wong, MB, ChB; Tonny Ng, MMed (Public
Health) Singapore, FHKAM (Community Medicine); Teresa Li, FFPH, FHKAM
(Community Medicine)
Elderly Health Service, Department of Health, Hong
Kong SAR Government, Hong Kong
Corresponding author: Dr Grace CY Wong (grace_cy_wong@dh.gov.hk)
Abstract
Introduction: This serial
cross-sectional survey study aimed to review the trend in various
infection control practices in residential care homes for the elderly
(RCHEs) in Hong Kong from 2005 to 2014.
Methods: Annual cross-sectional
surveys were conducted at all RCHEs in Hong Kong, including
self-administered questionnaires, on-site interviews, inspections, and
assessments conducted by trained nurses, from 2005 to 2014. In all,
98.5% to 100% of all RCHEs were surveyed each year based on the list of
licensed RCHEs in Hong Kong.
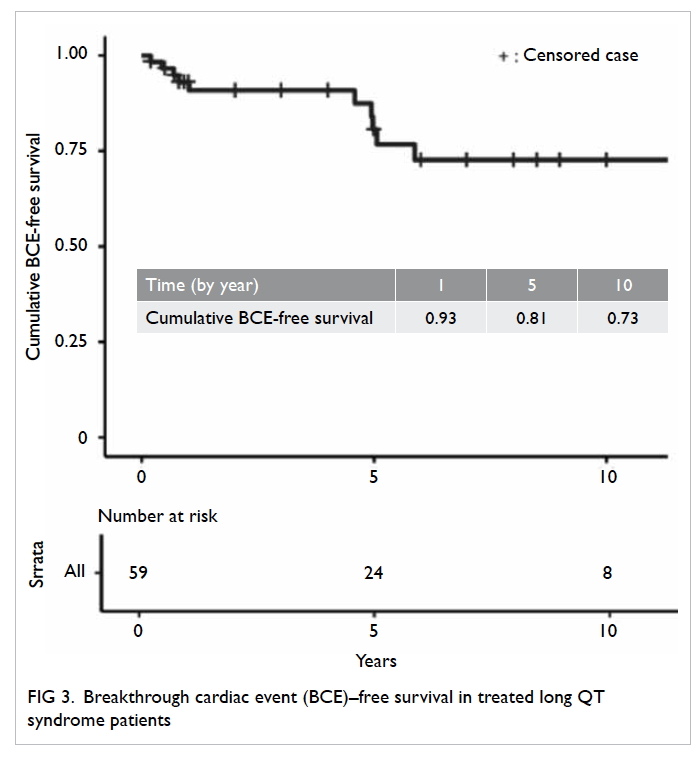
Results: There was a substantial
increase in the proportion of RCHE residents aged ≥85 years, from 40.0%
in 2005 to 50.2% in 2014 (P=0.002). The percentage of RCHE residents
with special care needs also increased, from 22.3% in 2005 to 32.6% in
2014 for residents with dementia (P<0.001) and from 3.4% in 2005 to
5.0% in 2014 for residents with a long-term indwelling urinary catheter
(P<0.001). The proportion of RCHEs with separate rooms for isolation
areas ranged from 73.6% to 80% but did not show any significant trend
over the study period. The proportion of RCHEs with alcohol hand rub
available showed an increasing trend from 25.4% in 2006 to 99.2% in 2014
(P=0.008). The proportion of health or care workers (who were not the
designated infection control officers) passing skills tests on hand
washing techniques increased from 79.2% in 2006 to 91.5% in 2014
(P=0.02). An increasing trend was also observed for the proportion of
infection control officers who were able to prepare properly diluted
bleach solution, from 71.5% in 2005 to 92.2% in 2014 (P=0.002).
Conclusions: For infection
control practice to continue improving, more effort should
be made to enhance and maintain proper practice, and to mitigate the
challenge posed by the high turnover rates of healthcare workers in
RCHEs. Introduction of self-audits on infection control practices should
be considered.
New knowledge added by this study
- From 2005 to 2014, among residents of care homes for the elderly, the proportion of those aged ≥85 years increased significantly.
- If this trend continues, the prevalence of co-morbidities and functional impairment will also continue to increase, leading to further infection control challenges.
- There have been improvements in infection control practices among residential care homes for the elderly in terms of manpower, facilities, practices, knowledge, and skills.
- The most obvious improvements have been in terms of manpower and facilities; more nurses and health workers were recruited, and more residential care homes for the elderly had made alcohol hand rub available. Correct hand washing techniques among health or care workers, availability of alcohol hand rub, and knowledge on the correct method to prepare diluted bleach solution have also improved over the years.
- Improvements in infection control knowledge and skills among staff of residential care homes for the elderly have seemingly reached a plateau.
- Future infection control training should aim to support sustained compliance with proper practices, through the introduction of elements such as self-audits.
Introduction
Residential care services for elderly people in Hong
Kong
In 2016, 8.1% of elderly population in Hong Kong
resided in non-domestic households (ie, residential care homes for the
elderly [RCHEs], hospitals and penal institutions, etc).1 Residential care homes for the elderly are a
heterogeneous group of institutions that provide varying levels of care
for elderly people, who, for personal, social, health, or other reasons,
can no longer live alone or with their families.
There is a mix of government-subvented,
self-financed, and privately run RCHEs in Hong Kong. All RCHEs must be
licensed under the Residential Care Homes (Elderly Persons) Ordinance. The
RCHEs operate according to the code of practice (COP)2 issued by the licensing authority. The COP sets out
guidelines, principles, procedures, and standards for the operation and
management of RCHEs. A chapter in the COP is devoted to infection control,
requiring the RCHE’s operator to designate an infection control officer
(ICO). The ICO must coordinate and implement infection control measures
within the home according to the infection control guideline issued by the
Centre for Health Protection of the Department of Health.3 Operators of RCHEs are required to report specific
infectious disease cases and outbreaks to the authorities.
Visiting health teams
Eighteen visiting health teams (VHTs) are
established under the Elderly Health Service of the Department of Health
in Hong Kong. Comprising 47 nurses, the teams reach out into the community
and residential care settings to conduct health promotion activities for
the elderly people, and carers of elderly people, aiming to increase the
health awareness and the self-care ability of elderly people, and to
enhance the quality of caregiving.
The first on-site assessment covering all RCHEs in
Hong Kong on infection control performance was conducted by VHTs between
August and October 2003 as an enhanced measure in response to the severe
acute respiratory syndrome (SARS) outbreak. Since then, annual assessments
have been conducted by VHTs to assess and monitor the effectiveness of
infection control measures and to identify the training needs of
healthcare staff working in RCHEs, so as to plan for training activities
for the following year. Assessment results are shared with relevant
stakeholders, including the licensing authority and the community
geriatric teams of public hospitals which provide outreach personal
medical care to residents of RCHEs. Feedback is also provided to RCHE
staff, to increase their alertness and encourage improvements.
This study aimed to review the 10-year trend in
infection control practices in RCHEs in Hong Kong, based on results of the
annual VHT assessments conducted from 2005 to 2014.
Methods
Assessment of all RCHE facilities, and the
infection control knowledge and skills of staff are conducted annually via
structured questionnaires and observational checklists.
Sample size and coverage rate
The annual surveys cover all RCHEs in Hong Kong
from 2005 to 2014, based on the lists maintained by the licensing
authority.4 The coverage rate was
98.5% to 100% from 2005 to 2014. A few RCHEs were not covered because they
were either non-operating (under renovation or recently closed) or refused
the VHT service. These RCHEs were excluded from analysis.
Data collection
The surveys were conducted from August to October
each year, based on an assessment protocol developed by doctors and nurses
of the VHTs, and with reference to the COP,2 the prevailing “Guidelines on
Prevention of Communicable Diseases in Residential Care Home for the
Elderly”3 and overseas guidelines
on infection control practice.5 6 7
Resident demographics, staff profiles, information on environment and
facilities related to infection control, and knowledge and skills of the
ICO and other staff were collected in the surveys. The assessments were
divided into four parts:
Part I: The characteristics and profiles of
residents and staff of the RCHEs, including the subjective training needs
of staff, were collected through a self-administered questionnaire (online
supplementary Appendix) completed by the person-in-charge of the
RCHE, prior to the site visit by the VHT.
Part II: The environmental conditions and
facilities related to infection control in RCHEs were assessed by a VHT
nurse during the site visit.
Part III: The health monitoring and record keeping
practices in RCHEs were assessed during the site visit.
Part IV: The knowledge and skills on infection
control of staff in RCHEs were assessed in face-to-face interviews during
the site visit. The ICO (or other staff, depending on the topic being
assessed) of each RCHE was assessed. An additional member of staff (either
a health worker or care worker) was also selected at random for assessment
on hand washing technique.
After the assessments, data were either
double-entered or double-checked by two separate colleagues. In addition,
10% of the questionnaires were audited by an independent colleague, who
rechecked all questionnaires if the error rate detected was greater than
0.5% of data fields. Descriptive statistics on the characteristics of the
residents and the health/personal care staff were tabulated. Categorical
data were analysed by either Chi squared test or Fisher’s exact test while
trend analysis was conducted by linear regression. A linear trend is
reported as significant when the slope of the regression line is
statistically different from zero. All analyses were conducted using SPSS
(Windows version 24.0; IBM Corp, Armonk [NY], United States). This report
was prepared following the STROBE (Strengthening the Reporting of
Observational Studies in Epidemiology) statement.8
Results
The majority of RCHEs (ranging from 73.9% to 75.7%,
between 2005 and 2014) were commercially operated RCHEs (“private RCHEs”).
The remaining 24.3% to 26.1% were “non-private RCHEs”, comprising those
that received subsidies or subventions from the government and those that
were non–profit making and self-financing in nature.9
Part I: Characteristics of residents and staff of
residential care homes for the elderly
Age profile of residents
The age profile of the residents in RCHEs from 2005
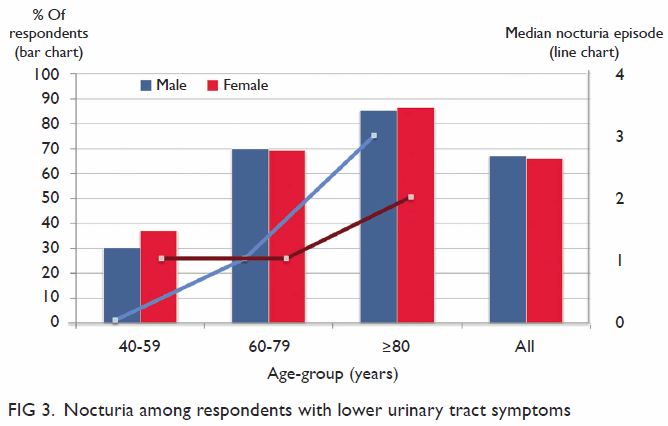
to 2014 is shown in the Figure. An apparent ageing trend is observed with
the proportion of RCHE residents aged ≥85 years rising from 40.0% (23 718)
in 2005 to 50.2% (31 149) in 2014 (P=0.002).
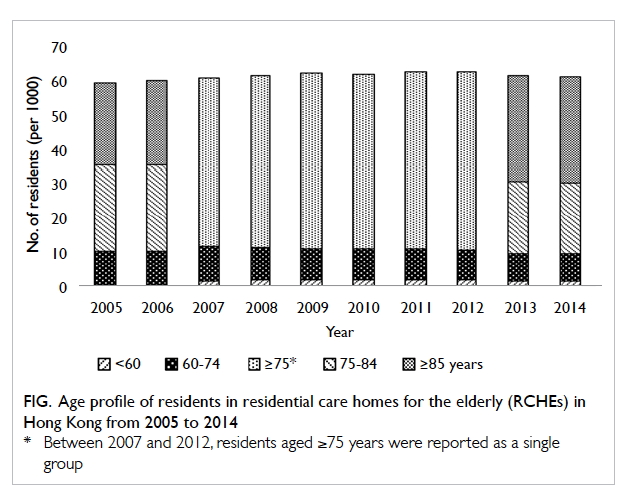
Figure. Age profile of residents in residential care homes for the elderly (RCHEs) in Hong Kong from 2005 to 2014
Residents with special care needs
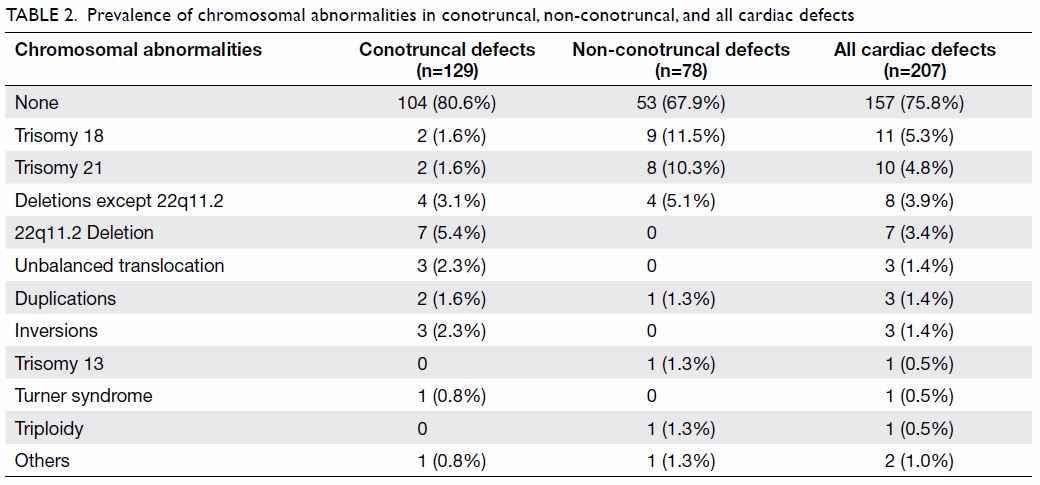
Table 1 shows the percentage of residents with
special care needs from 2005 to 2014. The proportion of residents with
dementia increased from 22.3% in 2005 to 32.6% in 2014 (P<0.001). The
percentage of residents with a long-term indwelling urinary catheter
increased from 3.4% in 2005 to 5.0% in 2014 (P<0.001), representing a
47% increase in the number of patients with a long-term indwelling urinary
catheter.
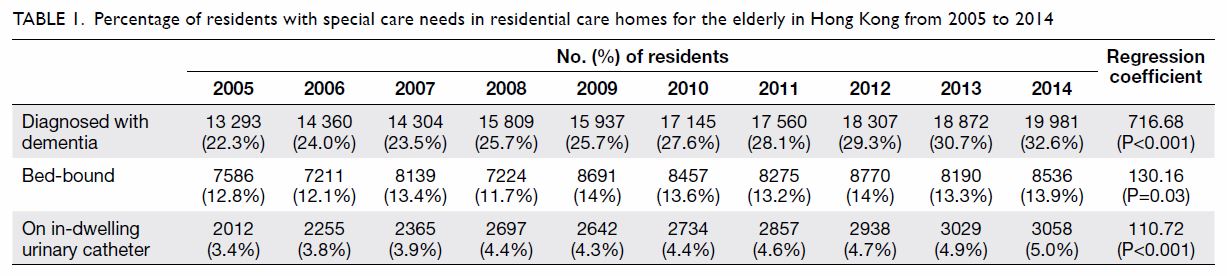
Table 1. Percentage of residents with special care needs in residential care homes for the elderly in Hong Kong from 2005 to 2014
Manpower in residential care homes for the elderly
The resident-to-staff ratios in RCHEs from 2005 to
2014 are shown in Table 2. The major types of staff in RCHEs in Hong
Kong are professionally qualified nurses (including registered nurses and
enrolled nurses registered under the Nursing Council of Hong Kong), health
workers who have completed basic training recognised by the licensing
authority, care workers who have not received any official training, and
other staff including allied health and supporting staff. There were no
significant changes in overall resident-to-staff ratio over the study
period. For nurses and health workers, the overall manpower ratios
improved from 30:1 and 27:1 in 2005 to 23:1 and 17:1 in 2014, respectively
(both P<0.001). Increases in numbers of full-time and part-time nurses
and health workers contributed to the improvements in these ratios.
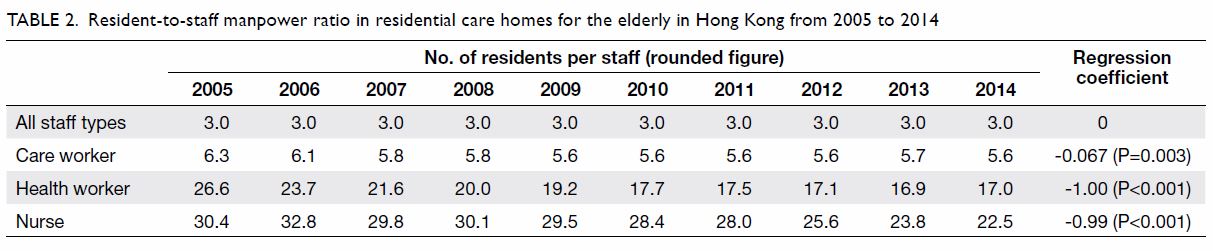
Table 2. Resident-to-staff manpower ratio in residential care homes for the elderly in Hong Kong from 2005 to 2014
There was an observable difference in terms of the
number of nurses between private RCHEs and non-private RCHEs. In 2014, the
resident-to-nurse ratio was 58:1 in private RCHEs compared with 11:1 in
non-private RCHEs. In fact, the majority of private RCHEs (70.9%) did not
employ any nursing staff. In contrast, only 3.8% of non-private RCHEs did
not have any nursing staff. Only 18.5% of private RCHEs had assigned
nurses as ICOs, whereas the percentage was 93.0% in non-private RCHEs. The
rest of the RCHEs appointed health workers as ICOs.
Part II: Infection control—environment and facilities
Common area
The RCHEs are collective living places where
communicable diseases can easily spread through contact with the
environment. Therefore, it is essential for RCHEs to be equipped with
proper facilities to prevent outbreaks. After years of promotion, the
proportion of RCHEs with alcohol hand rub increased significantly from
25.4% in 2006 to 99.2% in 2014 (P=0.008), as shown in Table
3. Nevertheless, further examination of a selected bottle of alcohol
hand rub at each of the RCHEs revealed that, in 2014, only 92.4% of RCHEs
had alcohol hand rub that had proper concentrations and were within the
expiry dates. Although this was an improvement from 64.1% in 2008, a
difference in performance was observed in 2014, with only 90.7% of private
RCHEs having proper alcohol hand rub, compared with 97.3% of non-private
RCHEs (P=0.003).
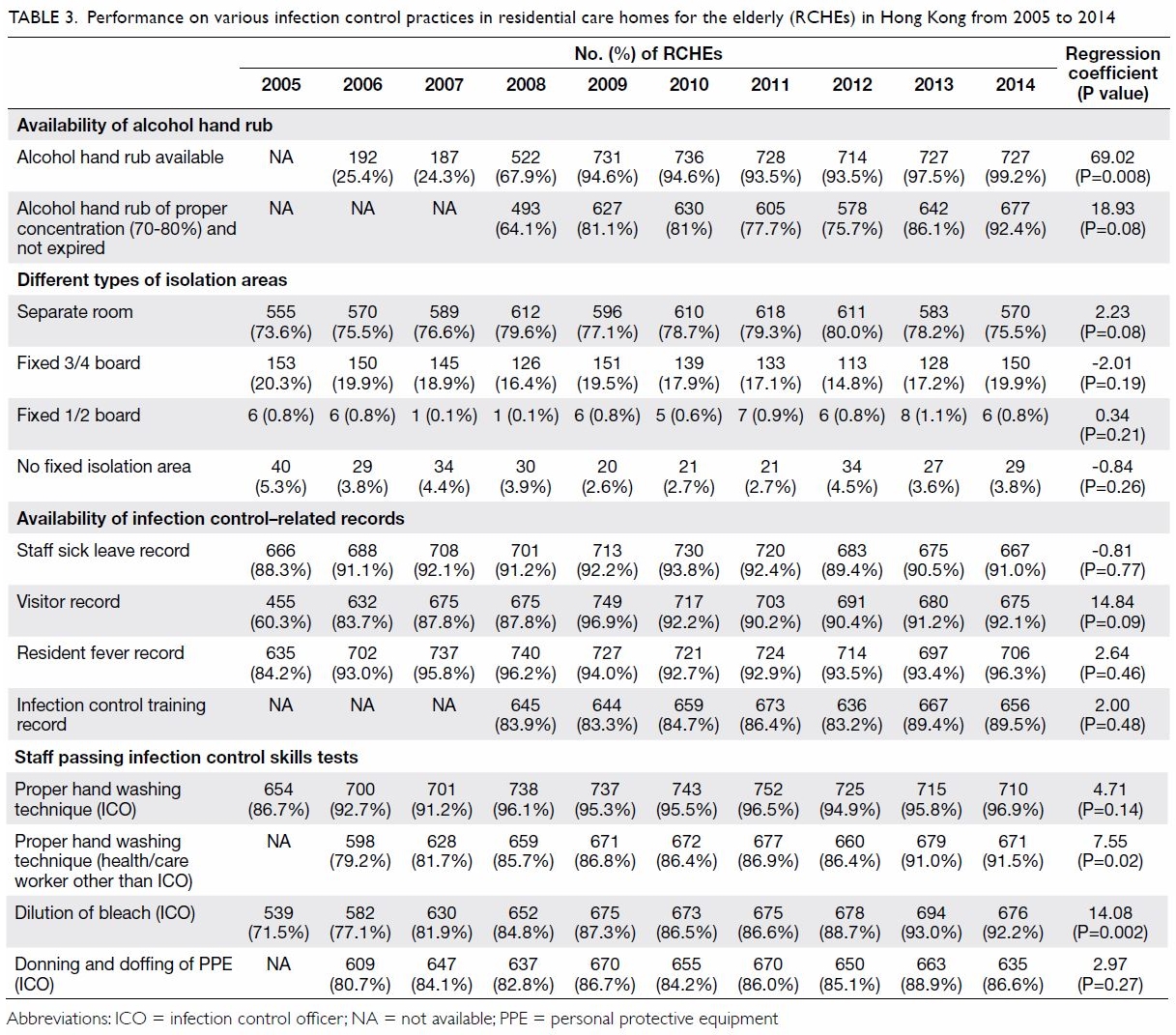
Table 3. Performance on various infection control practices in residential care homes for the elderly (RCHEs) in Hong Kong from 2005 to 2014
Isolation area
According to the COP for RCHEs,2 an isolation facility is a basic requirement for an
RCHE and is defined as “a designated area or room with good ventilation,
adequate space for equipment for proper disposal of personal and clinical
wastes, and basic hand hygiene and hand-drying facilities as well as
electric call bell.” The proportion of RCHEs equipped with a designated
room as an isolation area for fever cases ranged from 73.6% to 80.0%
between 2005 and 2014. No obvious trend was observed. In 2014, 19.9% and
0.8% of RCHEs were still only able to provide fixed boards of either
three-quarters or half the height of the room, respectively, as partitions
for the isolation area instead of providing separate rooms (Table
3). More non-private than private RCHEs were able to designate a
separate room for isolation in 2014 (90.3% vs 73.3%, P<0.05). However,
of the rooms designated as isolation areas, 1.5% in non-private RCHEs and
5.3% in private RCHEs were found to be occupied by residents without the
need for isolation, or used for storage.
Part III: Health monitoring and record keeping in
residential care homes for the elderly
For contact tracing and outbreak investigation, a
proper record system is essential. Only 60.3% of all RCHEs kept proper
visitors’ record in 2005, increasing to 92.1% in 2014. There were also
moderate improvements in the maintenance of sick leave records for staff,
fever records for residents, and training records on infection control for
staff, as shown in Table 3. However, a statistically significant trend
could not be identified.
Part IV: Infection control skills and practice
The ICO’s skill at hand washing, wearing and
removing of personal protective equipment, and preparing bleach solution
for environmental disinfection were tested in each RCHE. In addition to
assessing the ICO, a health worker or care worker was also selected at
random for hand washing technique auditing. The proportion of ICOs with
proper hand washing technique increased from 86.7% in 2005 to 96.9% in
2014, although a statistically significant trend was not observed
(P=0.14). However, an improvement trend was observed for non-ICO
health/care workers from 79.2% in 2006 to 91.5% in 2014 (P=0.02) [Table
3]. The proportion of ICOs with proper skills on wearing and
removing of personal protective equipment ranged from 80.7% to 88.9%
between years 2006 and 2014 (P=0.27). The proportion of ICOs who were able
to prepare bleach solution with the proper concentration showed an
improving trend from 71.5% in 2005 to 92.2% in 2014 (P=0.002).
Discussion
Infectious disease outbreaks are major concerns for
RCHEs as they often lead to significant morbidity and mortality. Local
data on infection control practices among RCHEs are limited. The current
study is the first institution-based serial survey on the trend of
infection control practices among RCHEs.
Residents of RCHEs are often functionally impaired,
putting them at higher risk of infection.10
Our results show that the proportion of RCHE residents aged ≥85 years is
increasing (Fig). This is expected to result in increased
prevalence of co-morbidities and functional impairment, leading to further
infection control challenges.
There have been improvements in infection control
practices among RCHEs over the study period from 2005 to 2014, in terms of
manpower, facilities, practices, knowledge, and skills. The improvement
was most obvious in terms of manpower and facilities. More nurses and
health workers were recruited into RCHEs, and common areas equipped with
alcohol hand rub. There was also a 10.2% improvement in hand washing
skills and a 5.9% improvement on skills of wearing and removing of
personal protective equipment among ICOs during the study period (Table
3). Possible contributory factors to such improvements may include
the overall increased level of awareness on the importance of infection
control, increased availability of manpower11
12 13
and financial resources, and improved access to infection control training
programmes.
Despite the improvements in infection control,
there are some areas of concern that are worth noting.
First, there was a sharp initial increase in the
number of RCHEs that had separate rooms as isolation areas in 2004. This
was likely an enhancement measure in response to the SARS outbreak in
2003. However, the proportion of RCHEs with separate isolation rooms has
remained stable at around 70% since then, despite ongoing training and
education. Possible explanations for this plateau include lack of space,
other competing demands, and other resourcing issues.
A similar plateau effect was also observed for
knowledge and skills on infection control measures. The RCHE staff’s
knowledge on the assessment items significantly improved (to near 90% for
most topics), then showed little further improvement.
Non-private RCHEs consistently performed better
than private RCHEs, especially in terms of nursing manpower, availability
of proper isolation areas, and availability of effective alcohol hand rub.
There is a fundamental funding difference between private and non-private
RCHEs. In addition to complying with statutory requirements, government
subvented RCHEs or those providing subsidised places (eg, RCHEs
participating in bought place schemes) are also required to meet quality
standards set out in the service contracts with the government. However,
private RCHEs not participating in such schemes are only required to
comply with the minimum statutory standards, such that service quality
among private RCHEs remains variable.14
Moreover, the high staff turnover rate in the
private sector may also explain why the performance of infection control
in private RCHEs still lags behind that of non-private RCHEs, because
knowledge and skills are not retained when trained care workers leave.15
There are several main limitations to our study.
First, although RCHE staff have attained a generally adequate level of
knowledge and skills on infection control, the implementation or the
extent of adoption of these skills in daily practice could not be
ascertained by our assessments which took the form of knowledge and skill
tests rather than covert observation of real practice. In addition, the
achieved results might not be representative, because the pre-scheduling
allowed ample lead time for the staff of the RCHEs to prepare for the
assessment. Unannounced visits and covert observation might provide a more
accurate assessment of staff skill levels and the extent of application of
such skills in daily practice, although covert observation itself may pose
other practical challenges.16
Second, it was not feasible for us to interview all
staff during our site visits, because the RCHEs must maintain routine
service for residents. During site visits, we assessed the knowledge and
practice of only the ICO and one additional health or care worker. The
performance of these two selected workers might not be representative of
all staff of the RCHE.
Third, to enhance comparability of assessment
results, most questions asked and skills tested were similar between
years. Thus, the assessment content might become predictable as the
assessments were repeated annually. This might have led to survey fatigue
and inability to capture true performance.
With an increasingly frail and ageing cohort of
residents, RCHEs are expected to face a growing risk of infectious disease
outbreaks in the coming decades, especially those involving
multidrug-resistant organisms. Other than general infection control
measures already adopted by the RCHEs, having a stable and well-trained
workforce will become an increasingly important factor in determining the
success of RCHEs in combating infectious diseases, especially as the
number of elderly residents with special care needs (such as those with
indwelling urinary catheters or on nasogastric feeding) is rising.
Manpower planning, development, and staff retention will remain a
challenge for infection control.
Moreover, as knowledge and skills on infection
control have stopped improving, training on infection control should
emphasise encouraging sustainability of vigilant practices. Measures
including self-auditing on infection control should be considered, to
encourage RCHE staff to monitor their own infection control performance on
a regular basis, between annual external assessments.
Conclusion
This is the first territory-wide report on trends
in infection control performance in RCHEs in Hong Kong. Data collected
enabled us to understand the strengths and limitations in RCHEs on
infection control, thus allowing stakeholders to design more targeted
infection control training programmes.
Knowledge and skills on infection control have
reached an adequate level and remained stable. Future infection control
training should aim to support sustained compliance with proper practice,
through introduction of elements such as self-audits.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design: GCY Wong, T Ng, T Li.
Acquisition of data: GCY Wong.
Analysis or interpretation of data: GCY Wong.
Drafting of the article: GCY Wong.
Critical revision for important intellectual content: T Ng, T Li.
Acquisition of data: GCY Wong.
Analysis or interpretation of data: GCY Wong.
Drafting of the article: GCY Wong.
Critical revision for important intellectual content: T Ng, T Li.
Conflicts of interest
The authors have disclosed no conflict of interest.
Funding/support
The report was funded by the Department of Health,
Hong Kong.
Ethics approval
A waiver for ethical review was endorsed by the
Ethics Committee of the Department of Health, Hong Kong.
References
1. Census and Statistics Department, Hong
Kong SAR Government. 2016 Population By-census. Thematic report: older
persons. Available from:
https://www.bycensus2016.gov.hk/data/16BC_Older_persons_report.pdf.
Accessed 8 Jan 2019.
2. Social Welfare Department, Hong Kong SAR
Government. Code of practice for residential care homes (elderly persons).
Available from:
http://www.swd.gov.hk/doc/LORCHE/CodeofPractice_E_201303_20150313R3.pdf.
Accessed 8 Jan 2019.
3. Department of Health, Hong Kong SAR
Government. Guidelines on prevention of communicable diseases in
residential care home for the elderly (3rd edition). Available from:
https://www.chp.gov.hk/files/pdf/guidelines_on_prevention_of_communicable_diseases_in_rche_eng.pdf.
Accessed 8 Jan 2019.
4. Social Welfare Department, Hong Kong SAR
Government. List of residential care homes. Available from:
https://www.swd.gov.hk/en/index/site_pubsvc/page_elderly/sub_residentia/id_listofresi/.
Accessed 8 Jan 2019.
5. World Health Organization. WHO
guidelines on hand hygiene in health care. Available from:
http://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf?sequence=1.
Accessed 8 Jan 2019.
6. Audit tools for monitoring infection
control guidelines within the community setting. Bathgate, UK: Infection
Control Nurses Association; 2005.
7. Routine practices and additional
precautions in all health care settings. Canada: Provincial Infectious
Diseases Advisory Committee. Ministry of Health and Long-Term Care; 2009.
8. von Elm E, Altman DG, Egger M, Pocock
SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The strengthening
the reporting of observational studies in epidemiology (STROBE) statement:
guidelines for reporting observational studies. PLoS Med 2007;4:e296. Crossref
9. Social Welfare Department, Hong Kong SAR
Government. SWD elderly information website. Type of residential care
homes. Available from:
https://www.elderlyinfo.swd.gov.hk/en/rches_natures.html. Accessed 8 Jan
2019.
10. Büla CJ, Ghilardi G, Wietlisbach V,
Petignat C, Francioli P. Infections and functional impairment in nursing
home residents: a reciprocal relationship. J Am Geriatr Soc 2004;52:700-6.
Crossref
11. Castle NG, Engberg J. The influence of
staffing characteristics on quality of care in nursing homes. Health Serv
Res 2007;42:1822-47. Crossref
12. Bostick JE, Rantz MJ, Flesner MK,
Riggs CJ. Systematic review of studies of staffing and quality in nursing
homes. J Am Med Dir Assoc 2006;7:366-76. Crossref
13. Bowers BJ, Esmond S, Jacobson N. The
relationship between staffing and quality in long-term care: exploring the
views of nurse aides. J Nurs Care Qual 2000;14:55-64. Crossref
14. Hong Kong SAR Government’s response to
a question raised by a Legislative Councillor on 11 January 2017.
Available from:
https://www.info.gov.hk/gia/general/201701/11/P2017011100501.htm. Accessed
28 Jan 2019.
15. Research Brief Issue No. 1 2015-2016,
Research Office, Legislative Council Secretariat, Hong Kong. Available
from:
https://www.legco.gov.hk/research-publications/english/1516rb01-challenges-of-population-ageing-20151215-e.pdf.
Accessed 8 Jan 2019.
16. Petticrew M, Semple S, Hilton S, et
al. Covert observation in practice: Lessons from the evaluation of the
prohibition of smoking in public places in Scotland. BMC Public Health
2007;7:204. Crossref



 A video clip illustrating totally
laparoscopic subtotal gastrectomy for a patient with gastric cancer is available at
A video clip illustrating totally
laparoscopic subtotal gastrectomy for a patient with gastric cancer is available at