Hong
Kong Med J 2018 Aug;24(4):361–8 | Epub 30 Jul 2018
DOI: 10.12809/hkmj177081
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Delayed diagnosis of tuberculosis: risk factors and
effect on mortality among older adults in Hong Kong
Eric CC Leung, MB, BS, FHKAM (Medicine)1;
CC Leung, MB, BS, FHKAM (Medicine)1; KC Chang, MB, BS, FHKAM
(Medicine)1; CK Chan, MB, BS, FHKAM (Medicine)1;
Thomas YW Mok, MB, BS, FHKAM (Medicine)2; KS Chan, MB, BS,
FHKAM (Medicine)3; KS Lau, MB, BS, FHKAM (Medicine)4;
CH Chau, MB, BS, FHKAM (Medicine)5; Wilson KS Yee, MB, ChB,
FHKAM (Medicine)6; WS Law, MB, ChB, FHKAM (Medicine)1;
SN Lee, MB, ChB, FHKAM (Medicine)1; KF Au, MB, ChB, MRCP (UK)1;
LB Tai, MB, ChB, FHKAM (Medicine)1; WM Leung, MB, ChB, FHKAM
(Medicine)1
1 Tuberculosis and Chest Service, Centre
for Health Protection, Department of Health, Hong Kong
2 Respiratory Medicine Department,
Kowloon Hospital, Homantin, Hong Kong
3 Pulmonary Service, Department of
Medicine, Haven of Hope Hospital, Tseung Kwan O, Hong Kong
4 Respiratory Medicine Department,
Ruttonjee Hospital, Wanchai, Hong Kong
5 Tuberculosis and Chest Unit, Grantham
Hospital, Wong Chuk Hang, Hong Kong
6 Department of Medicine and Geriatrics,
Kwong Wah Hospital, Hong Kong
Corresponding author: Dr Eric CC Leung (eric_leung@dh.gov.hk)
Abstract
Objective: To assess the risk
factors and effects of delayed diagnosis on tuberculosis (TB) mortality
in Hong Kong.
Methods: All consecutive
patients with TB notified in 2010 were tracked through their clinical
records for treatment outcome until 2012. All TB cases notified or
confirmed after death were identified for a mortality survey on the
timing and causes of death.
Results: Of 5092 TB cases
notified, 1061 (20.9%) died within 2 years of notification; 211 (4.1%)
patients died before notification, 683 (13.4%) died within the first
year, and 167 (3.3%) died within the second year after notification.
Among the 211 cases with TB notified after death, only 30 were certified
to have died from TB. However, 52 (24.6%) died from unspecified
pneumonia/sepsis possibly related to pulmonary TB. If these cases are
counted, the total TB-related deaths increases from 191 to 243. In 82
(33.7%) of these, TB was notified after death. Over 60% of cases in
which TB was diagnosed after death involved patients aged ≥80 years and a
similar proportion had an advance care directive against resuscitation
or investigation. Independent factors for TB notified after death
included female sex, living in an old age home, drug abuse, malignancy
other than lung cancer, sputum TB smear negative, sputum TB culture
positive, and chest X-ray not done.
Conclusions: High mortality was
observed among patients with TB aged ≥80 years. Increased vigilance is
warranted to avoid delayed diagnosis and reduce the
transmission risk, especially among elderly patients with co-morbidities
living in old age homes.
New knowledge added by this study
- Mortality among elderly patients with tuberculosis (TB) in Hong Kong is high.
- There is a risk of institutional TB transmission because a substantial portion (42%) of these elderly people live in old age homes.
- Timely diagnosis and treatment of TB is necessary to avert adverse outcomes and prevent transmission.
- Increased vigilance and deployment of rapid diagnostic tools are necessary to facilitate early diagnosis of TB and to reduce the TB transmission risk, especially among elderly patients with co-morbidities living in old age homes.
Introduction
Over the past 30 years, the proportion of the Hong
Kong population aged ≥65 years doubled from 6.6% in 1981 to 13.3% in 2011.1 The proportion of those aged ≥65
years among patients with tuberculosis (TB) tripled from 13%2 to 39%3 in the
same period. Although the annual notification rate decreased from 149.1 to
65 per 100 000 population and the TB mortality rate decreased from 9.4 to
2.6 per 100 000 population from 1981 to 2011, the proportion of those aged
≥65 years increased from 53% to 82% among TB deaths.2 3 In older
adults, TB is associated with other co-morbidities, hospitalisation, and
delays in presentation and commencement of treatment.4 Missed opportunities for intervention might contribute
to the higher mortality rates in older adults, and might also increase the
risk of TB transmission. The present longitudinal study was conducted to
assess the effects of age on the mortality rates of patients with TB and
to elucidate the factors associated with missed TB diagnosis.
Methods
All consecutive cases of TB notified to the
Department of Health in 2010 were retrospectively collected from the
statutory TB notification registry. Hong Kong identity card numbers (or
passport numbers for non-residents) were retrieved from the notification
registry, together with date of notification, source of notification, and
demographic and clinical information. Further clinical information and
outcome data at 1 year after notification/initiation of treatment were
retrieved from the TB programme record forms.3
These forms are filed by the TB and Chest Service for patients managed
under its chest clinics and for patients managed by other health care
providers. Treatment outcome was classified according to the World Health
Organization (WHO) recommendations.5
Using the identity card number/passport number as the unique identifier,
the 2010 TB cohort data were cross-matched with the statutory death
registry from 1 January 2009 till 31 December 2012 for vital status, date
and cause(s) of death. All cases with a date of TB notification after the
date of death were recorded. A mortality survey was conducted on these
recorded cases by retrieving relevant clinical information from records in
public clinics and hospitals.
The demographics, co-morbidities, treatment
outcomes, and mortality pattern of the cohort were analysed. Published
data on patients of all ages with TB6
and on elderly patients with TB7
notified in 1996 were used for comparison. A date of TB notification after
the date of death was considered as a surrogate marker of delayed
diagnosis. Categorical variables were analysed by Pearson χ2
test or Fisher’s exact test as appropriate; continuous variables were
analysed by Mann-Whitney U test. Binary regression modelling was
used to calculate the adjusted odds ratios (aORs) for risk factors for
delayed diagnosis of TB after death using a backward conditional approach,
with probability to remove being 0.10 and to retain being 0.05. A
two-tailed P<0.05 was considered statistically significant. Statistical
analyses were performed using SPSS for Windows, version 16.0 (SPSS Inc,
Chicago [IL], US).
Results
After exclusion of 336 cases subsequently
denotified because of alternative diagnoses, a total of 5092 patients with
TB were included in the 2010 TB cohort, at a notification rate of 72.5/100
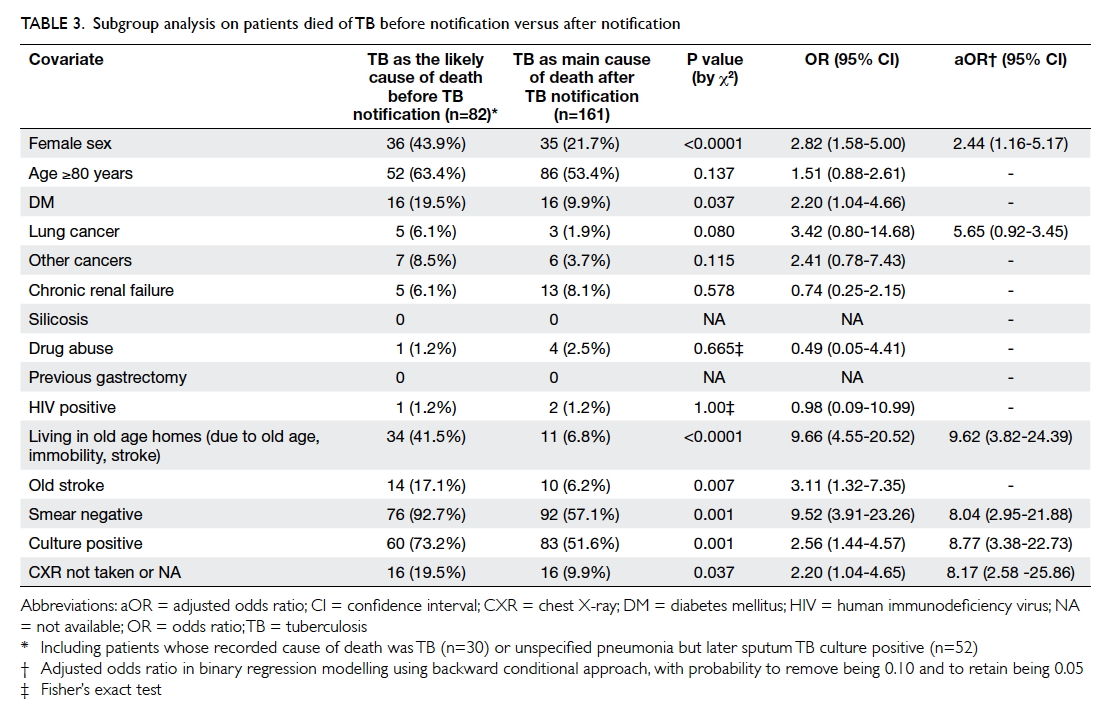
000 person-years. Table 1 summarises their demographic data, clinical
characteristics, and 1-year outcomes. Comparison with published data on
the 1996 TB cohort6 7 was restricted to patients managed under the TB and
Chest Service, for which the proportion of patients with TB aged ≥60 years
increased from 34.5% in 1996 to 42.9% in 2010. There were more
co-morbidities such as diabetes mellitus (16.0% vs 9.6%), lung cancer
(2.1% vs 1.1%), and other cancers (5.0% vs 0.6%) in the 2010 TB cohort
than in the 1996 TB cohort (χ2 test, P<0.001). In 2010, the
proportion of patients who died before completion of TB treatment was
smaller for those managed under the TB and Chest Service (7.4%) than for
the overall cohort (16.2%). However, the proportion of patients managed
under the TB and Chest Service who died before completion of TB treatment
nearly doubled between 1996 (3.9%) and 2010 (7.4%).
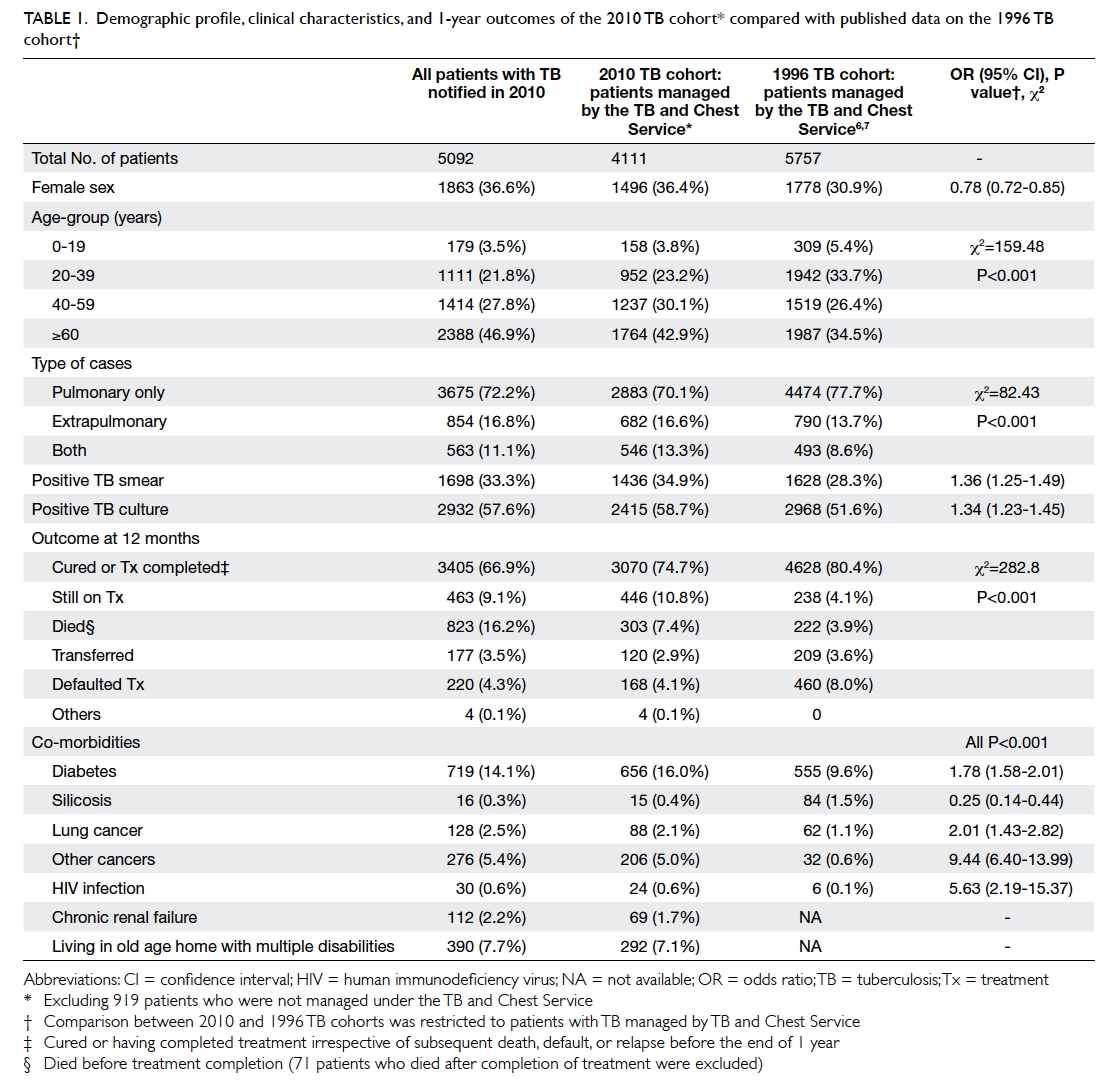
Table 1. Demographic profile, clinical characteristics, and 1-year outcomes of the 2010 TB cohort compared with published data on the 1996 TB cohort
Among 5092 TB notifications, 1061 (20.9%) deaths
occurred within 2 years of notification. Of the 1061 deaths, 211 (4.1%)
occurred before the TB notification (ie, TB was notified after death;
median delay in notification [interval between death and TB notification]
45 days, interquartile range 30-65 days). Of the deaths after
notification, 683 (13.4%) died in the first year and 167 (3.3%) died in
the second year. The reported causes of death were related to TB in only
191 (18.0%) of all deaths; 30 (14.2%) before TB notification, 158 (23.1%)
in the first year, and three (1.8%) in the second year after notification.
Among the 211 deaths before TB notification, only
30 (14.2%) had TB as the main cause of death. There were 54 cases of
‘pneumonia unspecified’ and three cases of ‘sepsis unspecified’ reported
as main cause of death. Of these cases, only five with potential causative
organisms, such as Pseudomonas, Acinetobacter, or Escherichia coli,
were identified. However, in the sputum that had been collected before
death in these patients, Mycobacterium tuberculosis was
subsequently isolated after prolonged culture, indicating that TB was the
likely main cause of death in the remaining 52 deaths initially reported
as ‘sepsis or pneumonia unspecified’. Including these revised results
increases the 2010 TB-related mortality from 191 to 243, ie, an increase
of 27% from the officially reported mortality figures of 2.6 to 3.4 per
100 000 person-years.8 The
corresponding proportion of TB-related mortality increases to 38.8%
(82/211) in cases with TB notified after death compared with 23.3%
(158/683) who died in the first year after notification and 1.7% (3/167)
who died in the second year. Therefore, a substantial proportion (15.5%)
of TB-related deaths could potentially have been prevented by early
diagnosis and treatment.
For the 211 deaths before TB notification, 25 cases
of TB were notified from the public mortuary. Of the remaining 186 cases
of TB that were notified from hospital, 173 hospital records were
collected; 13 cases had missing data. None of the 198 patients with
retrievable records were started on treatment. Of these 198 patients, 119
(60.1%) were aged ≥80 years at the time of death, and 93 (47%) had more
than one admission to hospital before death. Prior to death, of these 198
patients, 83 (41.9%) were living in an old age home (OAH), 78 (39.4%) were
bed-ridden, and 121 (61.1%) had an advance care directive such as ‘do not
resuscitate’ or ‘do not investigate’ stated in the case notes. Table
2 summarises the univariate and multiple logistic regression
analyses of these 198 early deaths, using deaths occurring within 1 year
after notification as controls. Female sex, having a malignancy other than
lung cancer, living in an OAH, drug abuser, sputum TB smear negative,
sputum TB culture positive, and chest X-ray (CXR) not done or not
available were independent risk factors for death before TB diagnosis.
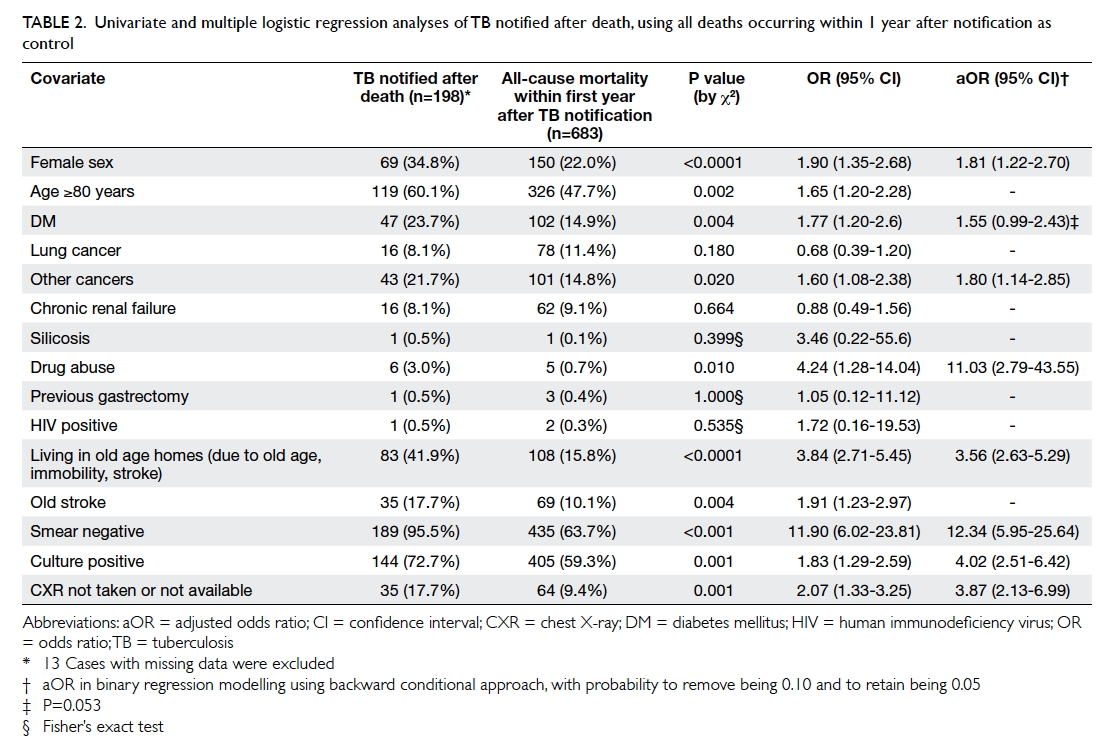
Table 2. Univariate and multiple logistic regression analyses of TB notified after death, using all deaths occurring within 1 year after notification as control
Subgroup analysis was carried out for patients that
most likely died of TB. The study group included the 30 patients who died
of TB before diagnosis and the 52 patients whose deaths were initially
reported as ‘sepsis or pneumonia unspecified’ but later sputum TB culture
was positive. The control group was all patients who died of TB after
notification (Table 3). Female sex, living in an OAH, sputum TB
smear negative, sputum TB culture positive, and CXR not done or not
available were independent risk factors for this group.
Discussion
In the present study, the proportion of patients
with TB aged ≥60 years increased by 25% from 1996 to 2010. However, over
the same interval, the proportion of patients who had died before
completion of treatment nearly doubled (Table 1). A substantial proportion (211 of 1061;
19.9%) of the TB-related deaths were notified after death. Over 60% of
these cases were aged ≥80 years and none were started on treatment,
suggesting a failure to detect TB rather than just a delay in
notification. Over 60% of them had an advance care directive against
resuscitation or investigation, likely indicating a concurrent terminal
illness. Independent factors associated with TB notified after death were
female sex, malignancies other than lung cancer, living in an OAH, drug
abuse, sputum TB smear negative, sputum TB culture positive, and CXR not
done. Although the recorded cause of death was TB in only 30 (14%) cases,
in 52 (25%) cases the recorded cause of death was respiratory disease
(predominantly pneumonia unspecified), particularly among those aged ≥80
years (19% vs 39%; P<0.005). In these cases, pulmonary TB is likely to
have been the main or precipitating cause.
In the present study, the fatality rate in the
first year of TB notification was 17.5% (4.1% died before TB notification
and 13.4% died within 1 year after TB notification). This is much higher
than rates reported earlier in Europe (7.8%9)
and England and Wales (8.4%10),
but similar to rates reported more recently in Taiwan (16.5%11). This is probably a reflection of differences among
patient profiles in these regions, especially age and the associated
co-morbidities. In the present study, 47% of patients with TB were aged
≥60 years (Table 1), whereas in the studies in Europe and the
United Kingdom only 24.3%9 and 17.9%10 of the patients with TB were cohort
aged ≥60 years.
Our finding that 4.1% of TB cases were notified
after death is similar to rates reported in Taiwan in 2006 (4.0%12) and in the US in the 1980s (5.1%13 and 3.9%14).
In all of these reports, advanced age was a consistent observation for
this extreme form of delayed diagnosis. As expected from the relatively
short turnover time for sputum TB smear tests and CXRs, sputum TB smear
negative, and CXR unknown or not done were important risk factors for TB
notified after death. The strong association between these cases and
positive sputum TB culture might be explained by the fact that the sputum
TB culture was the primary method of TB diagnosis, unless a diagnosis had
already been made during autopsy.
Our findings that drug abusers have a higher chance
of TB notification after death is in line with an earlier study that
suggested such patients have difficulty completing medical evaluations.15 Drug abusers might be less aware
of their TB symptoms because of the effects of the drugs taken, such as
opiate suppression of the cough reflex.
Female sex was also an independent factor in the
current study, similar to a previous study in Taiwan.11 This is expected, because there is a higher
proportion of women among the geriatric population16 and among residents of OAH17
owing to their longer life expectancy and because conservative treatment
is more frequently selected by these elderly female patients or their
guardians. Patients with terminal conditions might have an advance care
directive against resuscitation or investigation. An incorrect provisional
diagnosis might also result from the readiness to accept a diagnosis of
advanced disseminated malignancy in a patient with such an advance care
directive. As lung cancer patients usually had CXR and sputum samples
taken in their initial diagnostic investigation, coexisting TB could be
discovered early. In addition, most lung cancer patients were diagnosed at
an advanced stage and usually died within the first year after
presentation.18
In our study, TB-related death occurred shortly
before or after TB treatment was started, in line with findings from
studies in Taiwan,19 the US,20 and Russia21
reporting a median time of 3 to 7 weeks from diagnosis or notification of
TB to death. A study in Canada showed that a delay in TB treatment
increased risk of death (aOR=3.3; 95% confidence interval=1.7-6.2) and
intensive care unit admission (aOR=16.8; 95% confidence interval=2-144).22 Another study of hospitalised
patients with TB also showed that late TB treatment guided by conventional
TB culture was associated with a higher mortality than for treatment
guided by polymerase chain reaction (PCR), liquid culture, positive
histological findings or typical clinico-radiological manifestation.23 In settings with a high human immunodeficiency virus
prevalence, the WHO advocates early empirical TB treatment based on
clinical and radiological criteria in patients strongly suspected as
having TB but with sputum TB smear negative, because this can improve
survival.24 25
Although a timely diagnosis might not avert most
non–TB-related deaths, early treatment could reduce the institutional
transmission risk, because 42% of patients with TB were living in OAHs in
the current study. The prevalence of active TB in OAHs has been estimated
to be as high as 669 per 100 000 person-years in Hong Kong.26 The majority of patients in the present study did not
have a positive sputum TB smear; however, a representative sputum sample
might have been difficult to obtain from patients living in OAHs. That 73%
of these patients had a positive sputum TB culture suggests that there was
a sufficient degree of suspicion, either clinical or radiological, for
initiation of bacteriological sampling. In total, 54 out of 211 patients
who died before TB notification were recorded to have ‘pneumonia
unspecified’ or ‘respiratory disease’ as the main cause of death. Past
studies have shown that negative TB smear contributed to around 17% of TB
transmission in San Francisco27
and Vancouver28 and even 30% in
China.29 Thus, rapid diagnosis
with effective isolation and early treatment can reduce transmission and
even mortality. Sputum induction30
or gastric aspiration31 would
improve specimen collection. However, in view of the infection risk, these
bio-aerosol generating procedures would preferentially be performed in a
negative pressure room with effective personal protective equipment as
stipulated by the Institutional Infection Control Guidelines. Real-time
PCR diagnostic tests such as Xpert® MTB/RIF assay32
may also be valuable, either as a primary diagnostic test or as an add-on
test in patients previously found to be TB smear negative, to avoid the
long turnover time for bacteriological cultures. In a study in Hong Kong,33 Xpert® MTB/ RIF assay was found
to be a highly cost-effective strategy for TB diagnosis in terms of
quality-adjusted life-years gained and lower first year mortality rate.
Higher mortality among patients with TB aged ≥80
years is a consistent finding among different TB programmes.34 The present study also found frequently missed
diagnosis of TB and excessive mortality among patients aged ≥80 years who
were frequently institutionalised and had multiple co-morbidities. A high
index of suspicion and rapid diagnostic tools are necessary to reduce both
mortality and transmission risk in a rapidly ageing population, in order
to meet the WHO End TB 2035 target of a 95% reduction in TB mortality rate
compared with the 2015 rate.35
This study shares an important limitation with
other retrospective studies. The clinical data in this cohort were
constructed from a database of the pre-assembled ‘TB programme record
form’ which was not specifically designed for this study. Therefore, not
all pertinent risk factors were identified and recorded. As this is a
population-wide database, many health care professionals were involved and
the measurement of risk factors and outcomes is less accurate and less
consistent than a prospective study. Nonetheless, data from the TB
programme record form have been used in previous studies on patients with
TB6 and elderly patients with TB7 and were included for comparison in this
study.
Conclusions
This study was a collaborative effort between the
Hospital Authority and the Department of Health, and a database was
compiled for all patients with TB treated in the public or the private
sector. This study provides insight into the mortality of patients with TB
and the risk factors associated with a delay in TB diagnosis. These
factors include novel patient factors such as female sex, living in OAHs,
advance care directives refusing further investigation or resuscitation,
and drug abuse. Additional factors include lack of a representative sputum
sample. which could be mitigated by sputum induction or gastric
aspiration, and the relative insensitivity of sputum TB smear and long
turnover time for conventional TB culture, which could be mitigated by
using of real-time PCR tests. Information generated by this study will
help frontline clinicians to be better aware of this important infectious
disease among elderly people. Hopefully, more resources will be allocated
to promote rapid diagnosis of TB for patients in high-risk scenarios in
Hong Kong.
Acknowledgement
The authors would likely to thank the Nursing and
General Grade staff in Department of Health and Hospital Authority for
their assistance in collection and compilation of the demographical,
clinical and laboratory data for this study.
Author contributions
Concept or design: ECC Leung, CC Leung, CK Chan, KC
Chang.
Acquisition of data: TYW Mok, KS Chan, KS Lau, CH Chau, WKS Yee, WM Leung, KF Au.
Analysis or interpretation of data: WS Law, SN Lee, LB Tai.
Drafting of the article: ECC Leung, CC Leung, WM Leung, WS Law.
Critical revision for important intellectual content: All authors.
Acquisition of data: TYW Mok, KS Chan, KS Lau, CH Chau, WKS Yee, WM Leung, KF Au.
Analysis or interpretation of data: WS Law, SN Lee, LB Tai.
Drafting of the article: ECC Leung, CC Leung, WM Leung, WS Law.
Critical revision for important intellectual content: All authors.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Declaration
The authors have no conflicts of interest to
disclose.
Ethical approval
This study was approved by the Ethics Committee of
the Department of Health and Ethics Committees of all hospital clusters
from the Hospital Authority.
References
1. Demographic Statistics Section, Census
and Statistics Department, Hong Kong SAR Government. Demographic Trends in
Hong Kong 1981-2011. Available from:
https://www.statistics.gov.hk/pub/B1120017032012XXXXB0100.pdf Accessed 13
Jul 2018. Crossref
2. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual Report 1981. Hong
Kong: Department of Health, Hong Kong SAR Government; 1981. Crossref
3. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual Report 2011.
Available from: http://www.info.gov.hk/tb_chest/doc/AnnualReport2011.pdf.
Accessed 14 Jul 2018. Crossref
4. Leung CC, Yew WW, Chan CK, et al.
Tuberculosis in older people: a retrospective and comparative study from
Hong Kong. J Am Geriatr Soc 2002;50:1219-26. Crossref
5. World Health Organization. Definitions
and reporting framework for tuberculosis—2013 revision. Geneva,
Switzerland: World Health Organization; 2013. Crossref
6. Tam CM, Leung CC, Noertjojo K, Chan SL,
Chan-Yeung M. Tuberculosis in Hong Kong-patient characteristics and
treatment outcome. Hong Kong Med J 2003;9:83-90.
7. Chan-Yeung M, Noertjojo K, Tan J, Chan
SL, Tam CM. Tuberculosis in the elderly in Hong Kong. Int J Tuberc Lung
Dis 2002;6:771-9.
8. Centre for Health Protection, Department
of Health, Hong Kong SAR Government. Notification & death rate of
tuberculosis (all forms), 1947-2017. Available from:
https://www.chp.gov.hk/en/statistics/data/10/26/43/88.html. Accessed 20
Jul 2018. Crossref
9. Lefebvre N, Falzon D. Risk factors for
death among tuberculosis cases: analysis of European surveillance data.
Eur Respir J 2008;31:1256-60. Crossref
10. Crofts JP, Pebody R, Grant A, Watson
JM, Abubakar I. Estimating tuberculosis case mortality in England and
Wales, 2001-2002. Int J Tuberc Lung Dis 2008;12:308-13.
11. Wu YC, Lo HY, Yang SL, Chu DC, Chou P.
Comparing the factors correlated with tuberculosis-specific and
non-tuberculosis-specific deaths in different age groups among
tuberculosis-related deaths in Taiwan. PLoS ONE 2015;10:e0118929. Crossref
12. Wu YC, Lo HY, Yang SL, Chou P. Factors
correlated with tuberculosis reported after death. Int J Tuberc Lung Dis
2014;18:1485-90. Crossref
13. Rieder HL, Kelly GD, Bloch AB, Cauthen
GM, Snider DE Jr. Tuberculosis diagnosed at death in the United States.
Chest 1991;100:678-81. Crossref
14. DeRiemer K, Rudoy I, Schecter GF,
Hopewell PC, Daley CL. The epidemiology of tuberculosis diagnosed after
death in San Francisco, 1986-1995. Int J Tuberc Lung Dis 1999;3:488-93.
15. Deiss RG, Rodwell TC, Garfein RS.
Tuberculosis and illicit drug use: review and update. Clin Infect Dis
2009;48:72-82. Crossref
16. Census and Statistics Department, Hong
Kong SAR Government. Population by Age Group and Sex. Hong Kong Population
By-Census Main Report. 2015. Available from:
http://www.censtatd.gov.hk/hong_kong_statistics/statistical_tables/index.jsp?charsetID=1<tableID=002.
Accessed 16 Mar 2016.
17. Luk JK, Chan FH, Pau MM, Yu C.
Outreach geriatric service to private old age homes in Hong Kong West
Clusters. J HK Geriatr Soc 2002;11:5-11.
18. Cancer Research UK. Lung cancer
survival statistics. Available from:
http://www.cancerresearchuk.org/healthprofessional/cancer-statistics/statistics-by-cancer-type/lung-cancer/survival.
Accessed 15 Mar 2016. Crossref
19. Lin CH, Lin CJ, Kuo YW, et al.
Tuberculosis mortality: patient characteristics and causes. BMC Infect Dis
2014;14:5. Crossref
20. Oursler KK, Moore RD, Bishai WR,
Harrington SM, Pope DS, Chaisson RE. Survival of patients with pulmonary
tuberculosis: clinical and molecular epidemiologic factors. Clin Infect
Dis 2002;34:752-9. Crossref
21. Mathew TA, Ovsyanikova TN, Shin SS, et
al. Causes of death during tuberculosis treatment in Tomsk Oblast Russia.
Int J Tuberc Lung Dis 2006;10:857-63.
22. Greenaway C, Menzies D, Fanning A, et
al. Delay in diagnosis among hospitalized patients with active
tuberculosis—predictors and outcomes. Am J Respir Crit Care Med
2002;165:927-33. Crossref
23. Lui G, Wong RY, Li F, et al. High
mortality in adults hospitalized for active tuberculosis in a low HIV
prevalence setting. PLoS One 2014;9:e92077. Crossref
24. Holtz TH, Kabera G, Mthiyane T, et al.
Use of a WHO-recommended algorithm to reduce mortality in seriously ill
patients with HIV infection and smear-negative pulmonary tuberculosis in
South Africa: an observational cohort study. Lancet Infect Dis
2011;11:533-40. Crossref
25. Katagira W, Walter ND, Den Boon S, et
al. Empiric TB treatment of severely ill patients with HIV and presumed
pulmonary TB improves survival. J Acquir Immune Defic Syndr
2016;72:297-303. Crossref
26. Chan-Yeung M, Chan FH, Cheung AH, et
al. Prevalence of tuberculous infection and active tuberculosis in old age
homes in Hong Kong. J Am Geriatr Soc 2006;54:1334-40. Crossref
27. Behr MA, Warren SA, Salamon H, et al.
Transmission of Mycobacterium tuberculosis from patients
smear-negative for acid-fast bacilli. Lancet 1999;353:444-9. Crossref
28. Hernández-Garduño E, Cook V, Kunimoto
D, Elwood RK, Black WA, FitzGerald JM. Transmission of tuberculosis from
smear negative patients: a molecular epidemiology study. Thorax
2004;59:286-90. Crossref
29. Yang C, Shen X, Peng Y, et al.
Transmission of Mycobacterium tuberculosis in China; a
population-based molecular epidemiologic study. Clin Infect Dis
2015;61:219-27. Crossref
30. Chang KC, Leung CC, Yew WW, Tam CM.
Supervised and induced sputum among patients with smear-negative pulmonary
tuberculosis. Eur Respir J 2008;31:1085-90. Crossref
31. Brown M, Varia H, Bassett P, Davidson
RN, Wall R, Pasvol G. Prospective study of sputum induction, gastric
washing, and bronchoalveolar lavage for the diagnosis of pulmonary
tuberculosis in patients who are unable to expectorate. Clin Infect Dis
2007;44:1415-20. Crossref
32. Steingart KR, Schiller I, Horne DJ,
Pai M, Boehme CC, Dendukuri N. Xpert® MTB/RIF assay for pulmonary
tuberculosis and rifampicin resistance in adults. Cochrane Database Syst
Rev 2014;(1):CD009593. Crossref
33. You JH, Lui G, Kam KM, Lee NL.
Cost-effectiveness analysis of the Xpert MTB/RIF assay for rapid diagnosis
of suspected tuberculosis in an intermediate burden area. J Infect
2015;70:409-14. Crossref
34. Waitt CJ, Squire SB. A systematic
review of risk factors for death in adults during and after tuberculosis
treatment. Int J Tuberc Lung Dis 2011;15:871-85. Crossref
35. World Health Organization.
Implementing the end TB strategy: the essentials. Available from:
http://www.who.int/tb/publications/2015/The_Essentials_to_End_TB/en/.Accessed
3 May 2017. Crossref