Hong Kong Med J 2022 Apr;28(2):124–32 | Epub 14 Apr 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Knowledge, attitudes, and behaviours of pregnant
women towards COVID-19: a cross-sectional survey
WY Lok, FHKAM (Obstetrics and Gynaecology), FHKCOG; CY Chow, MB, ChB; CW Kong, FHKAM (Obstetrics and Gynaecology), FHKCOG; William WK To, FHKAM (Obstetrics and Gynaecology), FHKCOG
Department of Obstetrics and Gynaecology, United Christian Hospital, Hong Kong
Corresponding author: Dr WY Lok (happyah2@hotmail.com)
Abstract
Introduction: This study investigated the knowledge,
attitudes, and behaviours of pregnant women
towards coronavirus disease 2019 (COVID-19),
as well as obstetric services provided by public
hospitals (eg, universal screening) during the
pandemic.
Methods: This cross-sectional survey was
performed in the antenatal clinics of Kowloon East
Cluster, Hospital Authority. Questionnaires were
distributed to pregnant women for self-completion
during follow-up examinations.
Results: In total, 623 completed questionnaires
were collected from 28 July 2020 to 13 August 2020.
Within this cohort, 83.1% of the women expressed
high levels of worry (41.9% very worried and 41.3%
worried) about contracting COVID-19 during
pregnancy, 70.5% believed that maternal COVID-19
could cause intrauterine infection of their fetuses,
and 84.3% objected to banning husbands from
accompanying wives during labour and delivery.
Most women (80.6%) agreed with universal screening
for COVID-19 at certain points during pregnancy.
Logistic regression modelling showed that women
who were very worried about contracting COVID-19 (P=0.005) and women in their third trimester of
pregnancy (P=0.009) were more likely to agree with
universal screening during pregnancy; women with
higher income (P=0.017) and women who planned
to deliver in a private hospital (P=0.024) were more
likely to disagree with such screening.
Conclusion: Pregnant women expressed high levels
of worry about contracting COVID-19 during
pregnancy; universal screening during pregnancy
was acceptable to a large proportion of our
participants. Efforts should be made to specifically
include pregnant women when launching any
population screening programme for COVID-19.
New knowledge added by this study
- This study investigated the knowledge, psychosocial behavioural responses, and opinions of pregnant women in Hong Kong towards coronavirus disease 2019 (COVID-19).
- A large majority of the women in this study expressed worry about COVID-19, despite a lack of comprehensive knowledge about the disease.
- More than 80% of the women agreed with universal screening for COVID-19 in pregnant women during visits to clinics and hospitals.
- Universal screening should be incorporated as part of routine clinical management and in-patient care for pregnant women during the COVID-19 pandemic.
- Husbands should be allowed to accompany their wives during labour and delivery if a rapid screening method shows that the husbands do not have COVID-19.
- Online resources should be developed to enhance public knowledge about COVID-19-related complications in pregnancy.
Introduction
Coronavirus disease 2019 (COVID-19), caused by
severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2), has been a worldwide pandemic
for more than 2 years. The first reported case of
COVID-19 occurred in Wuhan, China in late
December 2019.1 2 On 21 January 2020, the first confirmed imported case of COVID-19 in Hong
Kong was identified in a mainland Chinese tourist
who arrived from Wuhan by high-speed rail.3
The dynamics of the current COVID-19
pandemic closely resemble the previous SARS
epidemic because each has involved a respiratory
disease caused by a coronavirus. Despite various measures and strategies employed by the Hong Kong
government and the public in an effort to combat
viral spread, a third wave of infections occurred in
the middle of 2020, leading to >100 new confirmed
COVID-19 cases daily for 12 days consecutively
in late July 2020.4 In response, the government
announced a variety of new measures to contain the
spread of COVID-19.
Pregnant women in Hong Kong are particularly
worried about the effects of COVID-19 because of
their vulnerable immune status during pregnancy,
as well as the fear of vertical transmission to the
neonate.5 6 During the 2003 SARS epidemic in Hong
Kong, 12 pregnant women contracted SARS and three
died. Among the survivors, SARS was associated with
poor outcomes including high rates of mechanical
ventilation and intensive care unit admission, as well
as spontaneous miscarriage, preterm delivery, and
intrauterine growth restriction. However, there was
no evidence of perinatal transmission of SARS to
infants.7 In early 2020, the first reports of COVID-19
in Chinese pregnant women were published.8 9
Systematic reviews concerning maternal and
perinatal outcomes in cases of COVID-19 have since
been published.10 11 12 13
To our knowledge, no studies have specifically
assessed the basic knowledge and concerns of
pregnant women with respect to COVID-19,
or their acceptance of universal screening for
infection by the causative virus (SARS-CoV-2);
such information is important for the establishment
of public education campaigns and launching
COVID-19 population screening efforts that target pregnant women. This study aimed to evaluate the
opinions of pregnant women concerning obstetric
services provided during the pandemic, with
particular focus on acceptance of universal screening
for COVID-19 during pregnancy. The study also
explored the knowledge, attitudes, and behaviours of
pregnant women towards the COVID-19 pandemic.
Methods
This cross-sectional survey was conducted in two
antenatal clinics in the Kowloon East Cluster of
Hong Kong. The questionnaires were distributed
to consecutive pregnant women who attended
antenatal follow-up examinations in the two clinics
from July 2020 to August 2020.
The paper questionnaires were anonymous,
self-administered, and available in either Chinese
or English. The first section of the questionnaire
collected basic demographic data from the recruited
women. The remaining sections comprised four
domains with 31 total questions; five questions had
multiple parts. The four domains included questions
regarding (1) knowledge of COVID-19 in pregnancy,
(2) attitudes towards COVID-19, (3) social
behaviours during the COVID-19 pandemic, and (4)
opinions about the provision of obstetric services
during the COVID-19 pandemic. The questions were
answered in the following formats (as appropriate):
binary (Yes/No), three options (Yes/No/unsure),
4-point Likert scale, or selection of available answers
(online supplementary Appendix).
The study protocol was approved by the
Research Ethics Committee of Kowloon East Cluster,
Hospital Authority. SPSS software (Windows version
20.0; IBM Corp, Armonk [NY], United States)
was used for data entry and analysis. Descriptive
categorical data were expressed as numbers and
percentages; they were compared and analysed by the
Chi squared test or Fisher’s exact test as appropriate.
Multivariate logistic regression analysis was used
to identify clinical covariates that were significantly
associated with pregnant women’s opinions about
universal screening for COVID-19. A P value of
<0.05 was considered statistically significant.
Results
Participants
The questionnaires were distributed to 700
pregnant women for 17 days, from 28 July 2020
to 13 August 2020. Seven women were excluded
because they could not understand either version
of the questionnaire (ie, Chinese or English), while
54 women refused to participate in the study. Of
the 639 women who completed the questionnaire,
16 were excluded because of missing answers; thus,
623 participants were included in the final analysis.
Nearly all participants were Chinese (93.3%). Half of the participants (50.2%) had an education level of
tertiary or above; 47.5% were in the third trimester of
pregnancy (Table 1).
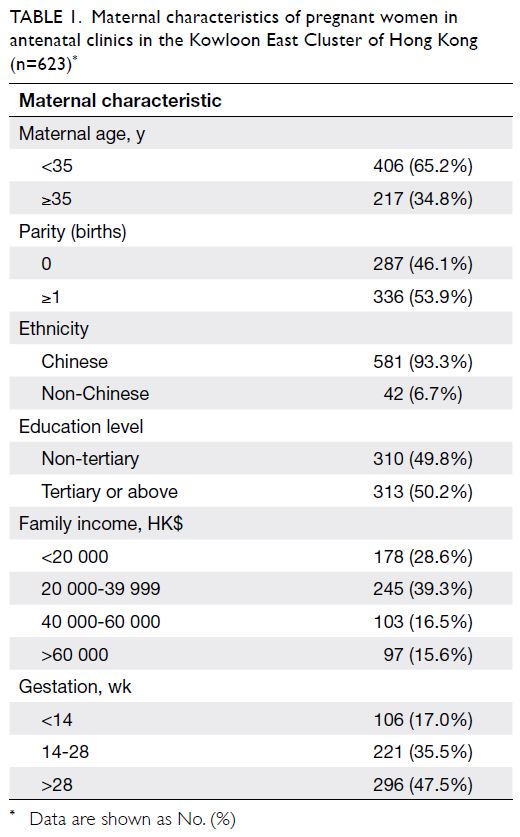
Table 1. Maternal characteristics of pregnant women in antenatal clinics in the Kowloon East Cluster of Hong Kong (n=623)
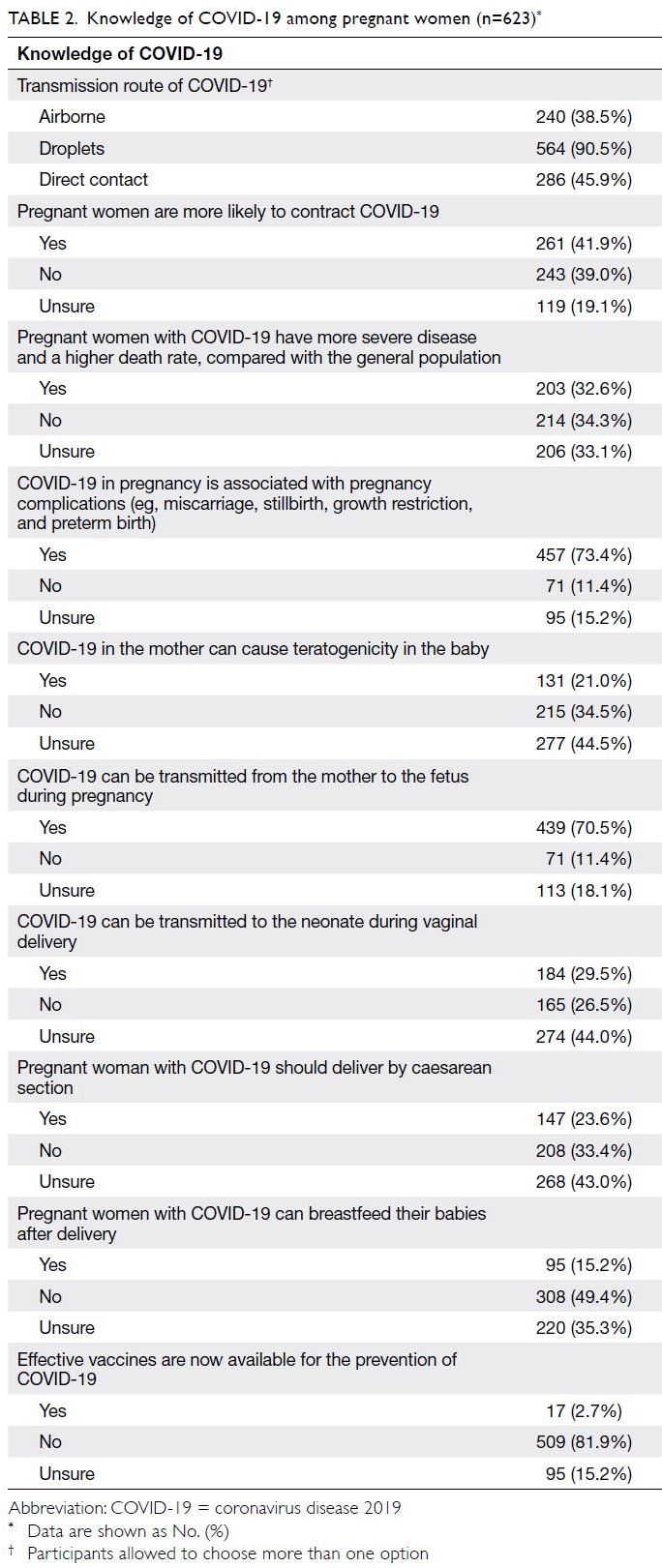
Knowledge of COVID-19 in pregnancy
A large proportion of the participants (90.5%)
knew that COVID-19 was transmitted by droplets,
while more than one-third of participants (38.5%)
thought that airborne transmission of COVID-19
was also possible. Additionally, more than one-third
of participants (41.9%) thought that they were
more likely to contract COVID-19, while 32.6%
presumed that pregnant women with COVID-19
would have more severe disease and experience
higher mortality rates compared with the general
population. Moreover, 73.4% of participants
thought that maternal COVID-19 was associated
with pregnancy complications such as miscarriage,
stillbirth, growth restriction, and preterm birth;
70.5% believed that maternal COVID-19 could be
vertically transmitted to the fetus during pregnancy.
Substantial proportions of participants were unsure
whether COVID-19 in pregnant women could lead
to teratogenicity in the fetus (44.5%), or whether
women with COVID-19 should be able to perform
vaginal delivery (44%) or breastfeed (35.3%) [Table 2].
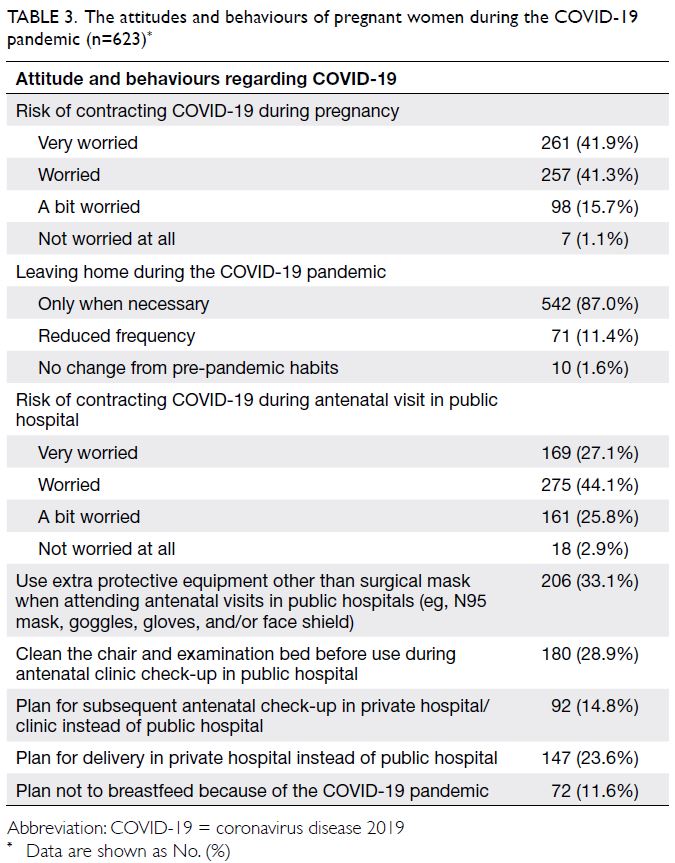
Attitudes and behaviours of pregnant women
during the COVID-19 pandemic
The majority (83.1%) of participants were worried
about contracting COVID-19 during pregnancy
(41.9% were very worried and 41.3% were worried).
Similarly, 87.0% of participants only left home
when necessary during the pandemic, while 71.3%
of participants were worried about contracting
COVID-19 during their antenatal visits in public
hospitals (27.1% were very worried and 44.1% were
worried). One-third of the participants (33.1%) used
extra protective gear other than surgical masks when
attending antenatal clinics (eg, N95 masks, goggles,
gloves, or face shields), while 28.9% of participants
reported cleaning the chair and examination bed
with disinfectants before use during an antenatal
clinic visit. Almost one-quarter of participants
(23.6%) intended to deliver in a private hospital,
among which 49.7% (73/147) believed that the risk of
contracting COVID-19 was lower when delivering in
a private hospital than in a public hospital. Moreover,
61.2% of participants who intended to deliver in a
private hospital (90/147) stated that public hospitals no longer permitted husbands to accompany wives
during labour and delivery during the COVID-19
pandemic, while private hospitals continued to allow
such practices. Seventy-two participants (11.6%)
decided not to breastfeed because of the COVID-19
pandemic, of which 77.8% (56/72) believed that
COVID-19 could be transmitted to the baby through
breast milk even if the mother had asymptomatic
illness (Table 3).
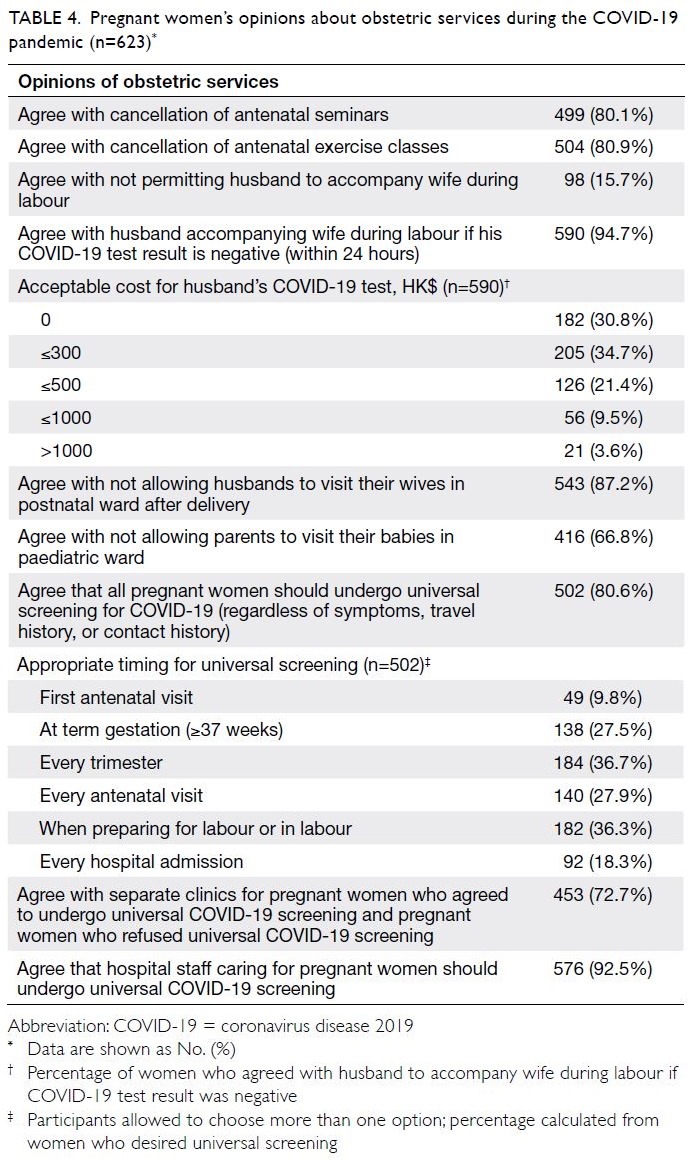
Opinions about the provision of obstetric
services during the COVID-19 pandemic
Most participants agreed that antenatal seminars
and antenatal exercise classes should be cancelled,
and that visitors should not be allowed in postnatal
wards and neonatal wards (including husbands and
parents). However, a large proportion of participants
(84.3%) objected to banning husbands from
accompanying wives during labour and delivery
in the COVID-19 pandemic; 94.7% of participants
agreed that husbands a with negative COVID-19
test results should be allowed to accompany wives
during labour, and 65.6% agreed with paying for
such a test if the price was ≤HK$300. While 80.6%
of participants agreed that pregnant women should
undergo universal screening for COVID-19 during
pregnancy, their preferences varied regarding the
optimal time to perform such screening. The most
popular option was screening in every trimester
(36.7%), followed by screening when preparing for
labour or in labour (36.3%). Almost all participants
(92.5%) agreed that hospital staff caring for pregnant
women should undergo regular universal COVID-19
screening (Table 4).
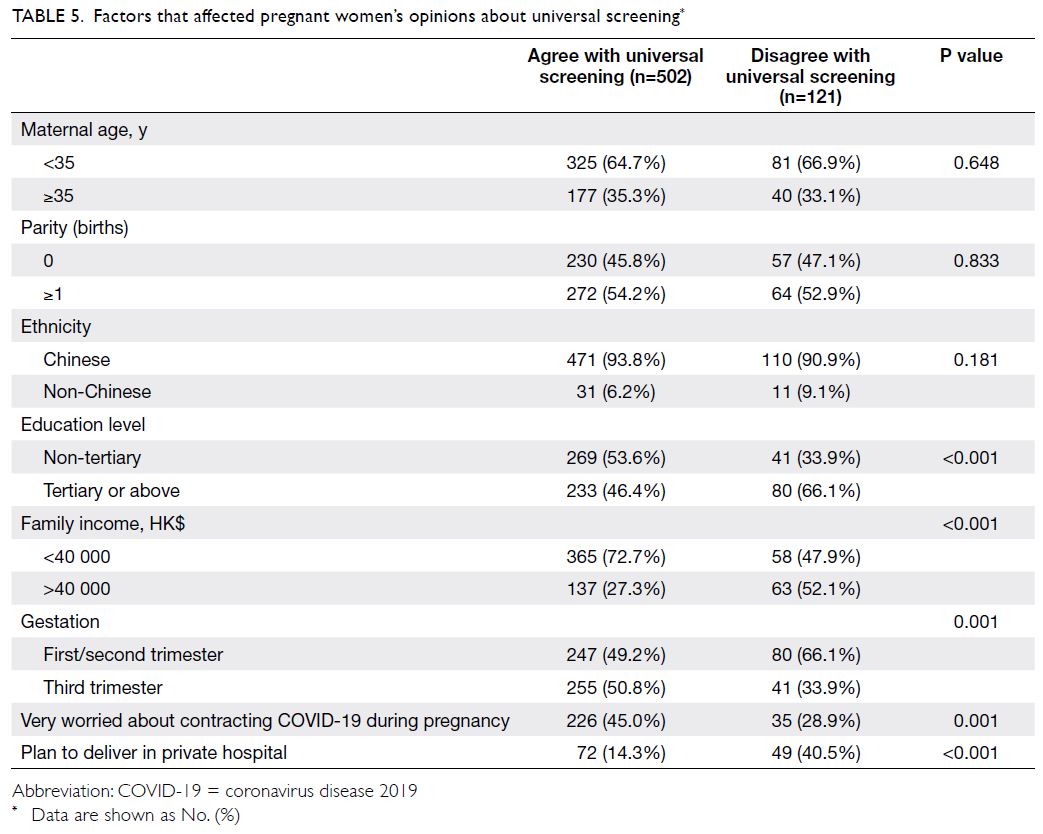
Factors that affect pregnant women’s
opinions about universal screening for COVID-19
Univariate analysis showed that a significantly
greater proportion of women who agreed with
universal screening had family income <$40 000
(72.7% vs 47.9%, P<0.001), were very worried about
contracting COVID-19 during pregnancy (45.0%
vs 28.9%, P=0.001), or were in their third trimester
(50.8% vs 33.9%, P=0.001). Conversely, women who
did not agree with screening were more likely to
have an education level of tertiary or above (46.4% vs
66.1%, P<0.001) and intended to deliver in a private
hospital (14.3% vs 40.5%, P<0.001). However, no
differences were observed in terms of parity, ethnicity,
or the proportion of women with advanced maternal
age between women who did and did not agree with
universal screening (Table 5). Logistic regression
analysis showed that women who were very worried
about contracting COVID-19 (P=0.005, odds ratio
[OR]=1.89) and women in their third trimester of
pregnancy (P=0.009, OR=1.77) were more likely to agree with universal screening during pregnancy;
women with family income >$40 000 (P=0.017,
OR=0.55) and women who planned to deliver in a
private hospital (P=0.024, OR=0.57) were more likely
to disagree with such screening. Education level was
not a significant risk factor according to multivariate
analysis (Table 6).
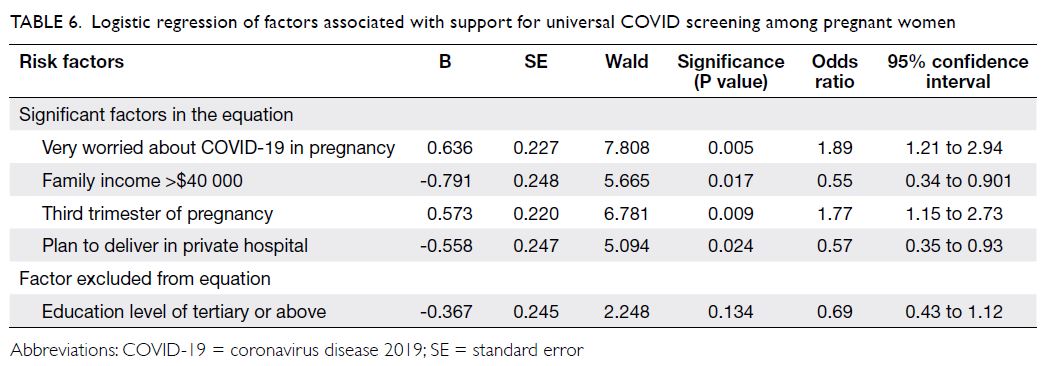
Table 6. Logistic regression of factors associated with support for universal COVID screening among pregnant women
Discussion
To our knowledge, this is the first large study
in Hong Kong concerning the knowledge and
psychobehavioural responses of pregnant women
towards the COVID-19 pandemic. While basic
concepts concerning COVID-19 appeared to be
understood by our study participants (eg, COVID-19
is primarily spread through droplets and that
vaccines were not available at the time of the study),
there was the potential for improved knowledge
regarding other concepts. For instance, there is
evidence that, compared with the general population,
pregnant women are not more susceptible to
contract COVID-19 and the majority of them do
not experience severe complications of COVID-19
in pregnancy; however, it has been suggested that
pregnant women may be at higher risk of more
severe disease than the non-pregnant women in
terms of intensive care unit admission particularly
when they are in the third trimester.14 In a systematic
review, the rate of severe pneumonia in pregnant
women with COVID-19 ranged from 0% to 14%;
sporadic maternal death was reported in case reports
of patients with severe COVID-19.10 Furthermore, approximately 70% of women in our cohort thought
that maternal COVID-19 led to increased pregnancy
complications and carried a high rate of vertical
transmission, more evidence in these areas are
now emerging. Systematic reviews have shown
that there could be increased risks of miscarriage
and stillbirths in pregnant women with COVID-19;
and pregnant women with symptomatic infection
had two-to-three-fold increased risks of preterm
birth, most of these were iatrogenic.12 13 In contrast,
there is no evidence showing increased risk for
teratogenicity or intrauterine growth restriction of
baby with maternal COVID-19 infection.15 The risks
of vertical transmission of COVID-19, which despite
remaining controversial, has now been supported
by systematic reviews.16 Online resources, such as
websites or mobile apps, should be considered to
provide updated information regarding the effects of
COVID-19 on pregnancy.
Our pregnant women demonstrated
uncertainties concerning the mode of delivery and
breastfeeding should they contract COVID-19,
mainly because they feared disease transmission
during delivery or via breast milk. While the
literature has reported that vertical transmission
during vaginal delivery or in the peripartum period could be possible, the actual risks appeared to be
very low and caesarean may not prevent vertical
transmission.17 Indeed, vaginal delivery is not contra-indicated
although high rates of caesarean delivery
have been reported in studies, with up to 85.9% of
deliveries via caesarean section in a large series of
116 women with COVID-19 (38.8% had COVID-19
pneumonia).18 However, there has been conflicting
evidence regarding the safety of breastfeeding.19
According to the Centers for Disease Control and
Prevention guidelines, breastfeeding is not contra-indicated
when a mother contracts COVID-19 but
should be determined by the mother’s overall health status.20 Available data suggest that SARS-CoV-2 is
not detectable in breast milk samples from mothers
with COVID-19. While some authors have suggested
isolation of the mother and baby,21 a large series of 82
neonates roomed with mothers who had COVID-19
in a closed Giraffe isolette (with necessary contact
precautions during direct breastfeeding) showed
that these neonates remained free of COVID-19.22
A large majority of the pregnant women in
our cohort expressed worry about contracting
COVID-19 during pregnancy or antenatal follow-up
examinations in public hospitals. A survey of the
psychological and behavioural responses of pregnant
women during the SARS epidemic in Hong Kong
revealed that pregnant women had slightly greater
anxiety during SARS than before the epidemic.23 In addition to their memories of the SARS epidemic,
the widespread worry among pregnant women
in our cohort could be explained by the timing of
our survey, which was conducted during a wave of
COVID-19 transmission in Hong Kong. We might
have been able to partially alleviate their fears if we
had stated that the World Health Organization’s
provisional case fatality rate of COVID-19 was 3.7%
during the study period, considerably lower than the
10% of SARS.24 A substantial proportion of pregnant
women (approximately 20%) in our survey revealed
that they had considered subsequent follow-up
examinations and delivery in private hospitals, which
they believed to be safer; however, this proportion
might be an underestimation because women who
intended to deliver in a private hospital might not
have attended our clinics for any examinations.
More than 80% of women objected to banning
husbands from accompanying wives during
labour and delivery in the COVID-19 pandemic,
particularly if those husbands had negative
COVID-19 test results. Indeed, many women
reported considering delivery in a private hospital for
this reason. A previous study conducted in our unit
demonstrated that partner companionship during
labour could offer emotional support and enhance
maternal satisfaction during delivery.25 As extended
screening becomes available, husbands should be
offered the opportunity to undergo screening when
their wives are admitted for labour and delivery to
address this need for partner companionship.
Because COVID-19 is highly transmissible
and COVID-19 carriers may be asymptomatic,
universal screening of all patients is important to
curb disease spread in the community. In August
2020, the Hong Kong Government announced that
a voluntary universal COVID-19 testing programme
would be launched. In partnership with the Board
of Directors of Yan Chai Hospital, the government’s
trial community testing programme for COVID-19
among pregnant women was launched on 10 August
2020, although we did not have data regarding this
programme during our study. Around 1 month
after our study, the Hospital Authority extended the
COVID-19 screening to all asymptomatic in-patients
including pregnant women. Our survey showed that
approximately 80% of pregnant women agreed with
universal screening for COVID-19 in the hospital
setting. While their opinions differed concerning
the frequency and timing of screening, women in
the third trimester of pregnancy generally wanted to
confirm that they were COVID-19-free at the time of
delivery. However, it is understandable that women
with higher family income and women who intended
to deliver in a private hospital might not agree with
universal screening in public hospitals. In the
literature, universal screening for COVID-19 in
pregnant women has mainly focused on screening at the time of admission for delivery; this practice was
implemented as early as March 2020 in countries
where community prevalence rates were considered
high. Such universal screening has yielded prevalence
rates of 0.43% to 13.7% for asymptomatic COVID-19
in pregnant women, depending on the local
epidemiological situation.26 27 28 29 In the latest update, the
Royal College of Obstetricians and Gynaecologists
recommended all pregnant women admitted to
hospitals in England should be offered SARS-CoV-2
testing regardless of symptoms.30 Ideally, such
screening enables early identification and cohorting
of asymptomatic women with COVID-19, thus
protecting other pregnant women, their newborn
infants, and healthcare staff. Negative test results
can be used to reassure the women and encourage
them to practise breastfeeding. The inclusion of
universal screening for COVID-19 among pregnant
women should be a key aspect of maternity care
after considering the need for laboratory support,
availability of isolation facilities and personal
protective equipment, and (most importantly)
the cost-effectiveness of screening based on the
estimated community prevalence of COVID-19.
There were some limitations in this study.
While we performed a small pilot study (involving
face-to-face interviews) when designing and refining
the survey questions to confirm responses by
pregnant women, we did not conduct further formal
validation or assessment of internal reliability.
The questionnaires were developed around the
peak of the third wave in Hong Kong; the results
drawn from the survey reflected only the recruited
women’s knowledge and opinions at that time
point. Thus, our findings might not be generalisable
to other populations or other points in the
COVID-19 pandemic with different epidemiological
characteristics.
Conclusion
Among pregnant women, knowledge about COVID-19 during pregnancy should be strengthened
through public education that specifically focuses on
COVID-19-related complications in pregnancy. A
large majority of pregnant women expressed worry
about contracting COVID-19 during pregnancy,
and most women in the study agreed with universal
screening during pregnancy. While the optimal
timing for screening in pregnancy requires further
consideration, there is a need to specifically
include pregnant women in population screening
programmes for COVID-19.
Author contributions
Concept or design: WY Lok, CW Kong, WWK To.
Acquisition of data: WY Lok, CY Chow.
Analysis or interpretation of data: WY Lok, CW Kong, WWK To.
Drafting of the manuscript: WY Lok, CW Kong.
Critical revision of the manuscript for important intellectual content: All authors
Acquisition of data: WY Lok, CY Chow.
Analysis or interpretation of data: WY Lok, CW Kong, WWK To.
Drafting of the manuscript: WY Lok, CW Kong.
Critical revision of the manuscript for important intellectual content: All authors
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was obtained from the Kowloon Central/Kowloon East Research Ethics Committees (Ref: KC/KE-20-
0226/ER-3).
References
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med
2020;382:727-33. Crossref
2. Huang C, Wang Y, Li X, et al. Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China.
Lancet 2020;395:497-506. Crossref
3. Cheung E. China Coronavirus: death toll almost doubles
in one day as Hong Kong reports its first two cases. South
China Moring Post. 2020 Jan 22. Available from: https://www.scmp.com/news/hong-kong/health-environment/article/3047193/china-coronavirus-first-case-confirmed-hong-
kong. Accessed 16 Aug 2020.
4. Ting V, Leung K, Cheung E. Hong Kong third wave: city’s
Covid-19 social-distancing measures set to be extended
after recent spike in cases. South China Moring Post.
2020 Aug 1. Available from: https://www.scmp.com/news/hongkong/healthenvironment/article/3095642/hong-kong-third-wave-more-100-new-covid-19-cases. Accessed 16 Aug 2020.
5. Dashraath P, Wong JL, Lim MX, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet
Gynecol 2020;222:521-31. Crossref
6. Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID-19) and
pregnancy: what obstetricians need to know. Am J Obstet
Gynecol 2020;222:415-26. Crossref
7. Wong SF, Chow KM, Leung TN, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory
syndrome. Am J Obstet Gynecol 2004;191:292-7. Crossref
8. Schwartz DA. An analysis of 38 pregnant women with
COVID-19, their newborn infants, and maternal-fetal
transmission of SARS-CoV-2: maternal coronavirus
infections and pregnancy outcomes. Arch Pathol Lab Med
2020;144:799-805. Crossref
9. Chen H, Guo J, Wang C, et al. Clinical characteristics and
intrauterine vertical transmission potential of COVID-19
infection in nine pregnant women: a retrospective review
of medical records. Lancet 2020;395:809-15. Crossref
10. Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC. Effect
of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: systematic review.
Ultrasound Obstet Gynecol 2020;56:15-27. Crossref
11. Zaigham M, Andersson O. Maternal and perinatal
outcomes with COVID-19: a systematic review of 108
pregnancies. Acta Obstet Gynecol Scand 2020;99:823-9. Crossref
12. Kazemi SN, Hajikhani B, Didar H, et al. COVID-19 and
cause of pregnancy loss during the pandemic: a systematic
review. PLoS One 2021;16:e0255994. Crossref
13. Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact
of COVID-19 on pregnancy outcomes: a systematic review
and meta-analysis. CMAJ 2021;193:E540-8. Crossref
14. Vousden N, Bunch K, Morris E, et al. The incidence,
characteristics and outcomes of pregnant women
hospitalized with symptomatic and asymptomatic SARS-CoV-
2 infection in the UK from March to September 2020:
a national cohort study using the UK Obstetric Surveillance
System (UKOSS). PLoS One 2021;16:e0251123. Crossref
15. Mullins E, Hudak ML, Banerjee J, et al. Pregnancy and
neonatal outcomes of COVID-19: coreporting of common
outcomes from PAN-COVID and AAP-SONPM registries.
Ultrasound Obstet Gynecol 2021;57:573-81. Crossref
16. Musa SS, Bello UM, Zhao S, Abdullahi ZU, Lawan MA,
He D. Vertical transmission of SARS-CoV-2: a systematic
review of systematic reviews. Viruses 2021;13:1877. Crossref
17. Sinaci S, Ocal DF, Seven B, et al. Vertical transmission of
SARS-CoV-2: a prospective cross-sectional study from a
tertiary center. J Med Virol 2021;93:5864-72. Crossref
18. Yan J, Guo J, Fan C, et al. Coronavirus disease 2019 in
pregnant women: a report based on 116 cases. Am J Obstet
Gynecol 2020;223:111.e1-14. Crossref
19. Poon LC, Yang H, Kapur A, et al. Global interim guidance
on coronavirus disease 2019 (COVID-19) during
pregnancy and puerperium from FIGO and allied partners:
information for healthcare professionals. Int J Gynecol
Obstet 2020;149:273-86. Crossref
20. Centers for Disease Control and Prevention. Care for
breastfeeding people. Interim guidance on breastfeeding
and breast milk feeds in the context of COVID-19.
Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/care-for-breastfeeding-women.html. Accessed 11 Aug 2020.
21. Griffin I, Benarba F, Peters C, et al. The impact of
COVID-19 infection on labor and delivery, newborn
nursery, and neonatal intensive care unit: prospective
observational data from a single hospital system. Am J
Perinatol 2020;37:1022-30. Crossref
22. Salvatore CM, Han JY, Acker KP et al. Neonatal
management and outcomes during the COVID-19
pandemic: an observation cohort study. Lancet Child
Adolesc Health 2020;4:721-7. Crossref
23. Lee DT, Sahotab D, Leung TN, Yip AS, Lee FF, Chung TK.
Psychological responses of pregnant women to an
infectious outbreak: a case-control study of the 2003 SARS
outbreak in Hong Kong. J Psychosom Res 2006;61:707-13. Crossref
24. World Health Organization. Coronavirus disease
(COVID-2019) situation reports-204. Available from:
https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200811-covid-19-sitrep-204.pdf?sfvrsn=1f4383dd_2. Accessed 12 Aug 2020.
25. Chung VW, Chiu JW, Chan DL, To WW. Companionship
during labour promotes vaginal delivery and enhances
maternal satisfaction. Hong Kong J Gynaecol Obstet
Midwifery 2017;17:12-7.
26. Sutton D, Fuchs K, D’Alton M, Goffman D. Universal
screening for SARS-CoV-2 in women admitted for delivery.
N Engl J Med 2020;382:2163-4. Crossref
27. Fassett MJ, Lurvey LD, Yasumura L, et al. Universal
SARS-Cov-2 screening in women admitted for delivery
in a large managed care organization. Am J Perinatol
2020;37:1110-4. Crossref
28. Tanacana A, Erola SA, Turgay B, et al. The rate of
SARS-CoV-2 positivity in asymptomatic pregnant women
admitted to hospital for delivery: experience of a pandemic
center in Turkey. Eur J Obstet Gynecol Reprod Biol
2020;253:31-4. Crossref
29. Herraiz I, Folgueira D, Villalaín C, Forcén L, Delgado R, Galindo A. Universal screening for SARS-CoV-2 before
labor admission during Covid-19 pandemic in Madrid. J
Perinat Med 2020;48:981-4. Crossref
30. The Royal College of Obstetricians and Gynaecologists.
Principles for the testing and triage of women seeking
maternity care in hospital settings, during the COVID-19
pandemic. A supplementary framework for maternity
healthcare professionals. version 2. Available from:
https://www.rcog.org.uk/globalassets/documents/guidelines/2020-08-10-principles-for-the-testing-and-triage-of-women-seeking-maternity-care-in-hospital-settings-during-the-covid-19-pandemic.pdf. Accessed 2
Oct 2020.