Serial surveys of Hong Kong medical students regarding attitudes towards HIV/AIDS from 2007 to 2017
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Serial surveys of Hong Kong medical students
regarding attitudes towards HIV/AIDS from 2007 to 2017
Greta Tam, MB, BS, MS1; NS Wong, PhD2; SS Lee, MD2
1 Department of Medicine, The University of Hong Kong, Hong Kong
2 Department of Medicine, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Prof SS Lee (sslee@cuhk.edu.hk)
Abstract
Introduction: With widespread adoption of
antiretroviral therapy, human immunodeficiency
virus (HIV) epidemiology has changed since the late
2000s. Accordingly, attitudes towards the disease
may also have changed. Because medical students
are future physicians, their attitudes have important
implications in access to care among patients with
HIV/acquired immunodeficiency syndrome (AIDS).
Here, we performed a survey to compare medical
students’ attitudes towards HIV/AIDS between the
late 2000s (2007-2010) and middle 2010s (2014-2017).
Methods: From 2007 to 2010, we surveyed three
cohorts of medical students at the end of clinical
training to assess their attitudes towards HIV/AIDS.
From 2014 to 2017, we surveyed three additional
cohorts of medical students at the end of clinical
training to compare changes in attitudes towards
HIV/AIDS between the late 2000s and middle 2010s.
Each set of three cohorts was grouped together to
maximise sample size; comparisons were performed
between the 2007-2010 and 2014-2017 cohorts.
Results: From 2007 to 2010, 546 medical students
were surveyed; from 2014 to 2017, 504 students were surveyed. Compared with students in the late 2000s,
significantly fewer students in the mid-2010s initially
encountered patients with HIV during attachment
to an HIV clinic or preferred to avoid work in a field
involving HIV/AIDS; significantly more students
planned to specialise in HIV medicine. Student
willingness to provide HIV care remained similar
over time: approximately 78% of students were
willing to provide care in each grouped cohort.
Conclusion: Although medical students had
more positive attitudes towards HIV/AIDS, their
willingness to provide HIV care did not change
between the late 2000s and middle 2010s.
New knowledge added by this study
- Although medical students had more positive attitudes towards human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), their willingness to provide HIV care in Hong Kong did not change between the late 2000s and middle 2010s.
- Interventions to reduce stigmatising attitudes towards people living with HIV should be incorporated during training for healthcare professionals.
- The medical school curriculum could be updated to incorporate interventions that involve experiential and affective teaching components to adequately address HIV stigma; additional clinical attachments can ensure that medical students have adequate exposure to patients with HIV.
Introduction
Since the beginning of the human immunodeficiency
virus (HIV) epidemic, stigma and discrimination
have affected the provision of healthcare to patients
with HIV. These factors have limited access to HIV
testing and treatment; they have also prevented
the uptake of interventions, such as pre-exposure
prophylaxis.1 The global shift necessary in the
biomedical response to acquired immunodeficiency
syndrome (AIDS) thus heavily relies on reductions of both stigma and discrimination. The importance
of stigma reduction has been recognised as a key
priority in the Blueprint for Achieving an AIDS-Free
Generation (established by The United States
President’s Emergency Plan for AIDS Relief)2 and in
the HIV investment framework (established by The
Joint United Nations Programme on HIV/AIDS).3
For many years, stigma from healthcare
professionals has remained a major barrier to
access for HIV prevention and treatment services. According to aggregated data from the Stigma
Index for 50 countries, healthcare has been denied
to one in eight people living with HIV (PLHIV).4
Despite high antiretroviral therapy coverage, Hong
Kong is no exception to this phenomenon. In the
early and middle 2010s, 26.8% of PLHIV reported
stigmatising experiences during treatment for non-
HIV-related healthcare needs.5 Since the late 2000s,
advances in HIV treatment have led to a decline in
mortality.6 Increasing life expectancy among PLHIV
has resulted in higher HIV prevalence.7 Thus,
medical students have an increased likelihood of
encountering patients with HIV in future clinical
practice, irrespective of their specialties. Because
HIV epidemiology has changed over the years,
medical students’ attitudes towards the disease
may also have changed. If attitudes have changed,
the medical school curriculum should be adjusted
to match such changes; this will ensure that future
physicians can provide the best possible care. To our
knowledge, no study has compared changes over
time in medical students’ attitudes towards HIV.
Thus, we performed a survey to compare medical
students’ attitudes towards HIV/AIDS between the
late 2000s (2007-2010) and middle 2010s (2014-2017).
Methods
Study design
This study was a descriptive cross-sectional survey to measure medical students’ attitudes towards HIV/AIDS, as well as their experiences within the HIV curriculum.
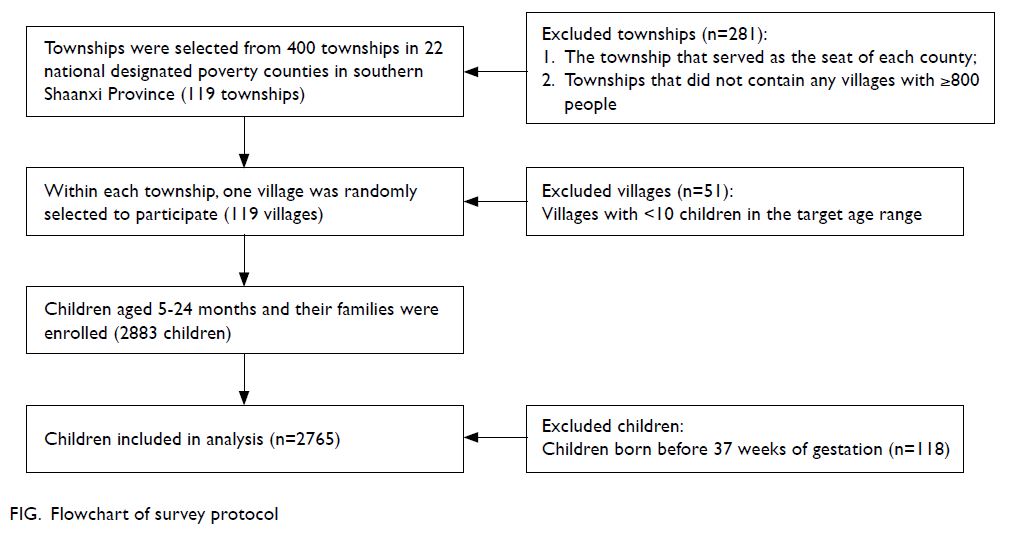
Sampling
An assessment survey was administered to final-year
medical students at the Chinese University of
Hong Kong, one of the two medical schools in Hong
Kong. Questionnaires were distributed to medical
students at the end of their final-year attachment to
an HIV specialist clinic. At the Chinese University
of Hong Kong, HIV education is an integral part of
the medical student curriculum. Over the course of
3 years, students attend microbiology and medicine
lectures regarding HIV/AIDS, a community
medicine module that includes the prevention and
control of HIV infection, a half-day attachment
to Hong Kong’s largest HIV specialist clinic, and
hospital ward rounds that involve patients with
HIV. The HIV curriculum was generally consistent
between the late 2000s and middle 2010s. This study
was based on the analysis of survey data collected
from six cohorts of medical students: three from
2007 to 2010 and three from 2014 to 2017. All
students were asked to complete the survey during
their final teaching session. Hard copies of the
self-administered structured questionnaire were
distributed to the students and collected by the
course instructors. All responses were anonymous
and participation was voluntary.
Data collection instrument
The study questionnaire was originally developed as
an assessment form by the HIV medicine teaching
team at the Chinese University of Hong Kong; it
was designed for completion by final-year medical
students. The form was piloted in 2005 and became
standardised in 2007, with minor modifications in
subsequent years.8 The questionnaire was in English
and consisted of 25 close-ended questions; all
questions were completed by the students without
assistance. The questionnaire contents slightly
differed between the 2007-2010 and 2014-2017
survey periods. Seven questions that appeared in
both questionnaires were selected for analysis.
These questions focused on demographics, exposure
to patients with HIV, and attitudes towards patients
with HIV. Eight additional questions were analysed
for cohorts from 2014 to 2017. These questions
focused on a participant’s ability to recall various
HIV learning experiences and their satisfaction with
clinical exposure during attachment to an HIV clinic.
We divided students into groups according to their willingness to provide HIV care in the future. An
unwilling student chose “strongly agree” or “agree” (on a four-point scale for cohorts from 2007 to 2010
and a six-point scale for cohorts from 2014 to 2017)
when asked whether they would refuse to perform
treatment or surgical procedures for patients with HIV.
Statistical analysis
We calculated proportions of responses, along
with exact binomial 95% confidence intervals (CIs).
We used bivariable logistic regression to compare
exposure and attitudes between participants in the
2007-2010 cohort (cohorts from 2007 to 2010) and
the 2014-2017 cohort (cohorts from 2014 to 2017);
each set of three cohorts was grouped together
to maximise sample size. Factors associated with
willingness to provide HIV care were analysed
using bivariable logistic regression. SPSS software
(Windows version 26; IBM Corp., Armonk [NY],
United States) was used for data management and
statistical analyses. Two-sided P values <0.05 were
considered statistically significant.
Results
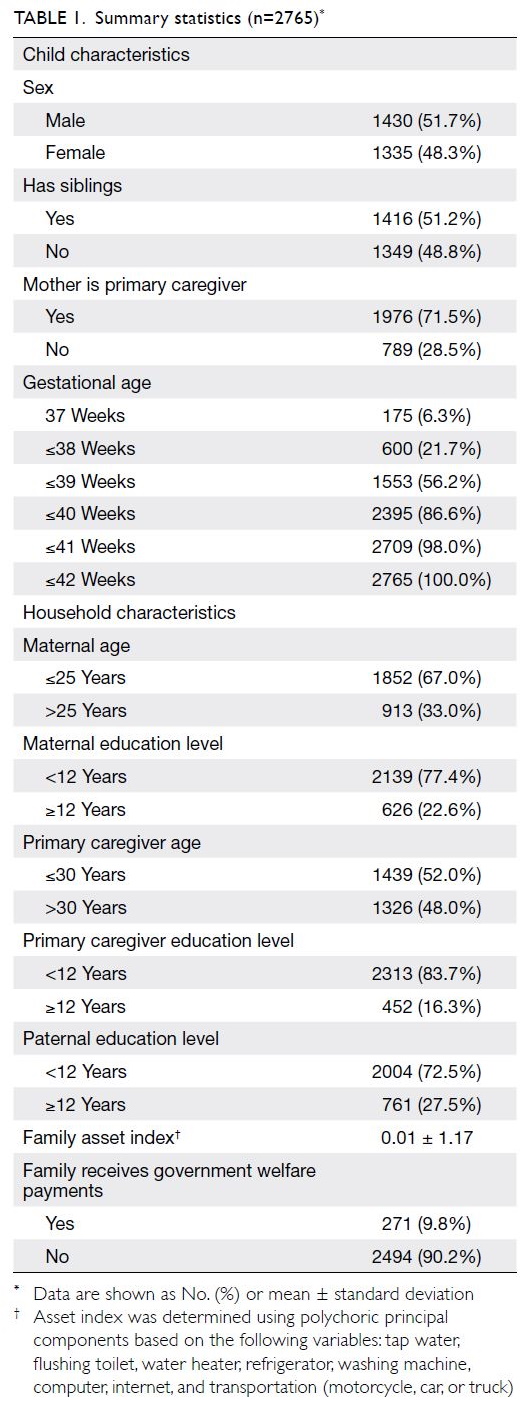
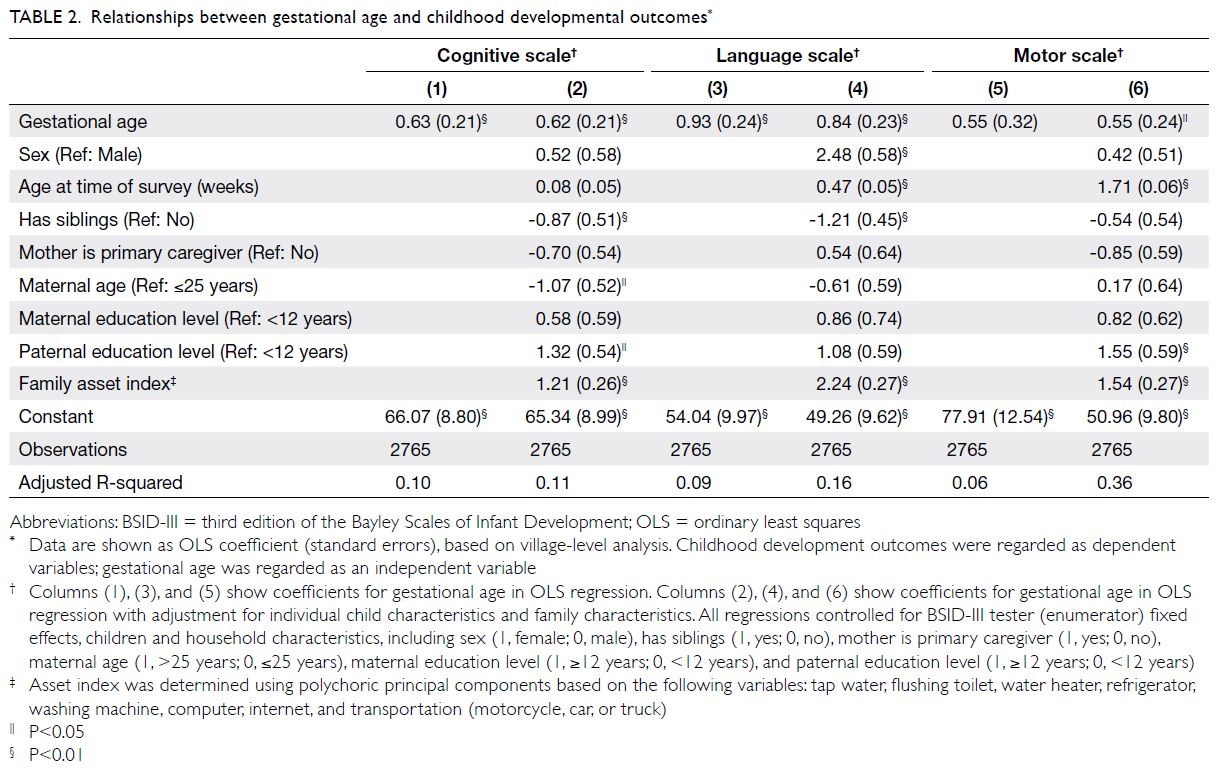
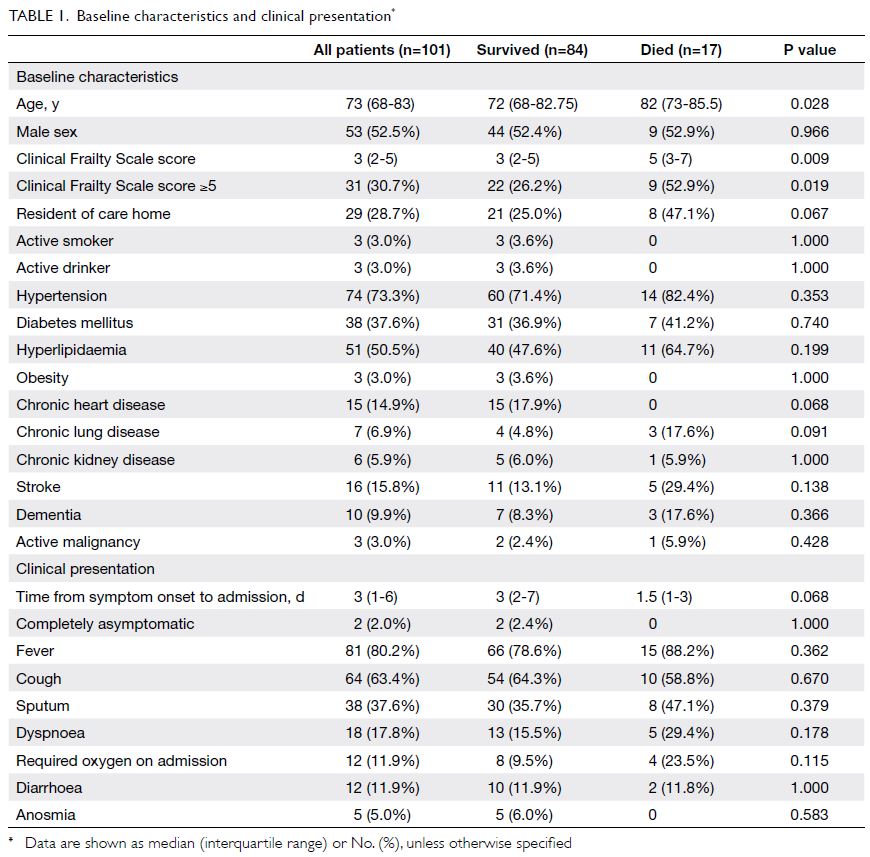
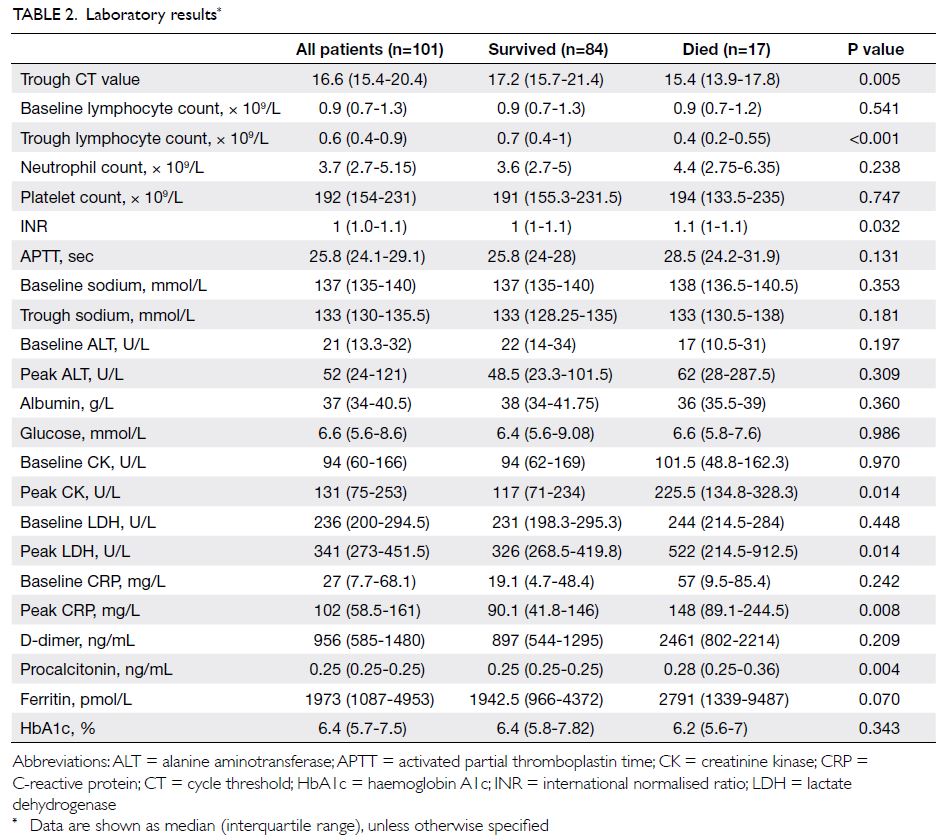
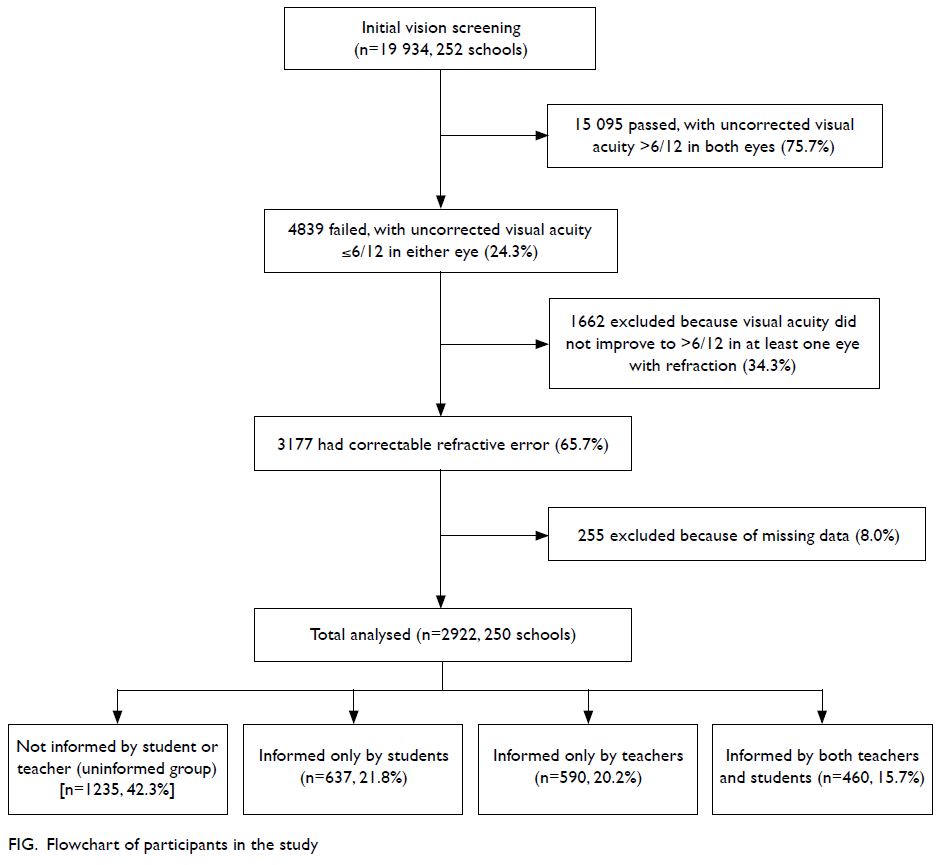
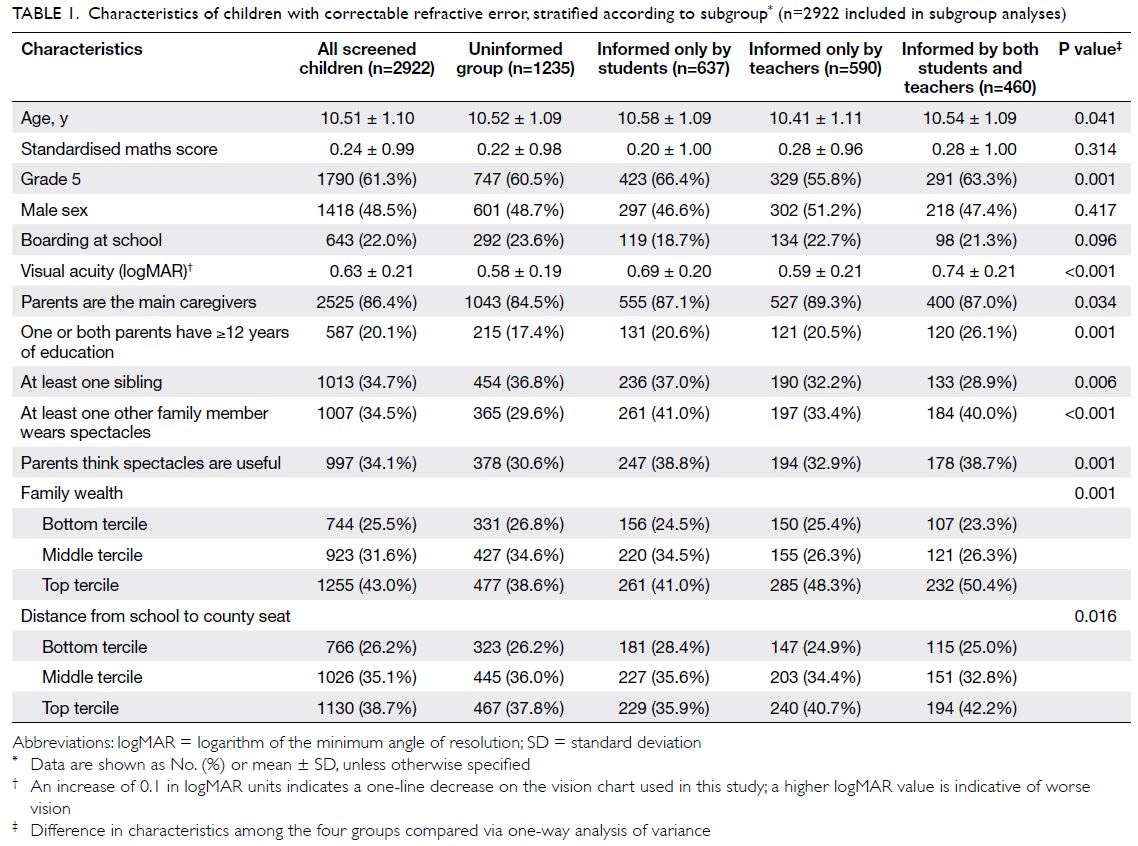
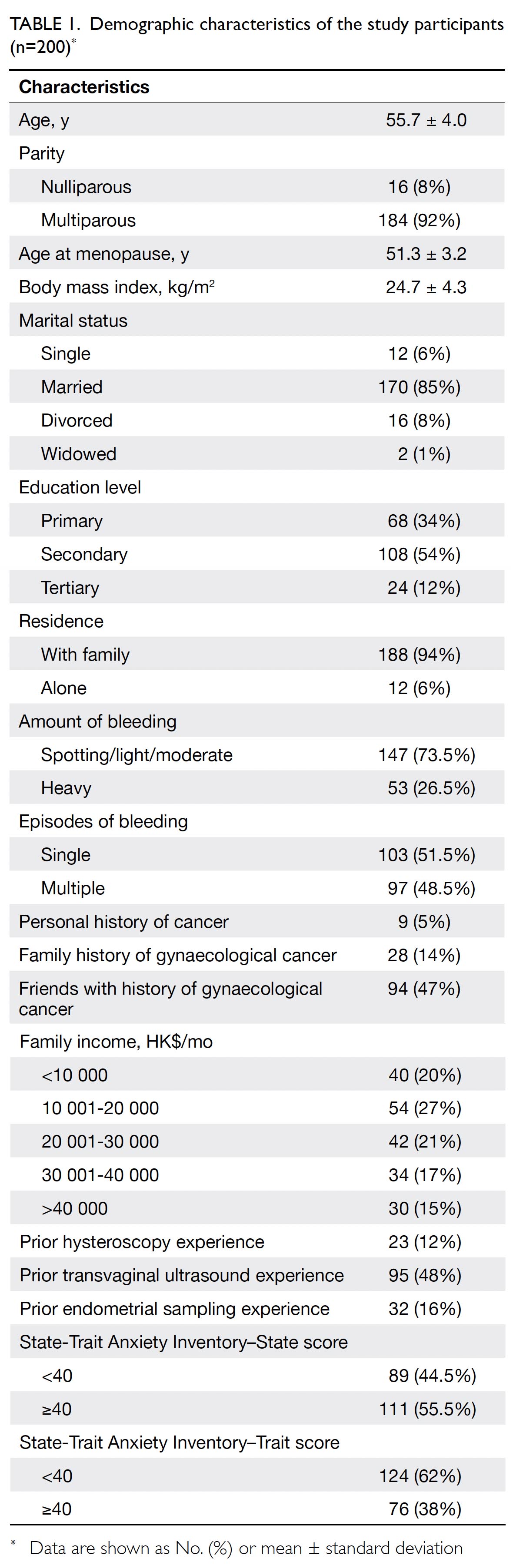
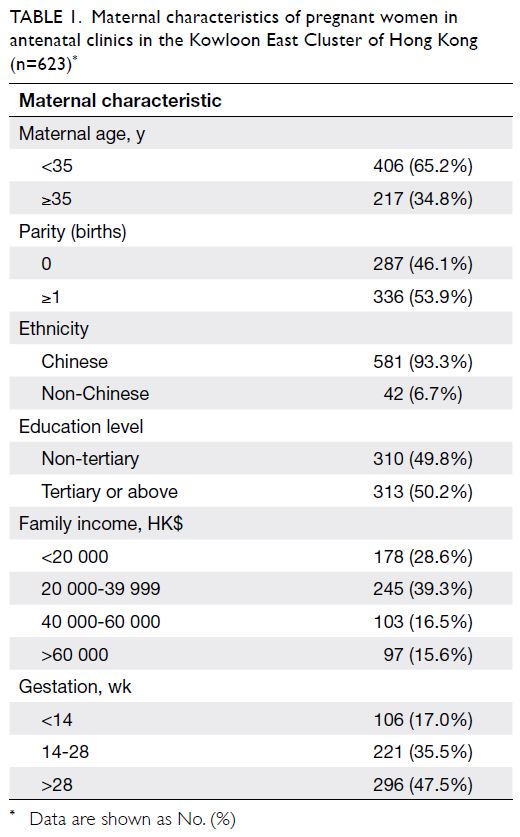
Participant characteristics
In total, 1050 final-year students participated in the
survey. Three cohorts of final-year medical students
participated between 2007 and 2010 (n=546); three
additional cohorts of final-year medical students
participated between 2014 and 2017 (n=504).
The response rates were 97% in the 2007-2010
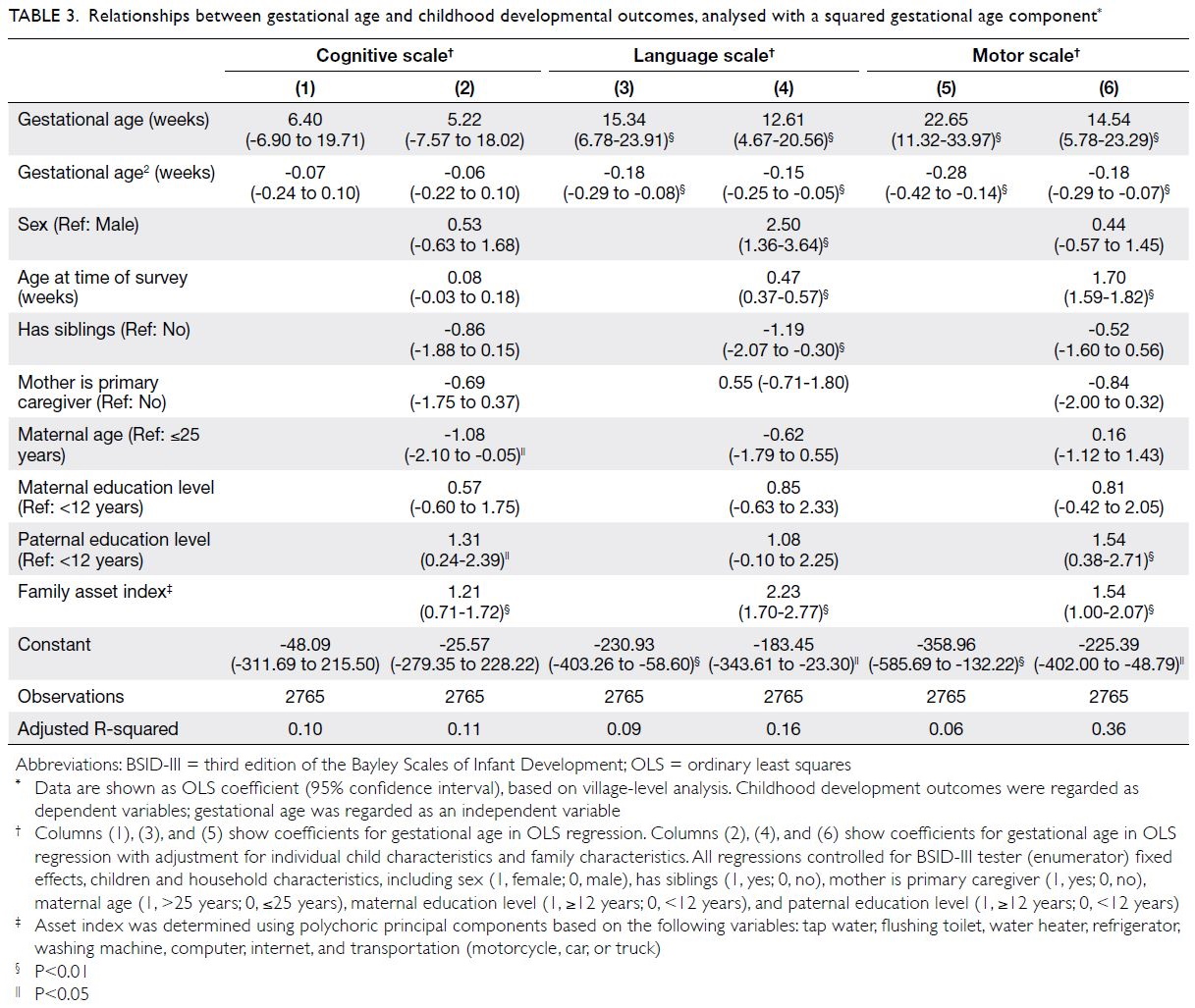
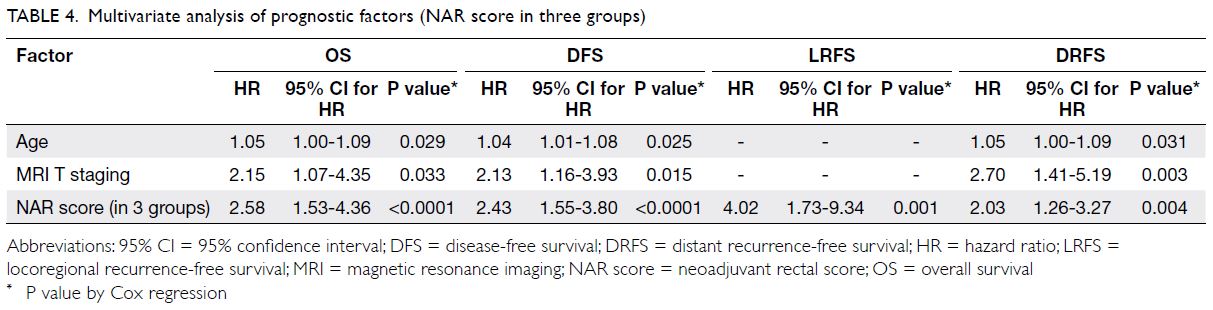
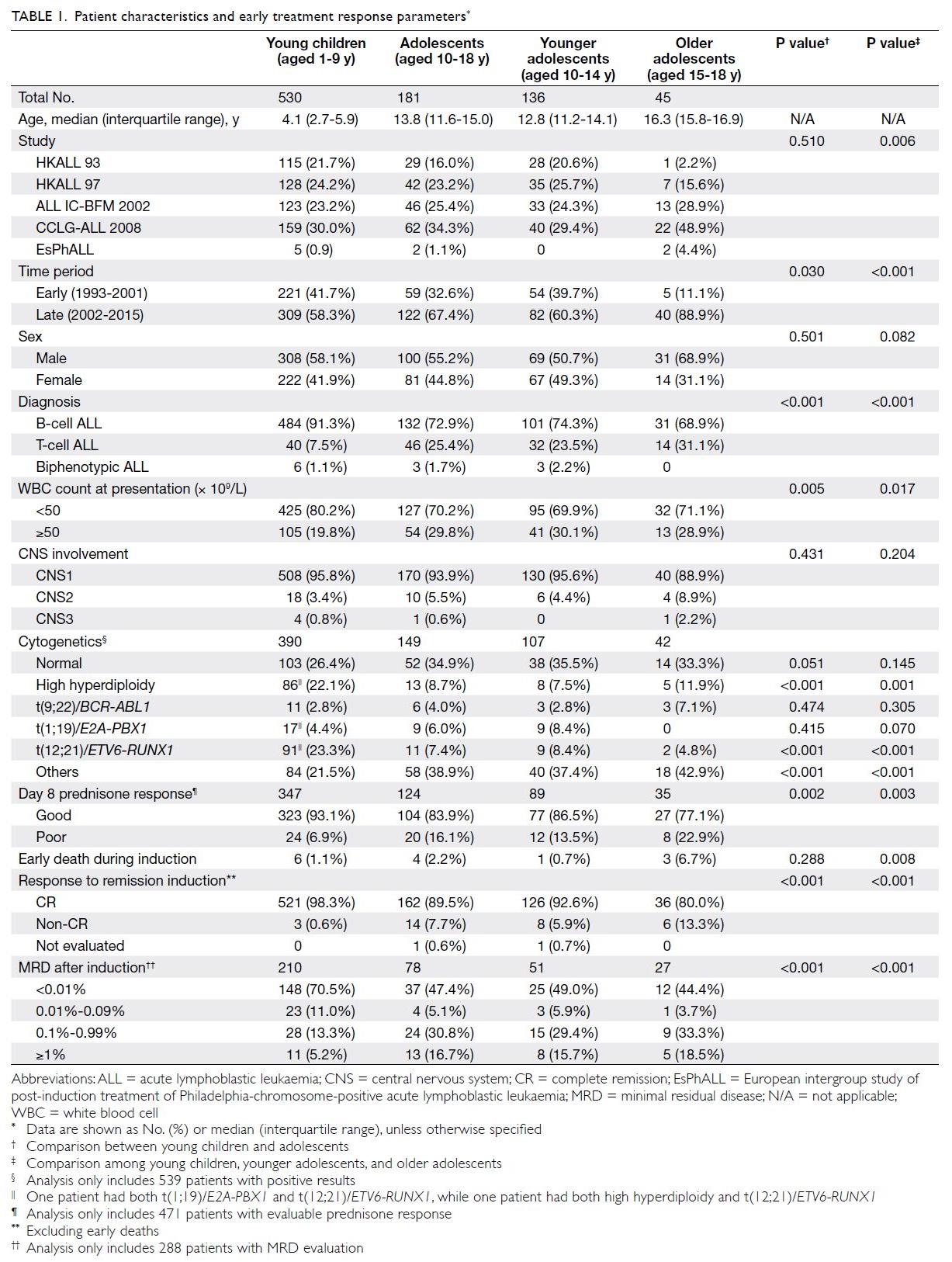
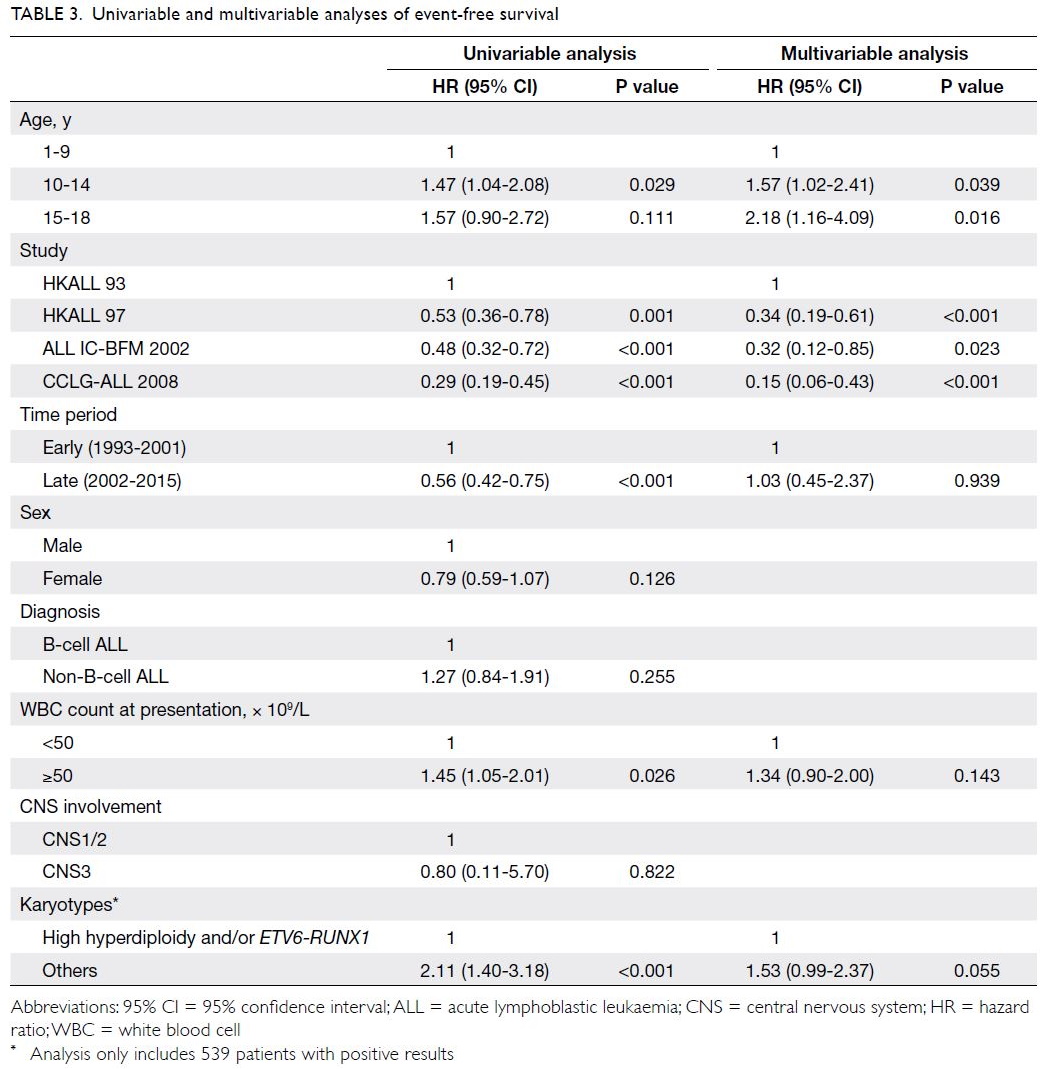
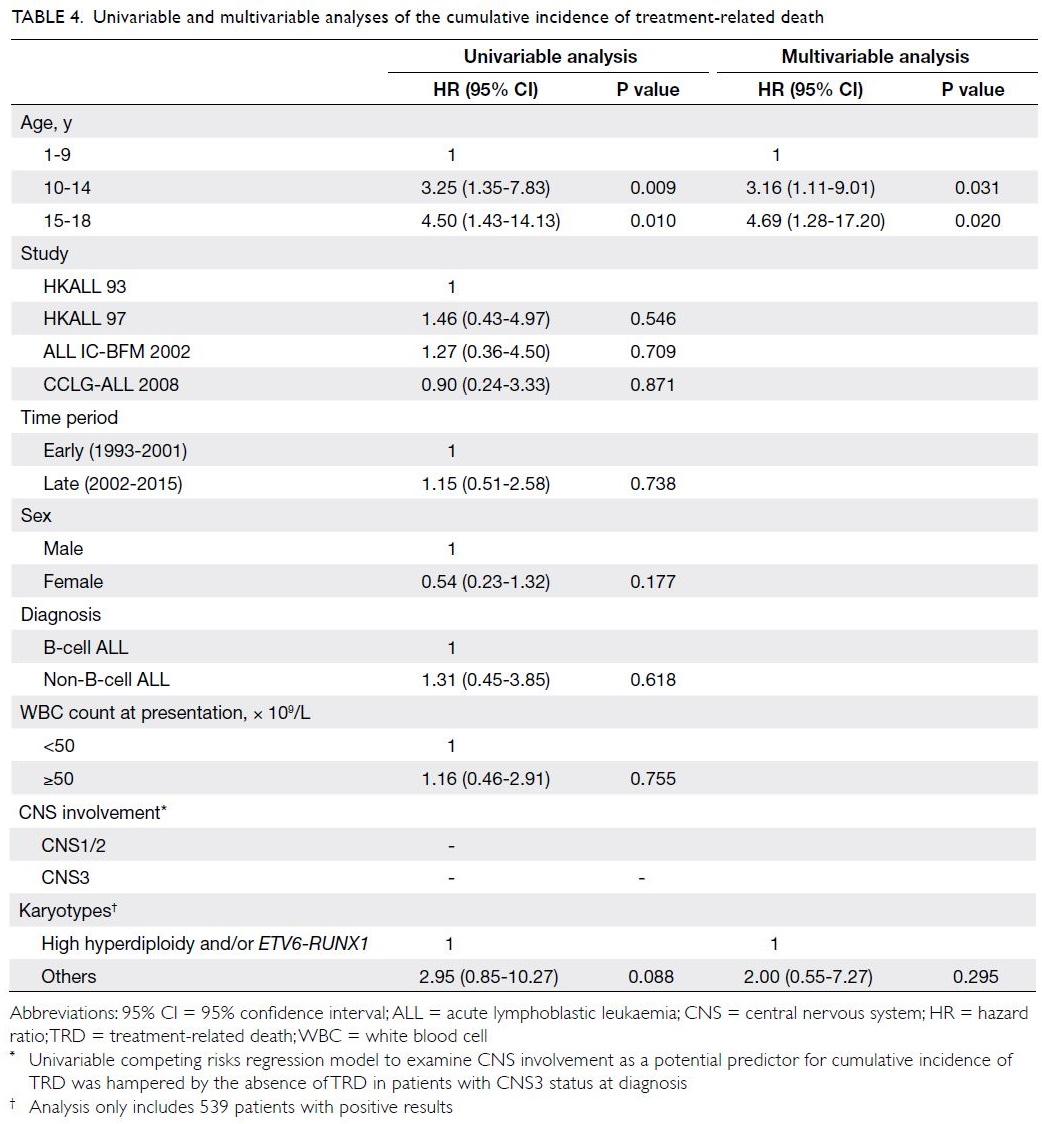
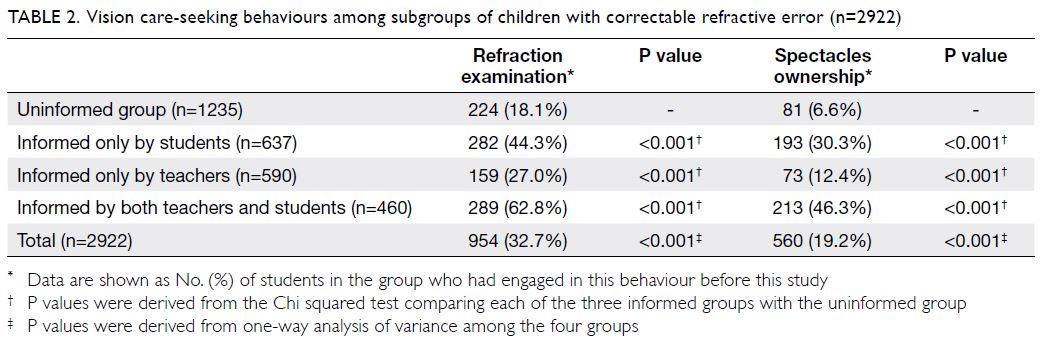
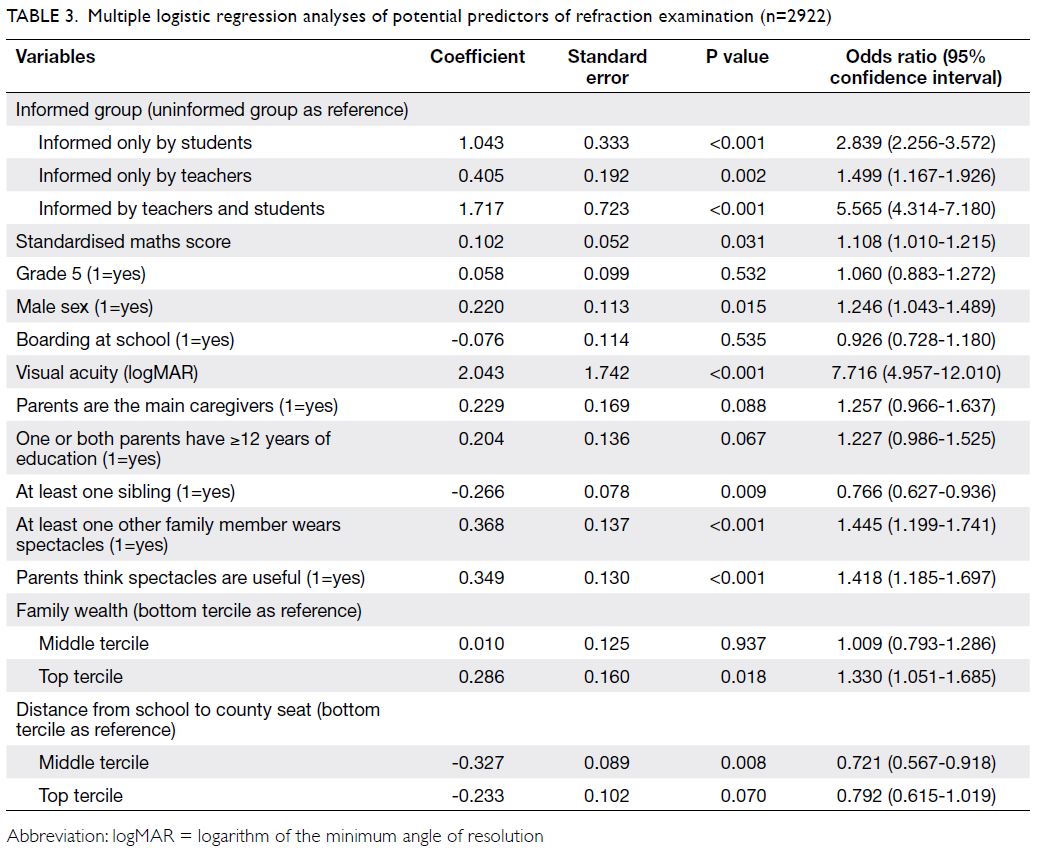
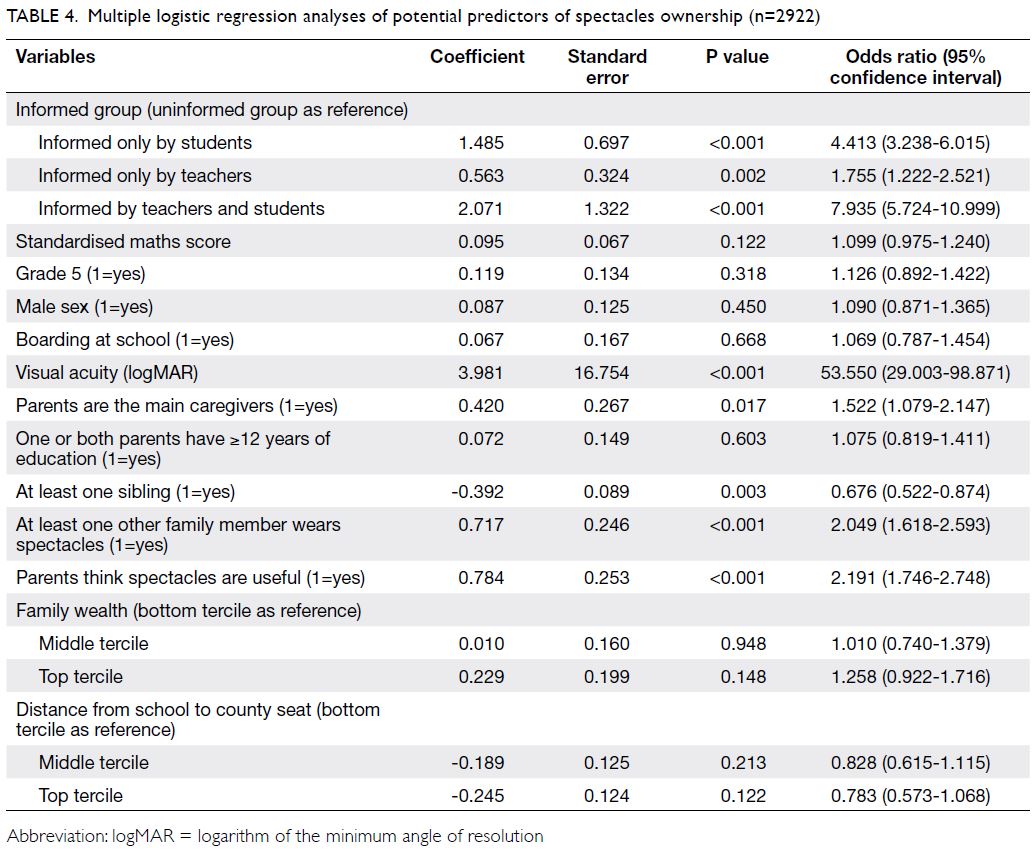
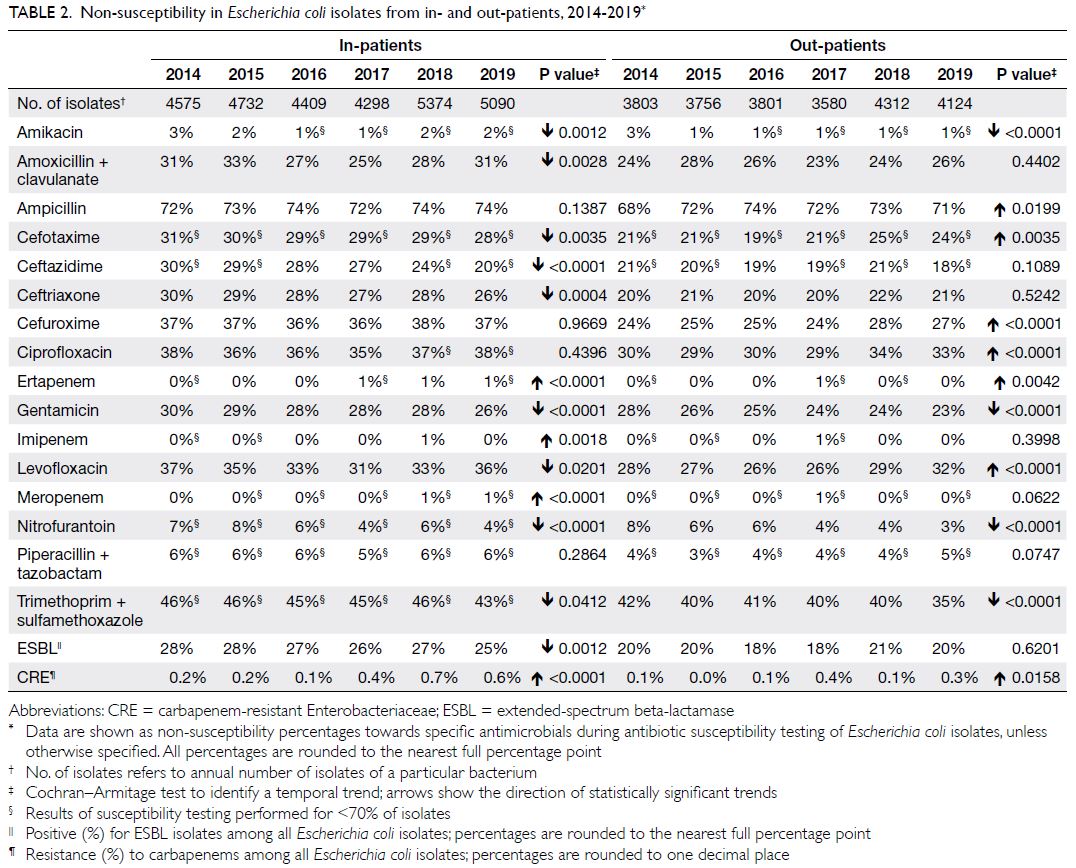
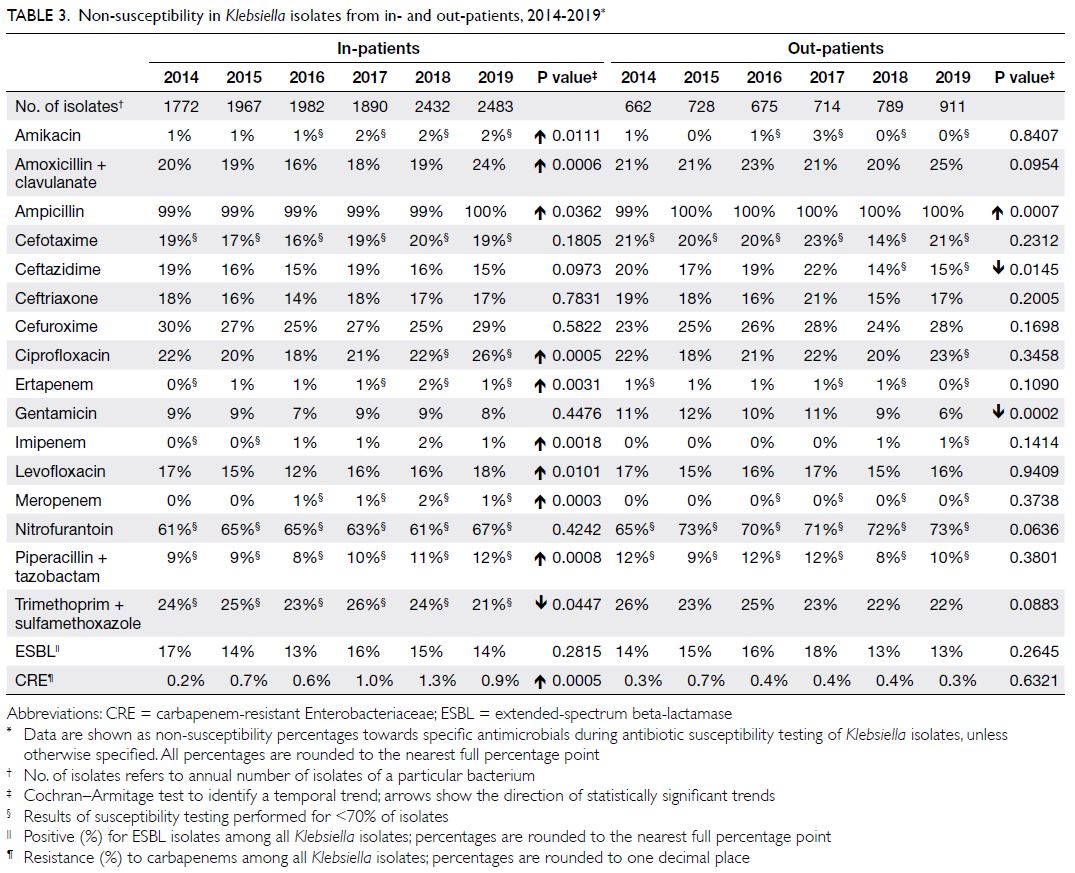
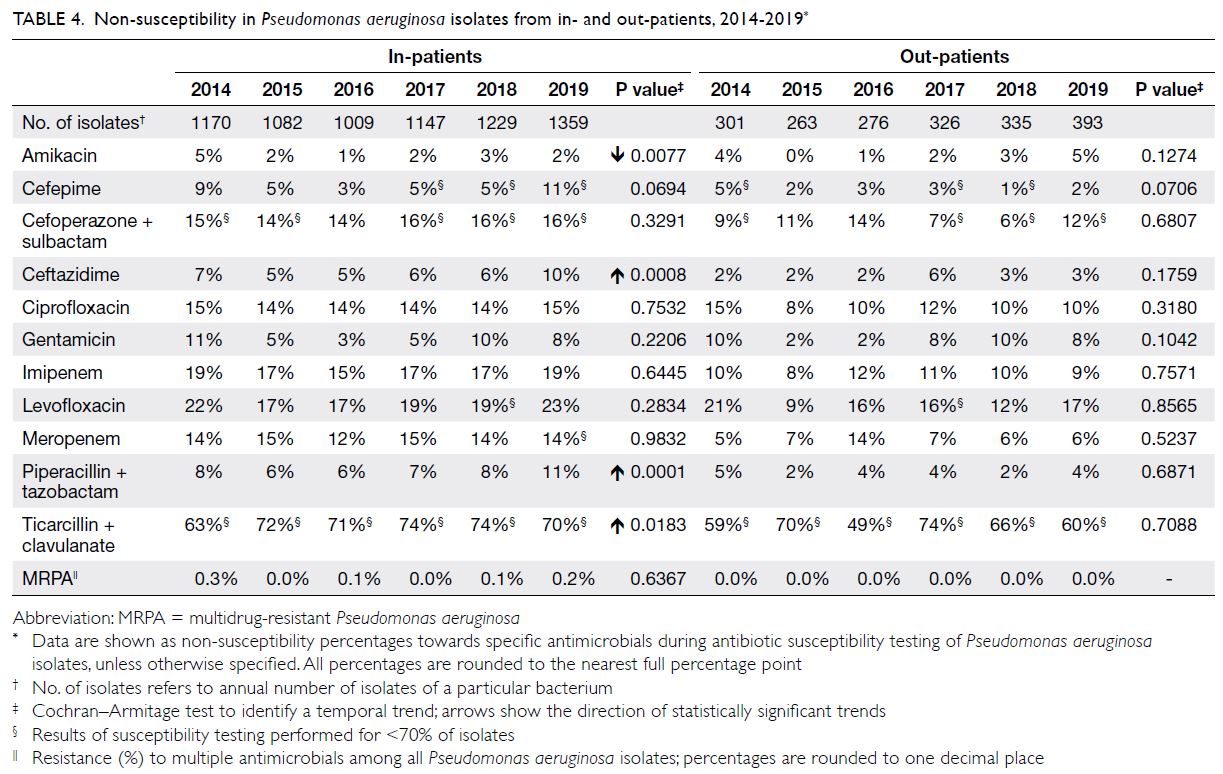
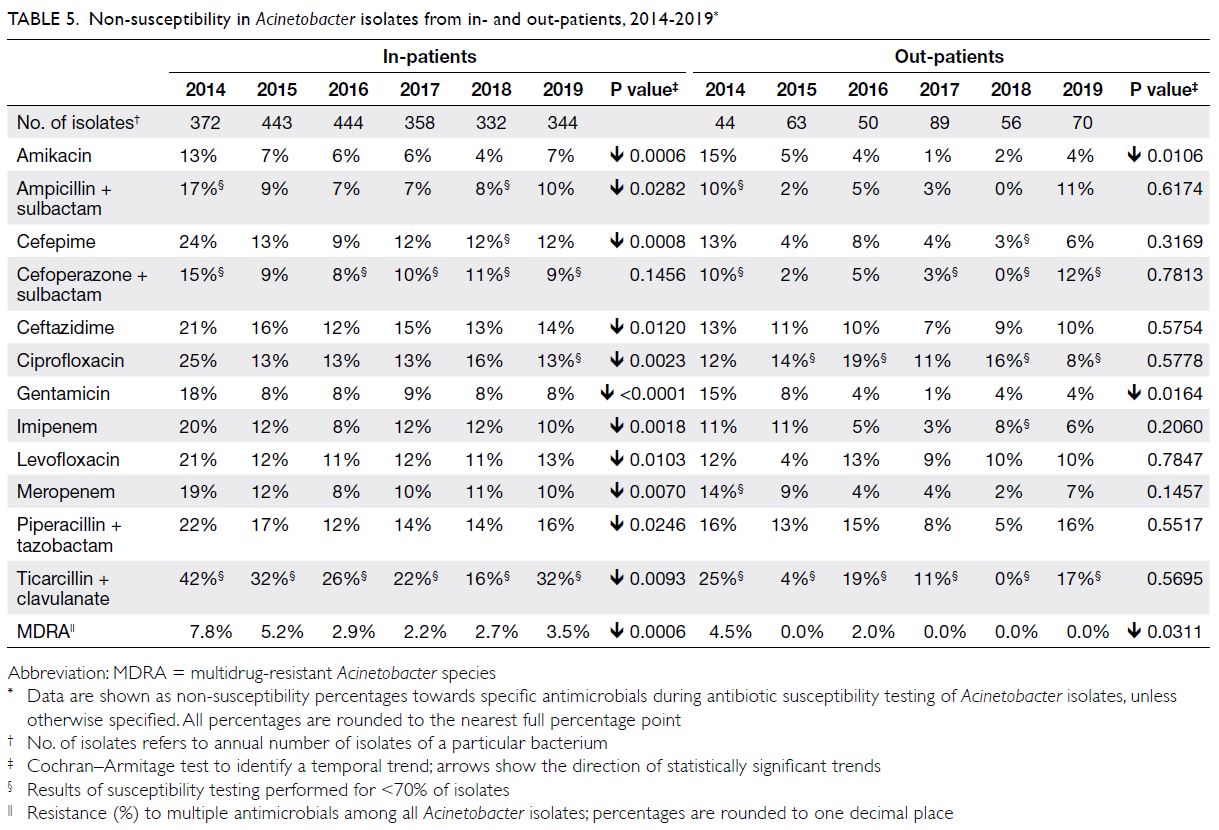
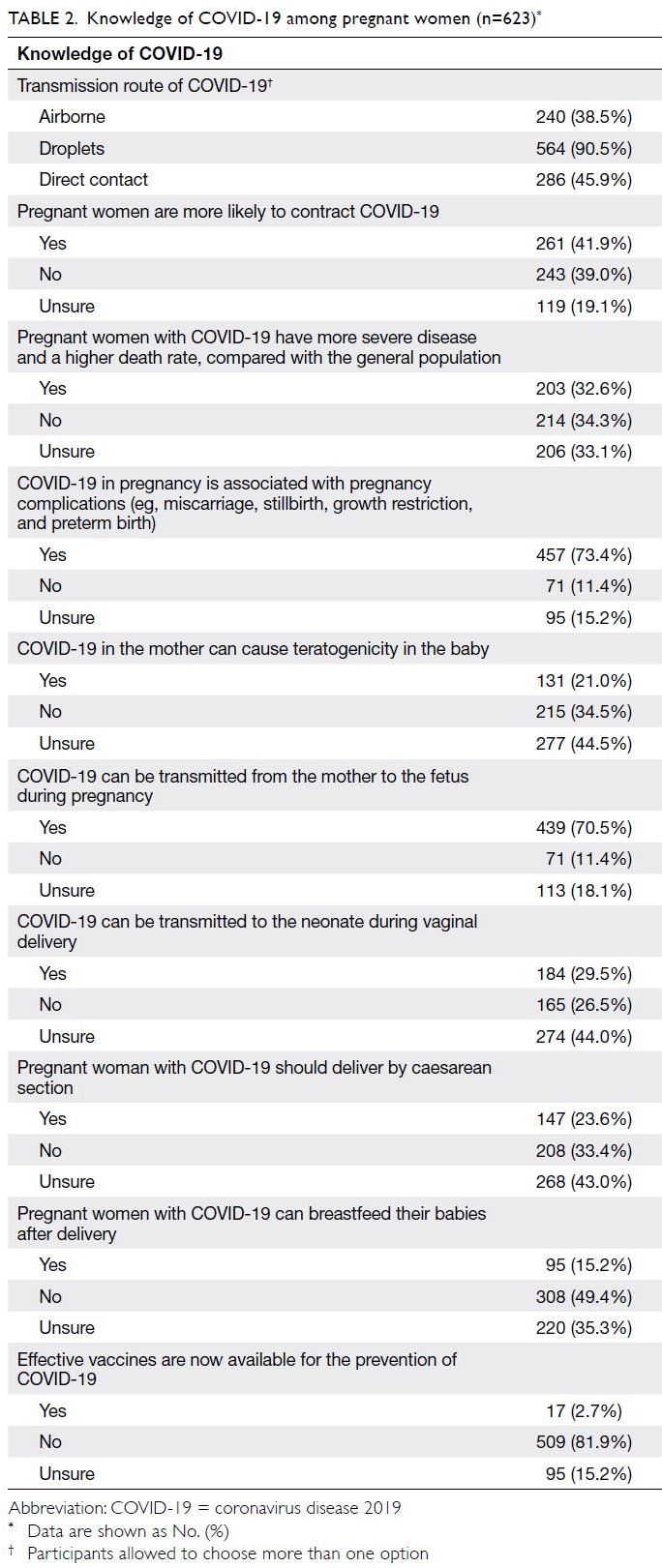
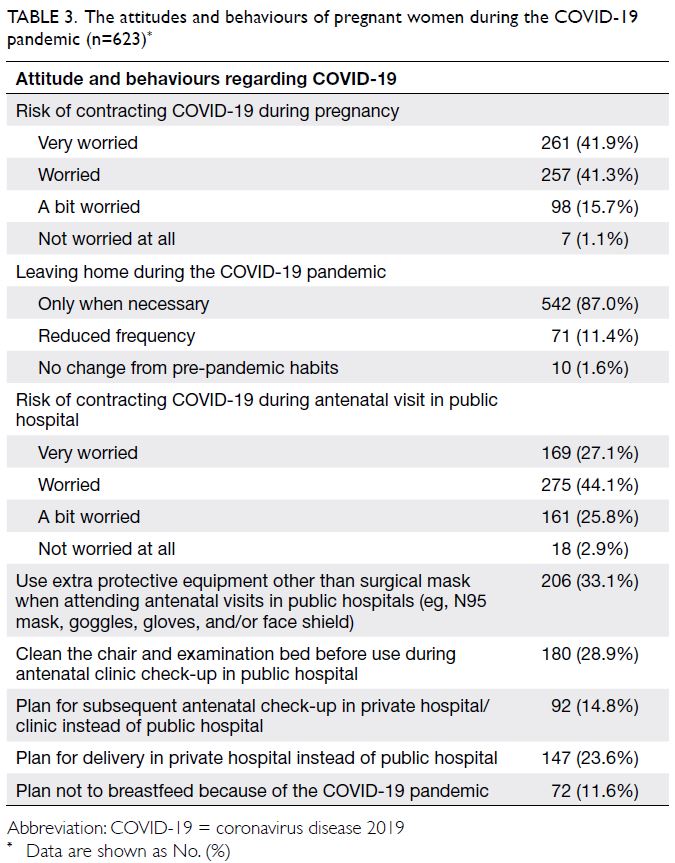
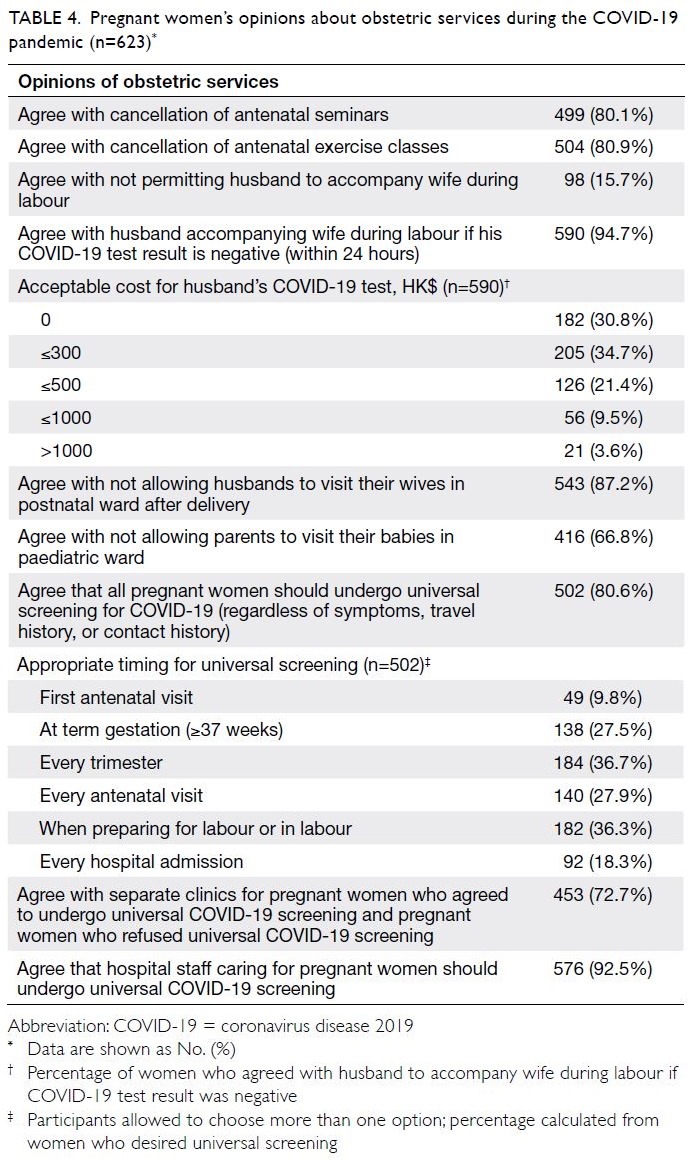
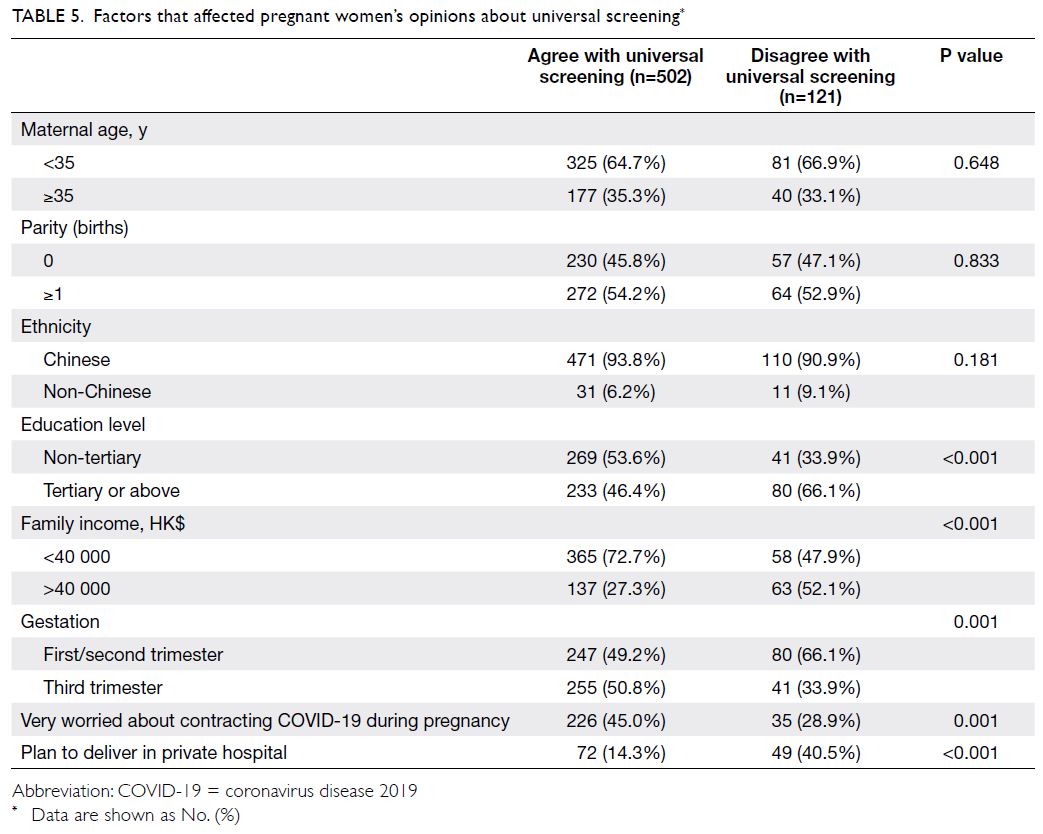
cohort and 91% in the 2014-2017 cohort. Table 1
shows the detailed characteristics, exposure, and
attitudes among the surveyed students. There was
no difference in gender between the 2007-2010
and 2014-2017 cohorts (odds ratio [OR]=1.14; 95%
CI=0.89-1.46).
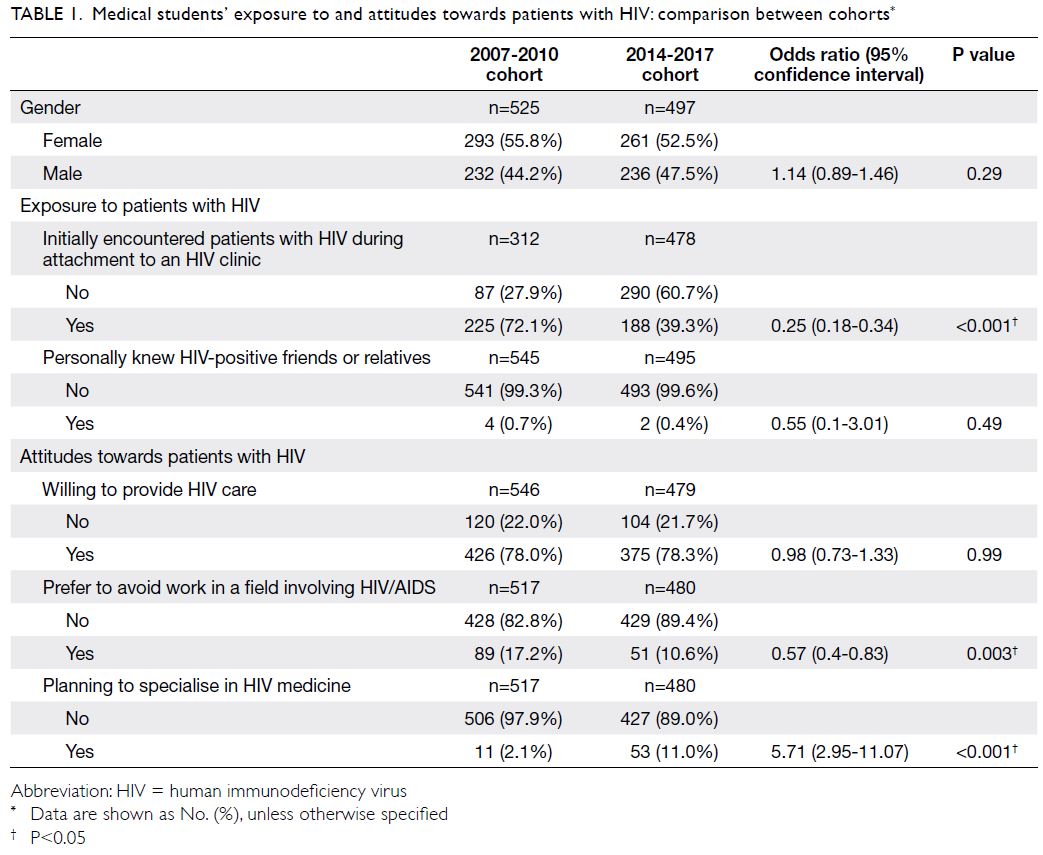
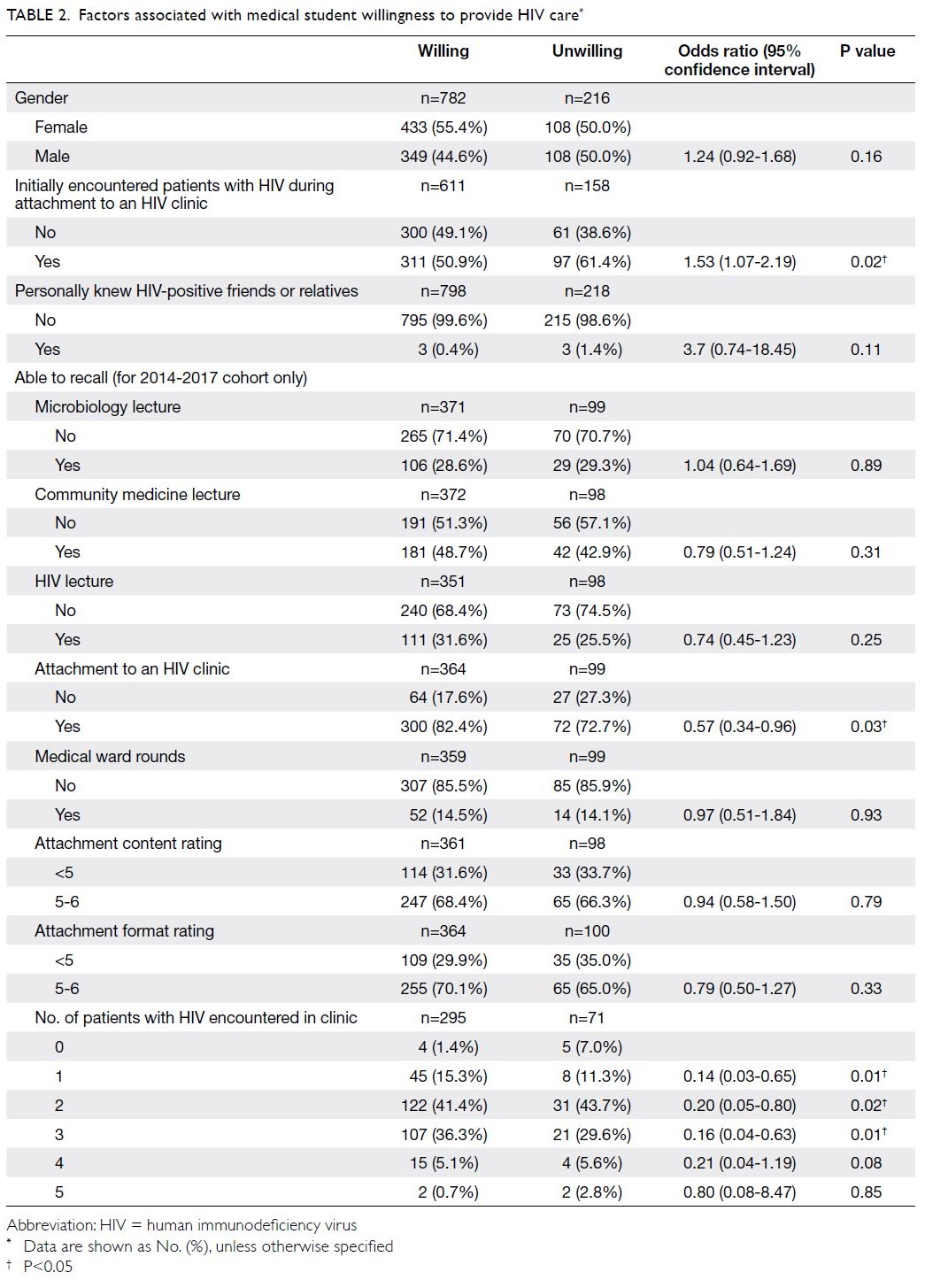
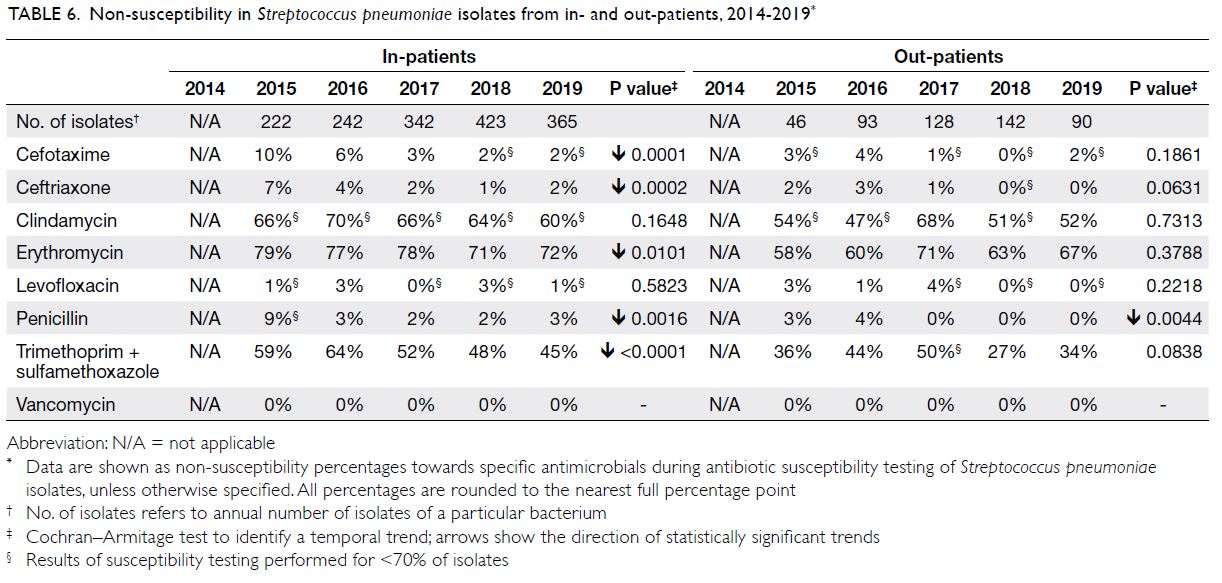
Table 1. Medical students’ exposure to and attitudes towards patients with HIV: comparison between cohorts
Participant exposure
Significantly fewer students (39.3%) in the mid-2010s initially encountered patients with HIV during
attachment to an HIV clinic, compared with students
in the late 2000s (72.1%; OR=0.25; 95% CI=0.18-0.34)
[Table 1]. The proportion of students who personally
knew HIV-positive friends or relatives remained low and did not significantly differ over time (OR=0.55;
95% CI=0.1-3.01). In the 2007-2010 and 2014-2017
cohorts, only four of 545 students (0.7%) and two of
495 students (0.4%), respectively, personally knew
HIV-positive friends or relatives.
Participant attitudes
Student willingness to provide HIV care was similar between cohorts (Table 1). Approximately 78% of
students were willing to provide care (OR=0.98;
95% CI=0.73-1.33). The proportion of students who
preferred to avoid work in a field involving HIV/AIDS significantly decreased over time: 17.2% in
the 2007-2010 cohort, compared with 10.6% in the
2014-2017 cohort (OR=0.57; 95% CI=0.4-0.83). An
increasing number of students planned to specialise
in clinical HIV treatment: 11 of 517 students (2.1%)
in the 2007-2010 cohort, compared with 53 of 480
students (11%) in the 2014-2017 cohort (OR=5.71;
95% CI=2.95-11.07).
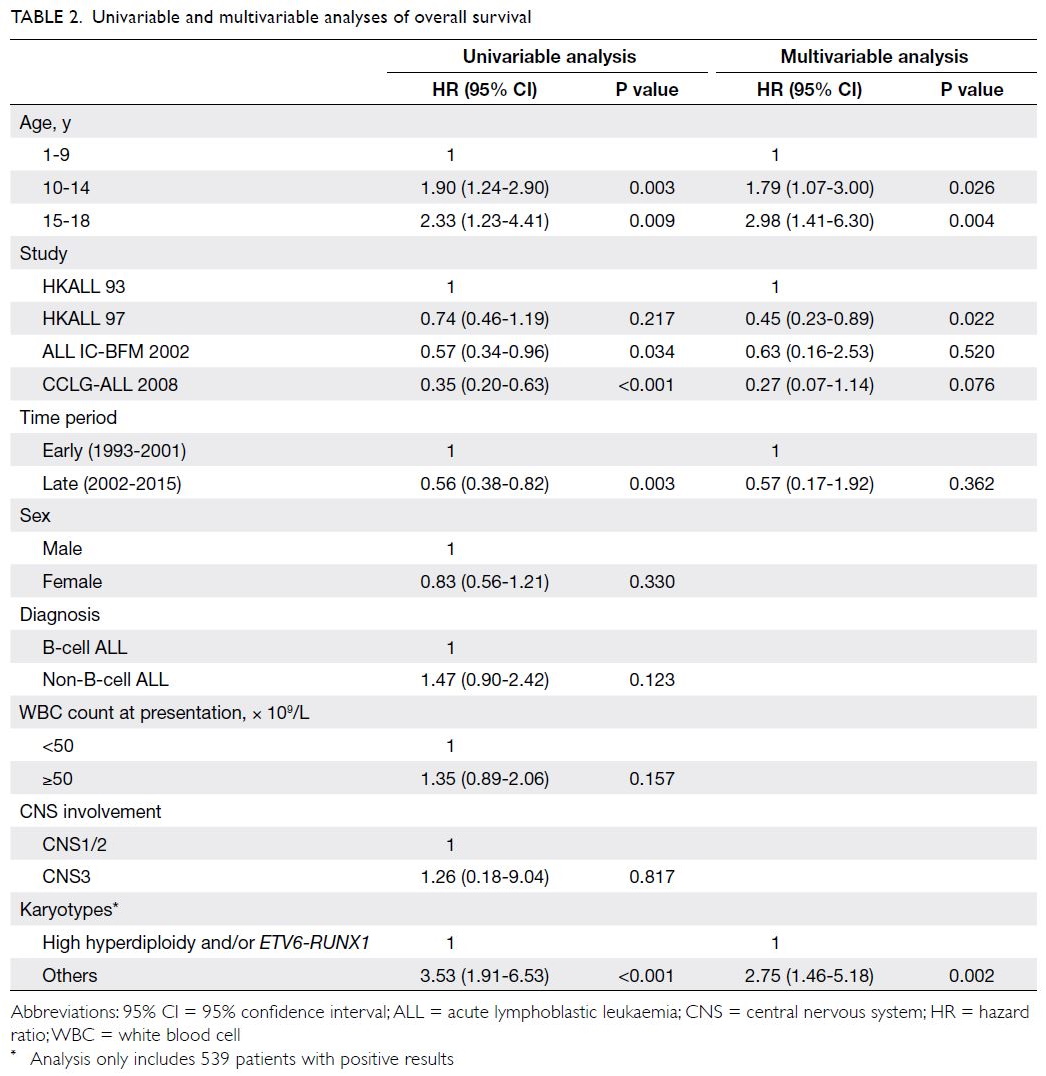
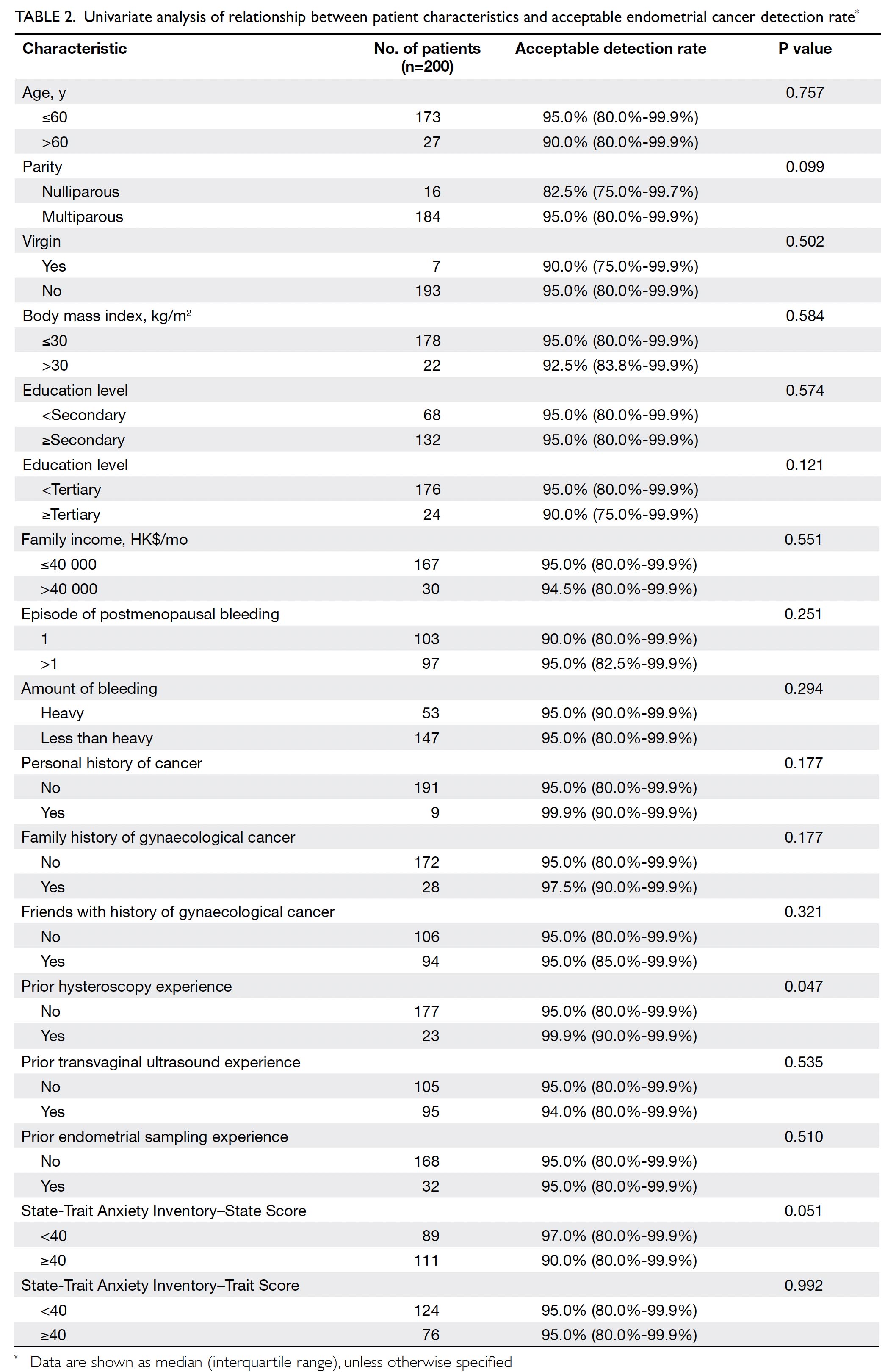
There was no difference in gender between
willing and unwilling students (OR=1.24;
95% CI=0.92-1.68) [Table 2]. Unwilling students were
more likely than willing students to have initially
encountered patients with HIV during attachment
to an HIV clinic (61.4% vs 50.9%) [OR=1.53;
95% CI=1.07-2.19]. Willingness was not associated
with personally knowing HIV-positive friends or
relatives. In the 2014-2017 cohort, most students
(80.3%) recalled their attachment to an HIV
clinic, whereas fewer than half could recall other
components of the HIV curriculum (lectures and
ward rounds; 14.5-48.7%). Notably, the ability to
recall attachment to an HIV clinic was associated
with willingness (OR=0.57; 95% CI=0.34-0.96)
to provide HIV care. Ratings of the content and
format of the attachment to an HIV clinic were not
associated with willingness (OR=0.94; 95% CI=0.58-1.50 and OR=0.79; 95% CI=0.50-1.27, respectively).
Overall, most students (97.5%) have encountered
>1 patient with HIV during clinical attachment.
Unwilling students (5/71, 7%) were less likely than
willing students (4/295, 1.4%) to have encountered
any patients with HIV during clinical attachment.
Discussion
Human immunodeficiency virus prevalence has
risen over time8 with advances in antiretroviral
therapy that contribute to prolonged survival; this
pattern has been observed in nearly all countries,
irrespective of the initial HIV prevalence. Thus,
it is unsurprising that exposure to patients with
HIV/AIDS increased over time among medical
students in our study. Nevertheless, Hong Kong
remains a low prevalence setting for HIV/AIDS9;
therefore, the number of students who personally
knew HIV-positive friends or relatives has remained
low. Despite predictable trends in exposure to patients with HIV since the late 2000s, some students
maintained negative attitudes towards patients with
HIV. Although exposure to patients with HIV has
increased, the proportion of students unwilling to
provide HIV care did not change between the late
2000s and middle 2010s. The proportion of unwilling
students in our study is higher than that in a similar
study conducted in 2011 in Malaysia, where 10% to
15% of students reported unwillingness to provide
HIV care.10 Because medical students are future
healthcare providers, their unwillingness to provide
HIV care represents an extreme manifestation
of stigma, which has been a problem since the
HIV/AIDS epidemic began.11
Stigma can have subtle effects, which may
influence career choices. A previous study found
that these effects can diminish over time12; our
results are consistent with that finding. While a large
proportion of students did not plan to work in a field
involving HIV, such plans may be related to personal
preferences for medical disciplines that facilitate
career development and job opportunities, although
discrimination cannot be ruled out. However, the
present study showed that, over time, fewer students
have reported that they prefer to avoid working in a
field involving HIV/AIDS. Encouragingly, increasing
numbers of students are planning to specialise in
clinical HIV treatment. “Interest” has been most
frequently cited as the main reason for choosing
a specialty; thus, interest in HIV/AIDS may be
increasing among medical students.13 However, the
proportion of students who intended to specialise in
clinical HIV treatment was lower in our study than
in a previous study in the United Kingdom, where
8% to 24% of students reported such an intention.14
Clinical attachment with patient exposure
appears to be an effective learning experience. In the
current system, some students may have overlooked
and missed the opportunity to encounter a patient
with HIV/AIDS. We found that, compared with
willing students, a higher proportion of students
unwilling to provide HIV/AIDS care had not
encountered a patient with HIV/AIDS during their
clinical attachment. This difference may be attributed
to a lack of exposure to patients with HIV/AIDS
during the medical school curriculum. Students
may benefit from repeated exposure to patients with
HIV/AIDS in different settings—willing students
were more likely to have previously encountered a
patient with HIV/AIDS. Further research is needed
to determine whether students could be exposed
to patients with HIV outside clinical settings (eg,
through non-governmental organisations) and to
understand the impacts of such exposure. Willing
students were more likely to recall their attachment
to an HIV clinic, compared with other teaching
methods; this suggests that their emotions were
aroused, which prompted recall.15
Previous research has shown that teaching
methods with experiential, small group, or affective
components and role models of positive attitudes
can effectively change students’ attitudes.14 Such considerations may be useful in clinics where small
numbers of students observe patient management
by a specialist physician. If a student is emotionally
affected by a patient or sees the clinician as a good role model, the clinical attachment may constitute a
memorable experience. This may be more important
than gaining technical knowledge and skills through
the clinical attachment experience because content
and format were not associated with willingness to
provide HIV care. Our results are consistent with
the findings of previous studies, which showed that
frequent clinical exposure to patients with HIV/AIDS
led to more positive attitudes.14 16 17 18 19 20 Furthermore,
knowledge alone cannot effectively decrease HIV
stigma21; similarly, we found that the ability to
recall lectures was not associated with willingness
to provide care for patients with HIV/AIDS.
However, increased exposure alone may be
insufficient to combat HIV stigma. Antibias
information is also needed to reduceprejudice,22
such as homophobia, which has been associated
with unwillingness to provide care for patients with
AIDS.12 Medical training should address these issues
that contribute to stigma towards patients with
HIV/AIDS. Notably, medical students reportedly
demonstrated increased willingness to provide
care for patients with HIV/AIDS after they had
attended an PLHIV sharing session or participated
in experiential games that were designed to increase
empathy towards PLHIV.23 In another study, HIV
stigma levels decreased in medical students after
exposure to an intervention that included discussion
of HIV stigma and other pre-existing related stigmas
(eg, homosexuality and illegal drug use).24
This study had some limitations. First, it was a comparison of cross-sectional surveys over a
10-year period and thus we were unable to assess
potential changes in attitudes among medical
students within a single cohort. Second, each cohort
used in comparative analysis was composed of three
annual cohorts; therefore, time intervals varied
among cohorts (eg, the 2007 and 2017 cohort were
separated by 10 years, whereas the 2010 and 2014
cohorts were separated by 4 years). Nevertheless,
we grouped cohorts together to maximise sample
size; our analysis clearly showed changes in attitudes
among medical students over time.
Conclusions
Despite more positive attitudes towards HIV/AIDS in terms of career choices, the willingness of medical
students to provide HIV care did not change between
the late 2000s and middle 2010s.
Interventions to reduce stigmatising attitudes
among towards PLHIV should be incorporated
in medical training; however, the framework for
medical school curriculum in Hong Kong makes
no mention of such interventions, although it
lists “attitudes and professionalism” as a core
competency.25 The medical school curriculum could
be updated to incorporate interventions that involve
experiential and affective teaching components to adequately address HIV stigma; additional clinical
attachments can ensure that medical students have
adequate exposure to patients with HIV.
Author contributions
Concept or design: G Tam, SS Lee.
Acquisition of data: SS Lee.
Analysis or interpretation of data: NS Wong.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: SS Lee.
Analysis or interpretation of data: NS Wong.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
The authors declare that they have no competing interests.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Survey and Behavioural
Research Ethics Committee, The Chinese University of Hong
Kong (Ref 12-01-2011). Participation was voluntary and
completion of the survey implied consent to participate in the
study. All data were anonymised and confidential.
References
1. Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A
systematic review of interventions to reduce HIV-related
stigma and discrimination from 2002 to 2013: how far have
we come? J Int AIDS Soc 2013;16(3 Suppl 2):18734. Crossref
2. US Department of State. The United States President’s
emergency plan for AIDS relief. Available from: https://www.pepfar.gov/documents/organization/201386.pdf.
Accessed 7 Jun 2022.
3. Schwartländer B, Stover J, Hallett T, et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet 2011;377:2031-41. Crossref
4. International Health Policy Program (IHPP), Ministry
of Public Health, Thailand. Report of a Pilot: Developing
Tools and Methods to Measure HIV-related Stigma and
Discrimination in Health Care Settings in Thailand.
Thailand: IHPP, Ministry of Public Health; 2014.
5. Scientific Committee on AIDS and STI (SCAS) Centre for
Health Protection Department of Health. Recommended
principles and practice of HIV clinical care in Hong Kong.
Hong Kong, 2016. Available from: https://www.chp.gov.hk/en/static/24003.html. Accessed 8 Jun 2022
6. The Lancet. The global HIV/AIDS epidemic—progress and
challenges. Lancet 2017;390:333. Crossref
7. Fettig J, Swaminathan M, Murrill CS, Kaplan JE. Global epidemiology of HIV. Infect Dis Clin North Am
2014;28:323-37. Crossref
8. Lee SS, Lam A, Lee KC. How prepared are our future doctors for HIV/AIDS? Public Health 2012;126:165-7. Crossref
9. Virtual AIDS Office of Hong Kong. HIV/AIDS Statistics in
Hong Kong 1984-June 2020. Available from: http://www.info.gov.hk/aids/english/surveillance/cumhivaids.jpg.
Accessed 8 Jun 2022.
10. Ahmed SI, Hassali MA, Bukhari NI, Sulaiman SA. A
comparison of HIV/AIDS related knowledge, attitudes and
risk perceptions between final year medical and pharmacy
students: a cross sectional study. Healthmed 2011;5:317-25.
11. Radecki S, Shapiro J, Thrupp LD, Gandhi SM, Sangha SS,
Miller RB. Willingness to treat HIV-positive patients at
different stages of medical education and experience. AIDS
Patient Care STDS 1999;13:403-14. Crossref
12. Kopacz DR, Grossman LS, Klamen DL. Medical students
and AIDS: knowledge, attitudes and implications for
education. Health Educ Res 1999;14:1-6. Crossref
13. Wu SM, Chu TK, Chan ML, Liang J, Chen JY, Wong SY. A
study on what influence medical undergraduates in Hong
Kong to choose family medicine as a career. Hong Kong
Pract 2014;36:123-9.
14. Ivens D, Sabin C. Medical student attitudes towards HIV.
Int J STD AIDS 2006;17:513-6. Crossref
15. Storbeck J, Clore GL. Affective arousal as information:
how affective arousal influences judgments, learning, and
memory. Soc Personal Psychol Compass 2008;2:1824-43. Crossref
16. Syed IA, Hassali MA, Khan TM. General knowledge &
attitudes towards AIDS among final year medical and
pharmacy students. Folia Medica 2010;45:9-13.
17. Mohsin S, Nayak S, Mandaviya V. Medical students’
knowledge and attitudes related to HIV/AIDS. Natl J
Community Med 2010;1:146-9.
18. Tešić V, Kolarić B, Begovac J. Attitudes towards HIV/AIDS among four year medical students at the University of Zagreb Medical School—better in 2002 than in 1993 but
still unfavorable. Coll Antropol 2006;30:89-97.
19. Sanchez NF, Rabatin J, Sanchez JP, Hubbard S, Kalet A.
Medical students’ ability to care for lesbian, gay, bisexual,
and transgendered patients. Fam Med 2006;38:21-7.
20. Umeh CN, Essien EJ, Ezedinachi EN, Ross MW. Knowledge,
beliefs and attitudes about HIV/AIDS-related issues, and
the sources of knowledge among health care professionals
in southern Nigeria. J R Soc Promot Health 2008;128:233-9. Crossref
21. Liu X, Erasmus V, Wu Q, Richardus JH. Behavioral
and psychosocial interventions for HIV prevention in
floating populations in China over the past decade: a
systematic literature review and meta-analysis. PLoS One
2014;9:e101006. Crossref
22. Aboud FE, Tredoux C, Tropp LR, Brown CS, Niens U,
Noor NM, Una Global Evaluation Group. Interventions
to reduce prejudice and enhance inclusion and respect for
ethnic differences in early childhood: a systematic review.
Dev Rev 2012;32:307-36. Crossref
23. Mak WW, Cheng SS, Law RW, Cheng WW, Chan F.
Reducing HIV-related stigma among health-care
professionals: a game-based experiential approach. AIDS
Care 2015;27:855-9. Crossref
24. Varas-Díaz N, Neilands TB, Cintrón-Bou F, et al. Testing
the efficacy of an HIV stigma reduction intervention with
medical students in Puerto Rico: the SPACES project. J Int
AIDS Soc 2013;16(3 Suppl 2):18670. Crossref
25. The Medical Council of Hong Kong. Hong Kong doctors.
2017. Available from: https://www.mchk.org.hk/english/publications/files/HKDoctors.pdf. Accessed 8 Jun 2022.