Hong
Kong Med J 2018 Oct;24(5):484–91 | Epub 28 Sep 2018
DOI: 10.12809/hkmj177135
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Prehospital 12-lead electrocardiogram for
patients with chest pain: a pilot study
KS Cheung, FHKCEM, MSc Cardiology1;
LP Leung, FHKCEM2;
YC Siu, FHKCEM3;
TC Tsang, FHKCEM1;
Matthew SH Tsui, FRCP (Edin), FHKAM (Emergency Medicine)1;
CC Tam, FHKCP, FHKAM (Medicine)4;
Raymond HW Chan, FHKAM (Medicine)5
1 Department of Accident and Emergency, Queen Mary Hospital,
Pokfulam, Hong Kong
2 Emergency Medicine Unit, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
3 Medical Director, Fire and Ambulance Services Academy, Hong Kong Fire Services Department, Hong Kong
4 Department of Medicine, Queen Mary Hospital, Pokfulam, Hong Kong
5 Honorary Consultant Cardiologist, Hong Kong Sanatorium Hospital, Happy Valley, Hong Kong
2 Emergency Medicine Unit, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
3 Medical Director, Fire and Ambulance Services Academy, Hong Kong Fire Services Department, Hong Kong
4 Department of Medicine, Queen Mary Hospital, Pokfulam, Hong Kong
5 Honorary Consultant Cardiologist, Hong Kong Sanatorium Hospital, Happy Valley, Hong Kong
Corresponding author: Dr KS Cheung (cks373@ha.org.hk)
Abstract
Introduction: After ST-segment elevation
myocardial infarction (STEMI), it is vital to shorten
reperfusion time. This study examined data from a
pilot project to shorten the door-to-balloon (D2B)
time by using prehospital 12-lead electrocardiogram
(ECG).
Methods: Methods: Fifteen ambulances equipped with
X Series® Monitor/Defibrillator (Zoll Medical
Corporation) were deployed to the catchment
area of Queen Mary Hospital, Hong Kong, from
November 2015 to December 2016. For patients with
chest pain, prehospital 12-lead ECG was performed
and tele-transmitted to attending physicians at the
accident and emergency department for immediate
interpretation. The on-call cardiologist was called
before patient arrival if STEMI was suspected.
Data from this group of patients with STEMI were
compared with data from patients with STEMI who
were transported by ambulances without prehospital
ECG or by self-arranged transport.
Results: From 841 patients with chest pain, 731 gave
verbal consent and prehospital ECG was performed
and transmitted. Of these, 25 patients with clinically
diagnosed STEMI required emergency coronary
angiogram with or without primary percutaneous
coronary intervention. The mean D2B time for these
25 patients (93 minutes) was significantly shorter
(P=0.003) than that for 58 patients with STEMI
transported by ambulances without prehospital
ECG (112 minutes) and that for 41 patients with
STEMI with self-arranged transport (138 minutes).
However, shorter reperfusion time was only recorded
during daytime hours (08:00-17:59). No statistically
significant difference in 30-day mortality was found.
Conclusion: Prehospital ECG is technologically
feasible in Hong Kong and shortens the D2B time.
However, shorter reperfusion time was only recorded
during daytime hours.
New knowledge added by this study
- This pilot study investigated the feasibility and performance of prehospital 12-lead electrocardiogram (ECG) deployed in ambulances in Hong Kong.
- There was a statistically significant difference in door-to-balloon time when prehospital ECG was performed during daytime hours.
- There was no statistically significant difference in 30-day mortality related to the use of prehospital ECG.
- Based on the evidence of feasibility and shortening of door-to-balloon time in Hong Kong, prehospital ECG services might be supported by the Hong Kong Fire Services Department.
- Primary diversion of ST-elevation myocardial infarction may be implemented in Hong Kong in the future.
Introduction
In 1970, Nagel et al1 first reported the transmission
of single-lead electrocardiogram (ECG) data via
radio system to hospital physicians in Florida, US,
for diagnostic purposes. To date, prehospital 12-lead
ECG programmes have been implemented in various
countries. In 2015, the American Heart Association
Guidelines for Cardiopulmonary Resuscitation and
Emergency Cardiovascular Care recommended that
prehospital 12-lead ECG should be acquired early for
patients with possible acute coronary syndrome.2 The
acquisition and tele-transmission of ECG data to the
accident and emergency department (AED) allows
rapid diagnosis of ST-segment elevation myocardial
infarction (STEMI) by attending physicians. The
on-call cardiologist and cardiac catheterisation
laboratory (CCL) can then be notified early. This
significantly shortens the door-to-balloon (D2B)
time and improves patient outcome.3
The Hong Kong Fire Services Department
(HKFSD) is the major emergency ambulance service
provider in Hong Kong. Ambulances are deployed by
the Fire Service Control Centre after calls to 999 and
are manned by ambulance crew in accordance with
pre-set protocols approved by the Medical Director
of the HKFSD. Patients are transported to the nearest
public hospital based on their geographical location.
There is no choice with respect to the destination
hospital, and there was no primary diversion for
chest pain or STEMI in the project period.
Queen Mary Hospital (QMH) is a tertiary
care hospital providing 24-hour emergency medical
services in Hong Kong. Since November 2010, QMH
has been the only public hospital in Hong Kong
providing a 24-hour primary percutaneous coronary
intervention (PPCI) service for all patients with
STEMI.
In November 2015, the HKFSD and the
QMH AED jointly launched a pilot project named
‘Prehospital Ambulance 12-Lead Electrocardiogram
for Chest Pain Patients in Hong Kong West Cluster’.
The present paper reports on the results of the
first phase of that project. We hypothesised that
prehospital ECG would shorten the D2B time and
reduce mortality in patients with STEMI treated in
AEDs in Hong Kong.
Methods
The present retrospective observational study
analysed data from the ‘Prehospital Ambulance
12-Lead Electrocardiogram for Chest Pain Patients in
Hong Kong West Cluster’ pilot project. That project
began on 12 November 2015 and its first phase
ended on 31 December 2016. All 122 ambulance
crew members involved with the study received a
half-day theory and hands-on training by clinical
specialists of Zoll Medical Corporation (Chelmsford
[MA], US) regarding the performance of prehospital
12-lead ECG. During the project period, there were
20 HKFSD ambulances operating in the catchment
area of QMH; 10 were not operated during the night
shift. Of these 20 ambulances, 15 were equipped
with X Series® Monitor/Defibrillator (Zoll Medical
Corporation) with ECG and tele-transmission
functions. These 15 ambulances were deployed by
the HKFSD to Aberdeen Ambulance Depot, Pok Fu
Lam Ambulance Depot, Mount Davis Ambulance
Depot, and Sheung Wan Fire Station.
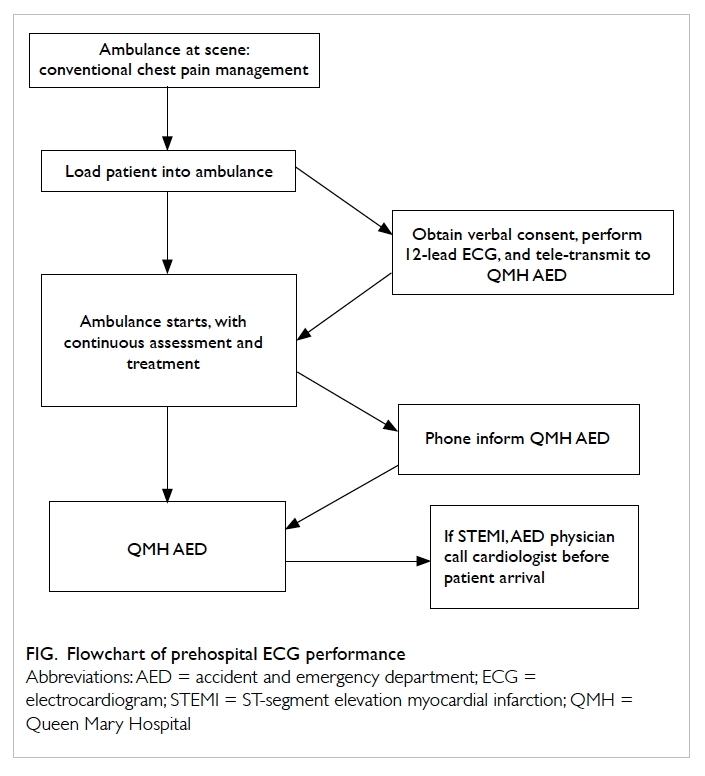
In addition to the conventional management
of chest pain or discomfort of cardiac origin,
ambulance crews performed prehospital ECG
(Fig). The ambulance crews were trained to use
a standardised script in Chinese or English to
explain the indication, procedure, benefit, and
risk of performing prehospital ECG. Patients and
accompanying relatives were provided with sufficient
time for questions before informed consent was
obtained. Patients were excluded if they were under
12 years of age; were in cardiac arrest; exhibited
airway or breathing that could not be managed; had
Glasgow Coma score ≤13; had first systolic blood
pressure <90 mm Hg; had respiratory rate <10 or
>29 breaths per minute; or were otherwise unable to
consent.
The prehospital ECG was obtained in the
ambulance compartment before its departure from
the scene and was immediately tele-transmitted to
the AED for interpretation by a physician. When a
new prehospital ECG was transmitted, staff at the
AED were notified via a dedicated laptop with alarm,
fax, and email, as well as an alert phone call from
the ambulance crew en route. The patient’s Hong
Kong Identity Card number was also conveyed
through the alert phone call from the ambulance.
This allowed early identification of any new changes
in the prehospital ECG, compared with previous
ECG data stored in the hospital clinical management
system record.
The most senior attending AED physician
available was responsible for reading and interpreting
the prehospital ECG. If the AED physician identified
ST-segment elevation in two or more contiguous
leads, the on-call cardiologist was paged and
AED manpower and equipment were arranged
immediately. Patients without such ST-segment
elevation were triaged by experienced AED nurses
upon arrival, in accordance with their overall clinical
condition.
To compare the characteristics and outcomes
of patients in this pilot project with those of other
patients with chest pain (ie, those attending the
AED by ambulance without prehospital ECG, or by
self-arranged transport), data from the cardiac care
unit of QMH were collected for comparison. Data
of all patients attending the AED with emergency
coronary angiography, with or without PPCI, were
analysed. The D2B or door-to-catheter (D2C) time
of different subgroups was determined and analysed
as the primary outcome of this study. Secondary
outcomes, including performance in daytime or
night-time AED registration, triage accuracy, and
30-day mortality, were assessed in further subgroup
analysis.
Results
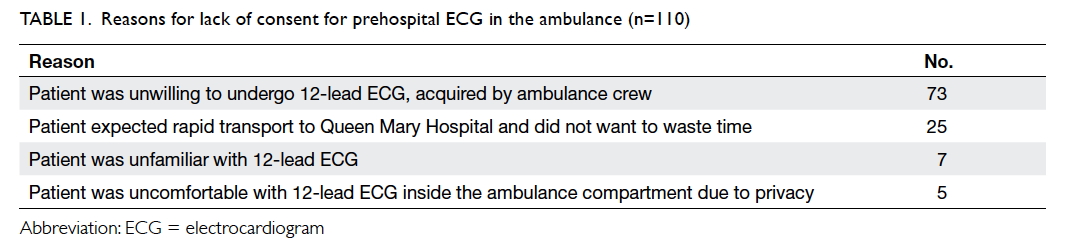
From 12 November 2015 to 31 December 2016,
ambulance crews equipped with X Series® attended
to 841 patients presenting with cardiac chest pain.
Verbal consent to perform prehospital ECG was
obtained from 731 (86.9%) patients and these were
included for analysis. A mean 1.76 prehospital ECGs
were successfully performed and transmitted per
day during the pilot project period. Reasons for not
performing prehospital ECG are shown in Table 1.
In total, 60% of patients were male. The patients’
mean age was 71 years, with a difference of 10 years
between male (mean, 67 years) and female (mean, 77
years) patients. More patients registered at the AED
during daytime hours (08:00-17:59; n=380 [52.0%])
than during night-time hours (18:00-07:59; n=351
[48.0%]). Most patients were triaged as category 3 in
the AED (n=577) [78.9%]; those triaged as category
1 (critical), 2 (emergency), 4 (semi-urgent), and 5
(non-urgent) were 39 (5.3%), 57 (7.8%), 58 (7.9%),
and 0, respectively.
In all, 93% of cases with cardiac chest pain
were managed by AED physicians without further
on-site consultation. Consultations with physicians
from the cardiac care unit were initiated by the AED
physician for 53 patients: 22 (41.5%) were performed
on or before patient arrival at the AED, whereas the
remaining 31 (58.5%) were conducted after patient
arrival.
Of the 731 patients who received pre-hospital
ECG, 534 (73.1%) patients were admitted to the
medical ward, 96 (13.1%) to the emergency medical
ward, 33 (4.5%) to the cardiac care unit, 13 (1.8%)
to the surgical ward, three (0.4%) to the intensive
care unit, and one (0.1%) to the neurosurgical ward
for further management of their symptoms. Of
the remaining patients, 39 (5.3%) were discharged
from the AED, eight (1.1%) were discharged against
medical advice, three (0.4%) disappeared, and one
(0.1%) was certified in the AED.
Of the 731 patients who received pre-hospital
ECG, 26 (3.6%) patients were clinically diagnosed
with STEMI by AED physicians. Coronary
angiogram, with or without PPCI, was arranged
immediately for 25 of these patients. The remaining
patient had a terminal malignancy and was offered
non-invasive treatment after discussion with the
patient’s family.
The mean D2B and D2C times were compared
among 124 patients with clinically diagnosed STEMI:
25 patients with STEMI treated with prehospital
ECGs; 58 patients with STEMI who were treated by
ambulance crews without prehospital ECGs; and 41
self-transported patients with STEMI treated in the
QMH AED during the pilot project period (Table 2).
A statistically significant difference was found in the
mean D2B time (P=0.003). Patients with prehospital
ECGs had the shortest mean D2B (93 minutes) and
D2C (71 minutes) times. Additionally, a greater
percentage of patients with prehospital 12-lead ECG
had D2B or D2C time ≤90 minutes.
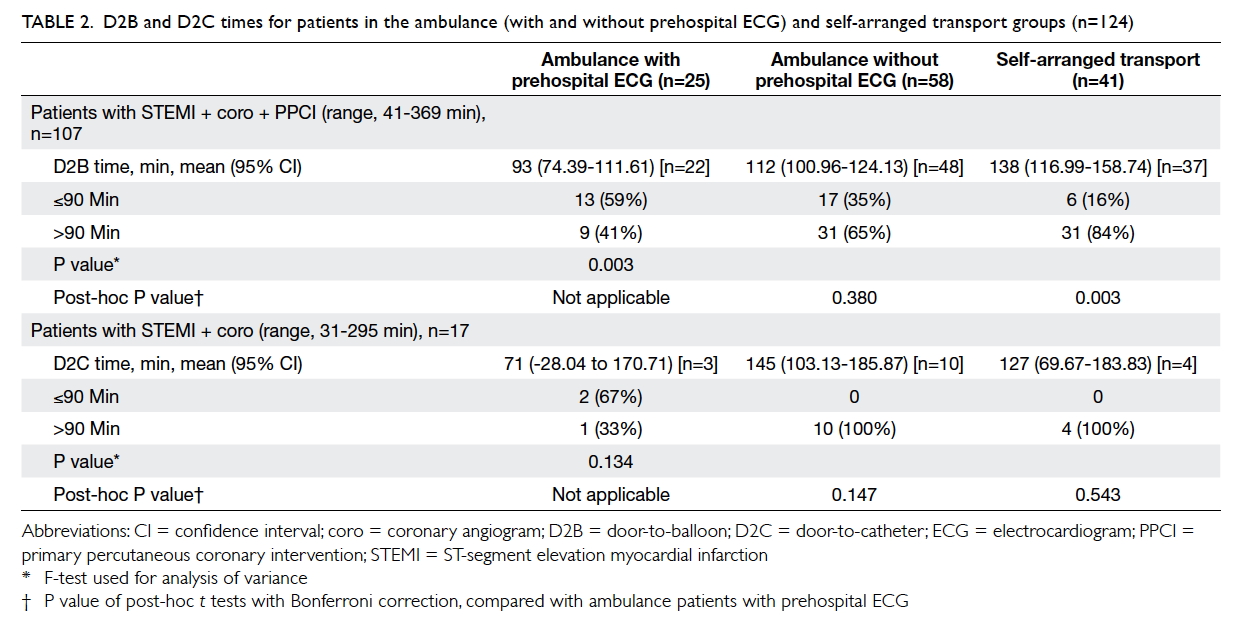
Table 2. D2B and D2C times for patients in the ambulance (with and without prehospital ECG) and self-arranged transport groups (n=124)
Table 3 shows that there were significant
differences in D2B or D2C times among the three
groups of patients with STEMI attending the AED
during daytime hours (08:00-17:59); there were no
significant differences between the groups during
night-time hours. The overall 30-day mortality of all
patients with clinically diagnosed STEMI was 8% (10
of 124 patients) [Table 4]. Fisher’s exact test did not
demonstrate any statistically significant difference
between the intervention and control groups.
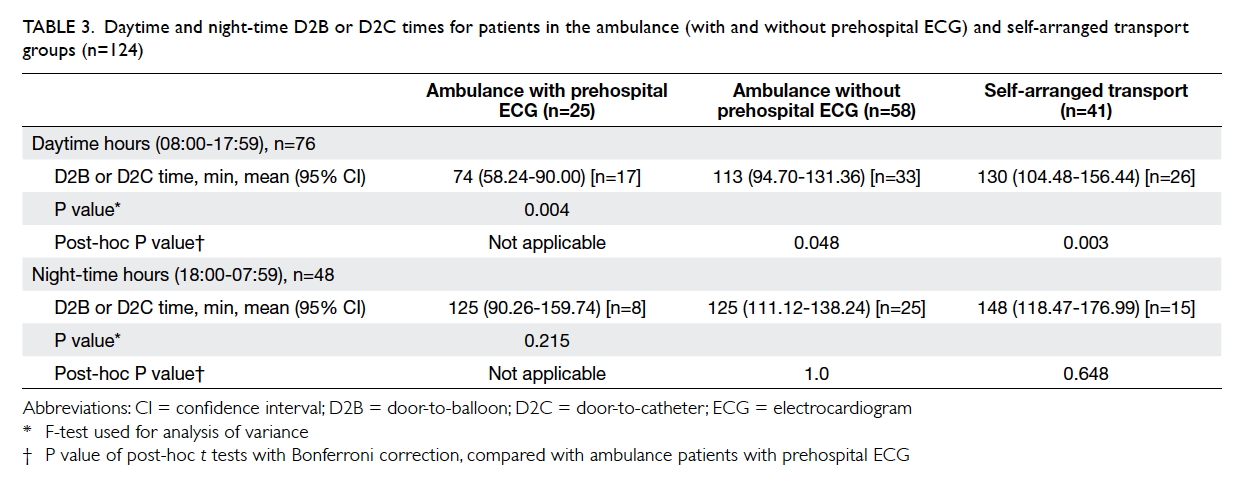
Table 3. Daytime and night-time D2B or D2C times for patients in the ambulance (with and without prehospital ECG) and self-arranged transport groups (n=124)
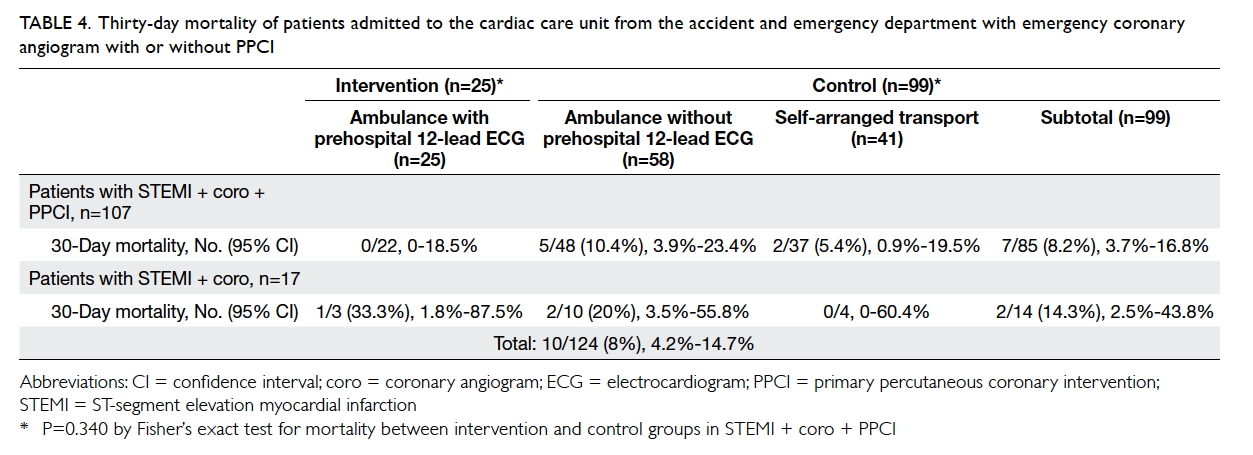
Table 4. Thirty-day mortality of patients admitted to the cardiac care unit from the accident and emergency department with emergency coronary angiogram with or without PPCI
When clinical diagnoses of STEMI were used
as a standard to verify diagnoses made by the X
Series® Monitor/Defibrillator diagnostic algorithm,
there were 14 true positive, three false positive,
702 true negative, and 12 false negative cases. This
corresponded to sensitivity (53.8%), specificity
(99.6%), positive predictive value (82.4%), negative
predictive value (98.3%), and accuracy (97.9%).
Discussion
Clinical diagnosis of ST-segment elevation
myocardial infarction
In an AED without point-of-care cardiac biomarker
testing capability, it is impossible to immediately
detect a rise and/or fall in cardiac biomarkers,
as described in the ‘Fourth universal definition
of myocardial infarction’.4 Some patients in the
AED with chest discomfort or other ischaemic
symptoms, who developed ST elevation in two
contiguous leads, were clinically diagnosed with
STEMI before confirmation of typical biomarker
changes, resulting in corresponding modification
to medical management. This caused inaccuracy
in calculation of the diagnostic performance of the
diagnostic algorithm used in the X Series®, when the
clinical diagnosis of STEMI in the AED was used as a
standard for comparison.
Shortened door-to-balloon or door-to-catheter
time during daytime hours
The theoretical benefits of prehospital 12-lead
ECG included early diagnosis by AED physicians,
early activation of the Acute Myocardial Infarction
Clinical Pathway with cardiologist input, and
activation of the CCL. It worked well during
office hours, when the full team of interventional
cardiologists, cardiac care nurses, and radiographers
were on-site. The shortest D2B time was 41 minutes.
However, during non-office hours or night-time
hours, this team had to return from their homes
for PPCI. This was the time-limiting factor during
night-time hours and there was no statistically
significant difference in night-time D2B or D2C
time in our series for ambulance patients with or
without prehospital 12-lead ECG. Possible solutions
might be the provision of sufficient manpower for
a 24-hour on-site interventional cardiology team.
Other measures, such as cardiologists receiving
prehospital 12-lead ECG data through their mobile
phones, or activation of the CCL by emergency
physicians (with an increased risk of inappropriate
activation) could be considered.
Comparison with international standards for
reperfusion
A greater percentage of patients with STEMI with
prehospital 12-lead ECGs received reperfusion
therapy with PPCI ≤90 minutes (Table 2). There
was also a reduction in 30-day mortality to 0% in
this subgroup (Table 4). However, whether a causeand-
effect relationship existed is uncertain, due to
our small sample size. Additionally, a statistically
significant difference in 30-day mortality could
not be demonstrated in our pilot project. Other
cardiovascular outcome measurements, including
re-infarction rate, major adverse cardiac events, and
heart failure rate could be studied to provide insights
regarding the benefit of prehospital 12-lead ECGs.
The D2B or D2C time could be improved
through measures such as the performance of
prehospital 12-lead ECGs on scene (rather than
in-ambulance), or skipping AED consultation with
direct cardiac care unit admission for patients
suspected of STEMI on prehospital ECGs.5
Inappropriate activation and false positivity
Inappropriate activation of the CCL occurred
when the interventional cardiologist provided an
alternative diagnosis or considered the patient not to
be a candidate for PPCI, with subsequent cancellation
of the catheterisation procedure. In QMH, the
CCL was activated by the on-call cardiologist, not
the emergency physician, for appropriate patients
with STEMI after on-site assessment. Therefore,
inappropriate activation of the CCL by the
emergency physician was 0% in our series. Instead,
false positivity existed. False positivity was defined
as patients with absence of thrombus causing
obstruction in the culprit vessels and absence of a
typical rise and fall of cardiac enzymes. In our pilot
project, 17 of 124 patients with STEMI admitted
through the AED had an emergency coronary
angiogram performed without PPCI. Excluding
one patient with triple vessel occlusion who failed
PPCI and required emergent coronary artery bypass
grafting, this yielded a false positive rate of 12.9% (16
of 124 patients). Prehospital 12-lead ECG extended
the emergency assessment of patient condition to
the prehospital phase. This allowed comparison of
prehospital and AED ECGs. Dynamic ECG changes
that occurred during the ambulance journey were
more likely to be detected. Whether this might help
to reduce the false positive activation of CCL or
false negative discharge of patients from AED can be
studied in the future.
Immediate electrocardiogram interpretation
In our pilot project, all ambulances equipped with
X Series® Monitor/Defibrillator served the QMH
catchment area without primary diversion. If primary
diversion of patients with STEMI to a hospital with
24-hour PPCI service were to be implemented,
on-scene ECG interpretation should be highly
sensitive to avoid under-diversion. The ECG data
could be interpreted by ambulance crews, machine
diagnostic algorithm, or emergency physicians or
cardiologists through tele-transmission. However,
not all ambulance crews in Hong Kong are trained
to interpret ECG data. Additionally, when compared
with clinical diagnosis of STEMI in the AED, the
sensitivity of the diagnostic algorithm used was
53.8% in our pilot project. Given this moderate
sensitivity, immediate ECG interpretation by
experienced emergency physicians or cardiologists
is preferable. This diagnostic process is inevitably
time-consuming. If ECG were performed on-scene
instead of in the ambulance compartment, transport
of the patient from scene to ambulance and the
diagnostic process could happen simultaneously.
Before ambulance departure from the scene, input
from the emergency physician or cardiologist would
be readily available to guide appropriate destination
AED selection.
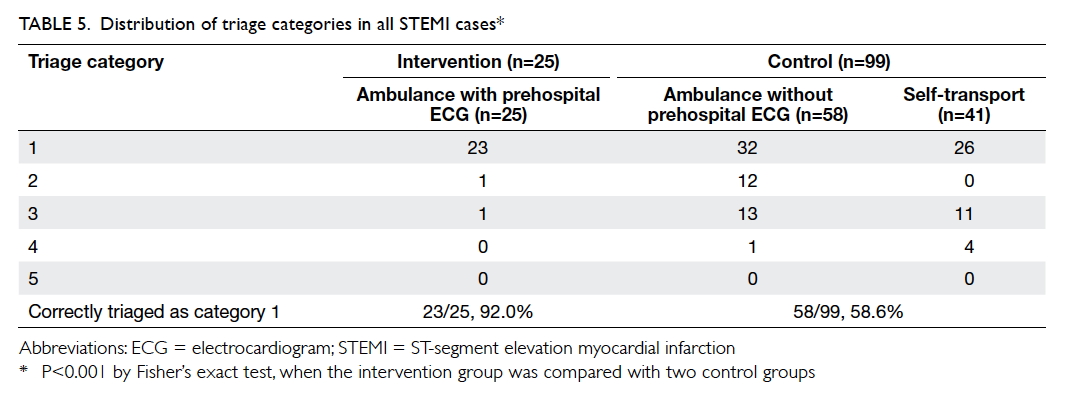
Reduction of under-triage in accident and
emergency department
Triage by AED nurses must be both efficient and
accurate, especially during busy periods. However,
chest pain is a subjective perception, as are all types
of pain. Before the availability of ECG, the vital signs
and brief clinical contact between triage nurses and
patients determined the assigned triage category for
each patient. Because patients with STEMI belonged
to category 1 (critical), it is inevitable that there
would be increased under-triage of STEMI cases in
the control group (Table 5). Prehospital ECG allowed
more accurate triage of patients with STEMI.
Overestimation of daytime door-to-balloon
or door-to-catheter time
In total, 61.3% (76/124) [Table 3] of emergency
coronary angiograms with or without PPCI were
performed during daytime hours (08:00-17:59).
However, this total includes patients who registered
during non-office hours on Saturday, Sunday, and
public holidays; during some of these, activation of
the CCL involved the interventional cardiology team
returning from home, as would be necessary during
night-time hours. Because night-time D2B or D2C
times were consistently longer than those recorded
during daytime hours (Table 3), daytime D2B or D2C
times were most likely overestimated. Studies have
shown that in units with no significant difference
in reperfusion time during daytime and night-time
hours, the mortality of patients with STEMI was not
influenced by whether patients presented during
standard working hours or outside of these hours.6
Measures could be implemented to shorten the
night-time D2B or D2C time for improved patient
outcomes.
Thirty-day mortality
The Acute Myocardial Infarction Clinical Pathway
was first established in QMH in 2007; by 2011, it
successfully reduced the 30-day mortality rate of
acute myocardial infarction from 18.4% to 14.9%.7
The mortality in our pilot project was 8.2% in the
control group with conventional management
(Table 4). This reduction of mortality in the control
group was likely a combined result of advances
in cardiovascular medications and diagnostic or
therapeutic technologies, as well as improvement
of patient health awareness in recent years. With
implementation of prehospital 12-lead ECG,
further reduction of mortality was expected. In our
subgroup with prehospital 12-lead ECG and PPCI,
30-day mortality of 0% was recorded. However, a
larger study over longer period of time is needed to
establish whether there is a statistically significant
clinical impact of prehospital 12-lead ECG on long-term
mortality.
Mode of transport
Approximately one-third (41 of 124) of patients with
AED diagnosis of STEMI arranged self-transport,
rather than calling an ambulance. This underuse
of the ambulance service is not unique to Hong
Kong8 9 10and has been a well-documented cause of
delayed hospital presentation8 10 and reperfusion
time.10 In addition to the inability to perform
prehospital ECG, patients with STEMI who self-transported
to the AED were deprived of early
assessment by the ambulance crew, administration
of aspirin and/or sublingual nitrate, early notification
of the AED for patients with unstable vitals, and
immediate cardiopulmonary resuscitation (with
defibrillation if necessary). Thus, wise use of the
ambulance service should be advocated.
Incomplete coverage of the catchment area
According to the HKFSD, 88% of the QMH catchment
area was covered by the 15 ambulances with X
Series® Monitor/Defibrillator installed. Owing
to this incomplete catchment area coverage, 48
ambulance patients did not receive prehospital ECG
before PPCI. A greater benefit might be observed
in the future, if all ambulances in the territory were
capable of transmitting prehospital ECG, together
with primary diversion of patients with STEMI.
Patient refusal
Consent to perform prehospital 12-lead ECG was
not obtained from 110 of 841 (13.1%) patients with
cardiac chest pain (71 female and 39 male patients).
Refusal to consent may result in worse outcomes
for patients with STEMI with delayed PPCI. Public
education regarding the benefit of performing
prehospital ECG may reduce refusal rates.
Referral from private physicians
Of 124 patients with STEMI attending the AED,
20 (16.1%) consulted private physicians before
attendance to the AED; a number of ECGs performed
in these private clinics or hospitals documented
STEMI. However, apart from handwritten
referral letters, there is currently no formal direct
communication channel between private physicians
and AED physicians. More convenient means of
prehospital communication with or without teletransmission
of prehospital 12-lead ECG performed
in private clinics or hospitals could be explored. The
benefits of seamless communication between private
physicians and the AED are not limited to STEMI
alone and may affect many other medical conditions.
Conclusion
Prehospital 12-lead ECG is technologically feasible
in Hong Kong and shortens the D2B time. However,
shorter reperfusion time was recorded only during
daytime hours. Promotion of prehospital 12-lead
ECG and proper utilisation of ambulance services for
patients with cardiac chest pain may allow additional
patients with STEMI to benefit from prehospital
ECG.
Author contributions
Concept or design: All authors.
Acquisition of data: KS Cheung, YC Siu, RHW Chan.
Analysis or interpretation of data: KS Cheung, LP Leung.
Drafting of the article: KS Cheung.
Critical revision for important intellectual content: All authors.
Acquisition of data: KS Cheung, YC Siu, RHW Chan.
Analysis or interpretation of data: KS Cheung, LP Leung.
Drafting of the article: KS Cheung.
Critical revision for important intellectual content: All authors.
Acknowledgement
We would like to thank the staff of the following institutions:
Hong Kong Fire Services Department, for performing
prehospital electrocardiograms and providing prehospital
data; Division of Cardiology, Department of Medicine,
Queen Mary Hospital, for providing data on door-to-balloon
and door-to-catheter time; Department of Accident and
Emergency, Queen Mary Hospital, for collecting patient
clinical data; Emergency Medical Unit, LKS Faculty of
Medicine, the University of Hong Kong, for statistical analyses;
and Zoll Medical Corporation (269 Mill Rd, Chelmsford, MA
01824-4105, US), for providing the machines, training, and
technical support free of charge.
Declaration
All authors have disclosed no conflicts of interest. All authors
had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Funding/support
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Ethical approval
Analysis of data from this pilot project was approved by the
Institutional Review Board of the University of Hong Kong/
Hospital Authority Hong Kong West Cluster (UW17-318).
Patient consent was waived.
References
1. Nagel EL, Hirshman JC, Nussenfeld SR, Rankin D, Lundblad
E. Telemetry-medical command in coronary and other
mobile emergency care systems. JAMA 1970;214:332-8. Crossref
2. O’Connor RE, Al Ali AS, Brady WJ, et al. Part 9: acute
coronary syndromes: 2015 American Heart Association
Guidelines Update for Cardiopulmonary Resuscitation
and Emergency Cardiovascular Care. Circulation
2015;132:S483-500. Crossref
3. Le May MR, Davies RF, Dionne R, et al. Comparison of early
mortality of paramedic-diagnosed ST-segment elevation
myocardial infarction with immediate transport to a
designated primary percutaneous coronary intervention
center to that of similar patients transported to the nearest
hospital. Am J Cardiol 2006;98:1329-33. Crossref
4. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal
definition of myocardial infarction (2018). Eur Heart J 2018
Aug 25. Epub ahead of print. Crossref
5. Anderson LL, French WJ, Peng SA, et al. Direct transfer
from the referring hospitals to the catheterization
laboratory to minimize reperfusion delays for primary
percutaneous coronary intervention: insights from the
National Cardiovascular Data Registry. Circ Cardiovasc
Interv 2015;8:e002477. Crossref
6. Cockburn J, Karimi K, Hoo S, et al. Outcomes by day and
night for patients bypassing the emergency department
presenting with ST-segment elevation myocardial
infarction identified with a pre-hospital electrocardiogram.
J Interv Cardiol 2015;28:24-31. Crossref
7. Wong KL, Wong YT, Yung SY, et al. A single centre
retrospective cohort study to evaluate the association
between implementation of an acute myocardial infarction
clinical pathway and clinical outcomes. Int J Cardiol
2015;182:82-4. Crossref
8. Hong CC, Sultana P, Wong AS, Chan KP, Pek PP, Ong
ME. Prehospital delay in patients presenting with acute
ST-elevation myocardial infarction. Eur J Emerg Med
2011;18:268-71. Crossref
9. Song L, Yan HB, Yang JG, et al. Factors associated with
use of emergency medical service for acute myocardial
infarction in Beijing [in Chinese]. Zhonghua Yi Xue Za Zhi
2010;90:834-8.
10. Mathews R, Peterson ED, Li S, et al. Use of emergency
medical service transport among patients with ST-segment-elevation myocardial infarction: findings from
the National Cardiovascular Data Registry Acute Coronary
Treatment Intervention Outcomes Network Registry—Get
With The Guidelines. Circulation 2011;124:154-63. Crossref