EDITORIAL
Kidney Health for All: bridging the gap in kidney health education and literacy
Robyn G Langham, MB, BS, PhD1 #; Kamyar Kalantar-Zadeh, MD, PhD2 #; Ann Bonner, RN, PhD3; Alessandro Balducci, MD4 #; LL Hsiao, MD, PhD5 #; Latha A Kumaraswami, BA6 #; Paul Laffin, MS7 #; Vassilios Liakopoulos, MD, PhD8 #; Gamal Saadi, MD9 #; Ekamol Tantisattamo, MD, MPH2;
Ifeoma Ulasi, MB, BS, MSc10 #; SF Lui, MD11 #; for the World Kidney Day Joint Steering Committee#
1 St Vincent’s Hospital, Department of Medicine, University of Melbourne, Melbourne, Victoria, Australia
2 Division of Nephrology, Hypertension and Kidney Transplantation, Department of Medicine, University of California Irvine School of Medicine, Orange, California, United States
3 School of Nursing and Midwifery, Griffith University, Southport, Queensland, Australia
4 Italian Kidney Foundation, Rome, Italy
5 Brigham and Women’s Hospital, Renal Division, Department of Medicine, Boston, Massachusetts, United States
6 Tamilnad Kidney Research (TANKER) Foundation, The International Federation of Kidney Foundations–World Kidney Alliance
(IFKF–WKA), Chennai, India
7 International Society of Nephrology, Brussels, Belgium
8 Division of Nephrology and Hypertension, First Department of Internal Medicine, AHEPA Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece
9 Nephrology Unit, Department of Internal Medicine, Faculty of Medicine, Cairo University, Giza, Egypt
10 Renal Unit, Department of Medicine, College of Medicine, University of Nigeria, Ituku-Ozalla, Enugu, Nigeria
11 International Federation of Kidney Foundations–World Kidney Alliance, The Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong
# Members of the World Kidney Day Steering Committee
 Full paper in PDF
Full paper in PDF
Abstract
The high burden of kidney disease, global disparities in kidney care, and poor outcomes of kidney failure bring a concomitant growing burden to persons affected, their families, and carers, and the community at large. Health literacy is the degree to which persons and organisations have or equitably enable individuals to have the ability to find, understand, and use information and services to make informed health-related decisions and actions for themselves and others. Rather than viewing health literacy as a patient deficit, improving health literacy largely rests with healthcare providers communicating and educating effectively in codesigned partnership with those with kidney disease. For kidney policy makers, health literacy provides the imperative to shift organisations to a culture that places the person at the centre of healthcare. The growing capability of and access to technology provides new opportunities to enhance education and awareness of kidney disease for all stakeholders. Advances in telecommunication, including social media platforms, can be leveraged to enhance persons’ and providers’ education; The World Kidney Day declares 2022 as the year of “Kidney Health for All” to promote global teamwork in advancing strategies in bridging the gap in kidney health education and literacy. Kidney organisations should work towards shifting the patient-deficit health literacy narrative to that of being the responsibility of healthcare providers and health policy makers. By engaging in and supporting kidney health–centred policy making, community health planning, and health literacy approaches for all, the kidney communities strive to prevent kidney diseases and enable living well with kidney disease.
Given the high burden of kidney disease and global disparities related to kidney care, in carrying forward our mission of advocating Kidney Health for All, the challenging issue of bridging the well-identified gap in the global understanding of kidney disease and its health literacy is the theme for World Kidney Day (WKD) 2022. Health literacy is defined as the degree to which persons and organisations have—or equitably enable individuals to have—the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.
1 Not only is there is growing recognition of the role that health literacy has in determining outcomes for persons affected by kidney disease and the community in general, but there is an emergent imperative for policy makers worldwide to be informed and cognizant of opportunities and real measurable outcomes that can be achieved through kidney-specific preventative strategies.
The global community of people
with kidney disease
Most people are not aware of what kidneys are for
or even where their kidneys are. For those afflicted
by disease and the subsequent effects on overall
health, effective healthcare provider communication
is required to support individuals to be able to
understand what to do, to make decisions, and to
take action. Health literacy involves more than
functional abilities of an individual; it is also the
cognitive and social skills needed to gain access
to, understand, and use information to manage
health conditions.
2 It is also contextual
3 in that
as health needs change, so too does the level of
understanding and ability to problem solve alter. Health literacy is, therefore, an interaction between
individuals, healthcare providers, and health policy
makers.
4 This is why the imperatives around health
literacy are now recognised as indicators for the
quality of local and national healthcare systems and
healthcare professionals within them.
5 For chronic
kidney disease (CKD), as the disease progresses
alongside other health changes and increasing
treatment complexities, it becomes more difficult for
individuals to manage.
6 Promoted in health policy
for around a decade involving care partnerships
between health-centred policy, community health
planning, and health literacy,
7 current approaches
need to be shifted forward (
Table 1).
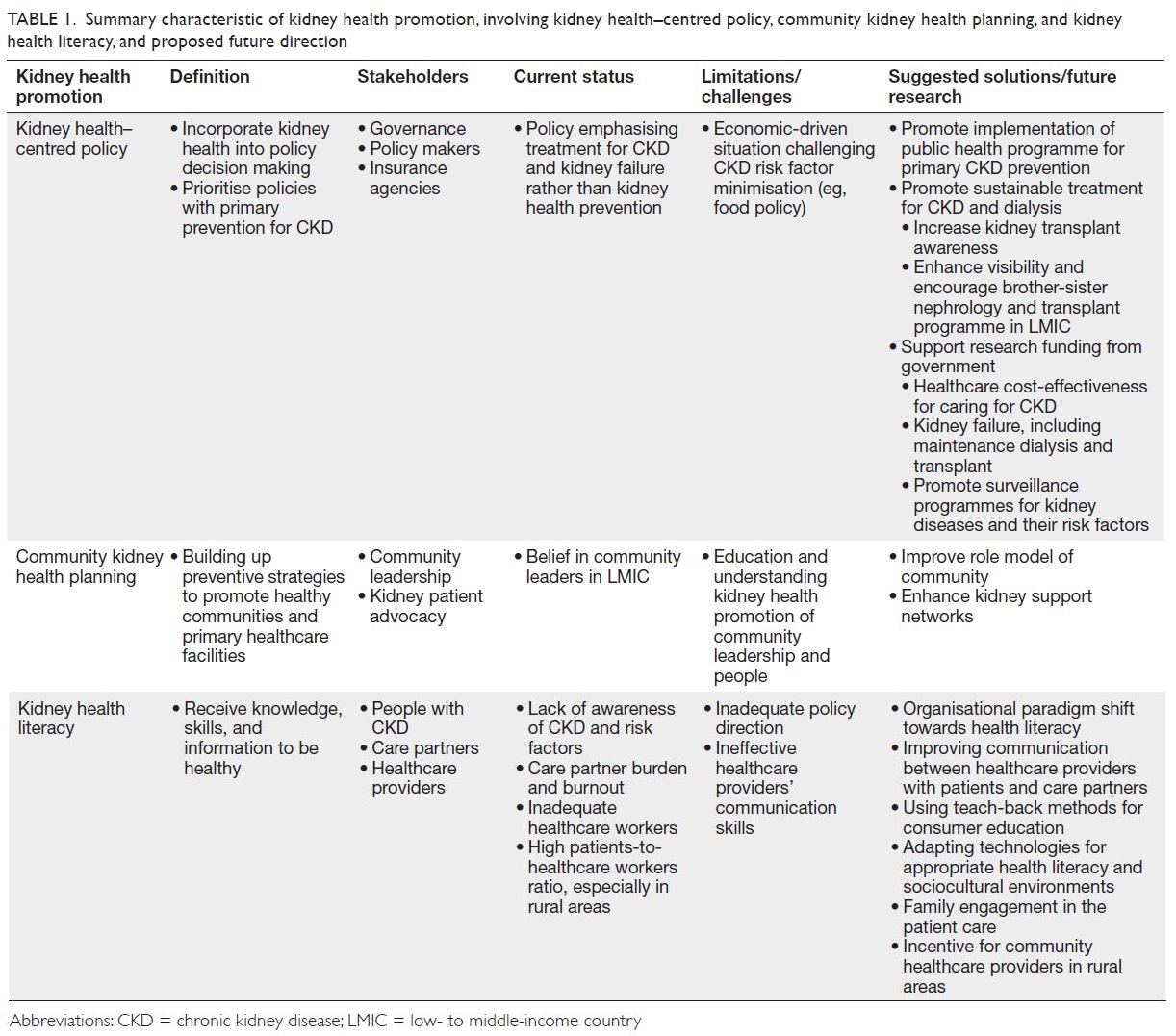
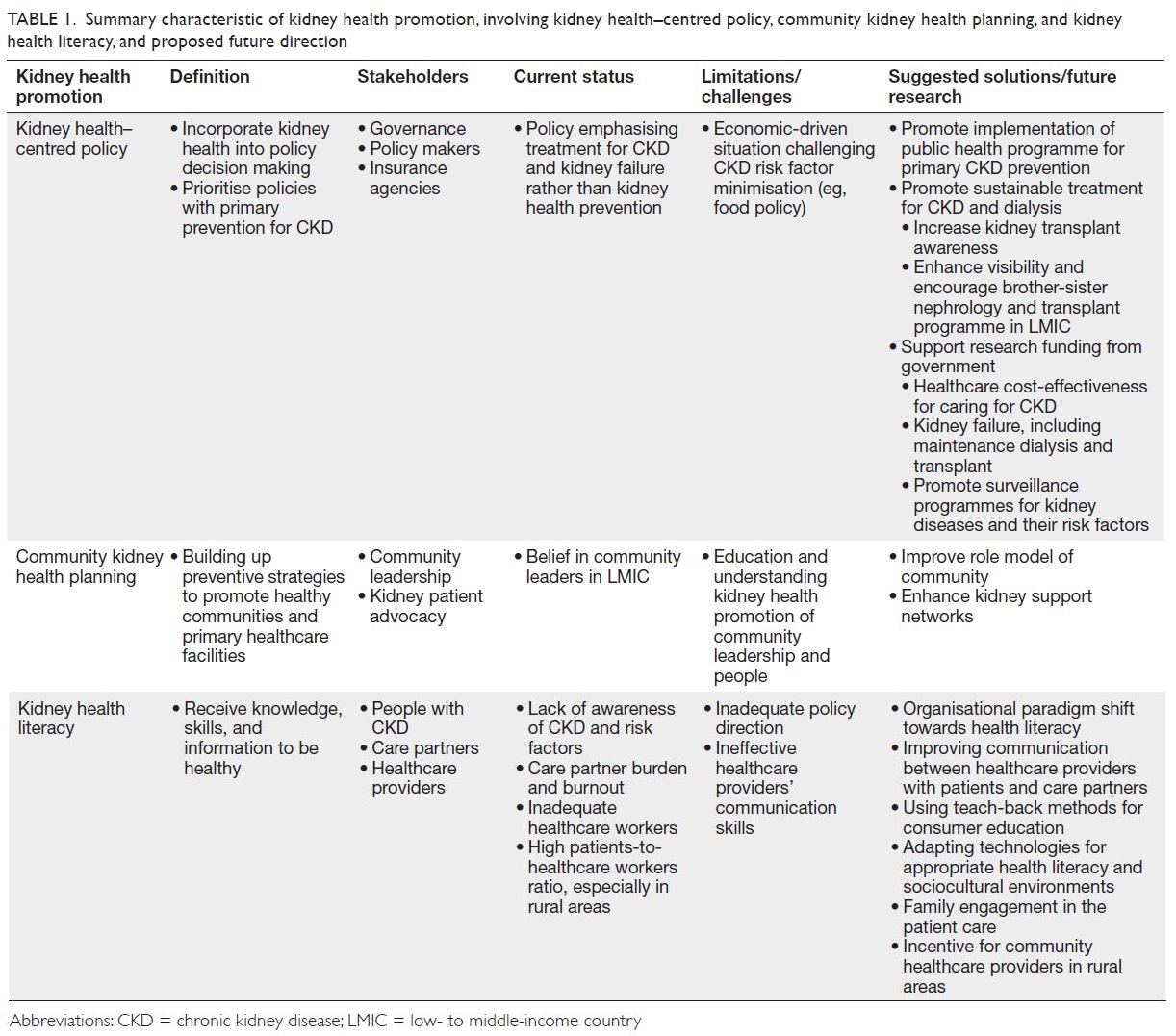 Table 1.
Table 1. Summary characteristic of kidney health promotion, involving kidney health–centred policy, community kidney health planning, and kidney
health literacy, and proposed future direction
Assessing health literacy necessitates the use
of appropriate multidimensional patient-reported measures, such as the World Health Organization–recommended Health Literacy Questionnaire
(available in over 30 languages) rather than tools
measuring only functional health literacy (eg, Rapid
Estimate of Adult Literacy in Medicine or Short
Test of Functional Health Literacy in Adults).
8 It is
therefore not surprising that studies of low health
literacy (LHL) abilities in people with CKD have
been demonstrated to be associated with poor
CKD knowledge, self-management behaviours,
and health-related quality of life and in those with
greater co-morbidity severity.
7 Unfortunately, most
CKD studies have measured only functional health
literacy, so the evidence that LHL results in poorer
outcomes, particularly that it increases healthcare
utilisation and mortality
9 and reduces access to
transplantation,
10 is weak.
Recently, health literacy is now considered to be
an important bridge between lower socioeconomic
status and other social determinants of health.
4
Indeed, this is not a feature that can be measured
by the gross domestic product of a country, as
the effects of LHL on the extent of CKD in the
community are experienced globally regardless of
country income status. The lack of awareness of
risk factors of kidney disease, even in those with
high health literacy abilities, is a testament to the
difficulties in understanding this disease, and why
the United States, for instance, recommends that
a universal precautions approach towards health
literacy is undertaken.
11
So, what does the perfect health literacy
programme look like for people with CKD? In
several high-income countries, there are national
health literacy action plans with the emphasis
shifted to policy directives, organisational culture,
and healthcare providers. In Australia, for instance,
a compulsory health literacy accreditation standard
makes the healthcare organisation responsible
for ensuring providers are cognizant of individual
health literacy abilities.
12 Although many high-income
countries, healthcare organisations, non-governmental
organisations, and jurisdictions are
providing an array of consumer-facing web-based
programmes that provide detailed information and
self-care training opportunities, most are largely
designed for individual/family use that are unlikely
to mitigate LHL. There is, however, substantial
evidence that interventions improving healthcare
provider communication are more likely to improve
understanding of health problems and abilities to
adhere to complex treatment regimens.
13
Access to information that is authentic and
tailored specifically to the needs of the individual and
the community is the aim. The challenge is recognised
acutely in more remote and low- to middle-income
countries of the world, specifically the importance
of culturally appropriate knowledge provision. The principles of improving health literacy are the same,
but understanding how to proceed, and putting
consumers in charge, with a co-design approach,
is critical and may result in a different outcome
in more remote parts of the world. This principle
especially applies to communities that are smaller,
with less access to electronic communication and
healthcare services, where the level of health literacy
is shared across the community and where what
affects the individual also affects all the community.
Decision support systems are different, led by elders,
and in turn educational resources are best aimed at
improving knowledge of the whole community.
A systematic review of the evaluation of
interventions and strategies shows this area of
research is still at an early stage,
14 with no studies
unravelling the link between LHL and poor CKD
outcomes. The best evidence is in supporting
targeted programmes on improving communication
capabilities of healthcare professionals as central.
One prime example is ‘teach-back’, a cyclical, simple,
low-cost education intervention, which shows
promise for improving communication, knowledge,
and self-management in the CKD populations in
low- or high-income countries.
15 Furthermore,
the consumer-led voice has articulated research
priorities that align closely with principles felt to be
important to the success of education: building new
education resources, devised in partnership with
consumers, and focussed on the needs of vulnerable
groups. Indeed, programmes that address the lack
of culturally safe, person-centred and holistic care,
along with improving the communication skills
of health professionals, are crucial for those with
CKD.
16
The networked community of
kidney healthcare workers
Nonphysician healthcare workers, including nurses
and advanced practice providers (physician assistants
and nurse practitioners) as well as dietitians,
pharmacists, social workers, technicians, physical
therapists, and other allied health professionals,
often spend more time with persons with kidney
disease, compared with nephrologists and other
physician specialists. In an ambulatory care setting at
an appointment, in the emergency department, or in
the in-patient setting, these healthcare professionals
often see and relate to the patient first, last, and
in between, given that physician encounters are
often short and focused. Hence, the nonphysician
healthcare workers have many opportunities to
discuss kidney disease-related topics with the
individuals and their care partners and to empower
them.
17 18 For instance, medical assistants can help
identify those with or at risk of developing CKD and
can initiate educating them and their family members about the role of diet and lifestyle modification for
primary, secondary, and tertiary prevention of CKD
while waiting to see the physician.
19 Some healthcare
workers provide networking and support for kidney
patient advocacy groups and kidney support
networks, which have been initiated or expanded via
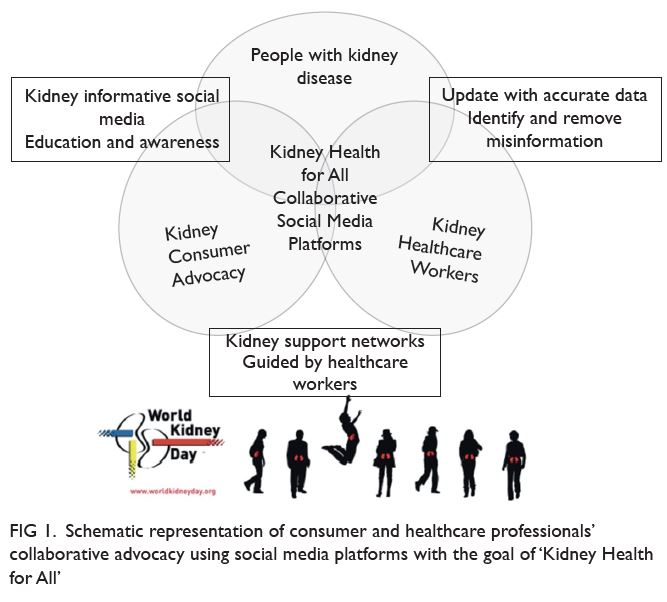
social media platforms (
Fig 1).
20 21 Studies examining the efficacy of social media in kidney care and
advocacy are on the way.
22 23
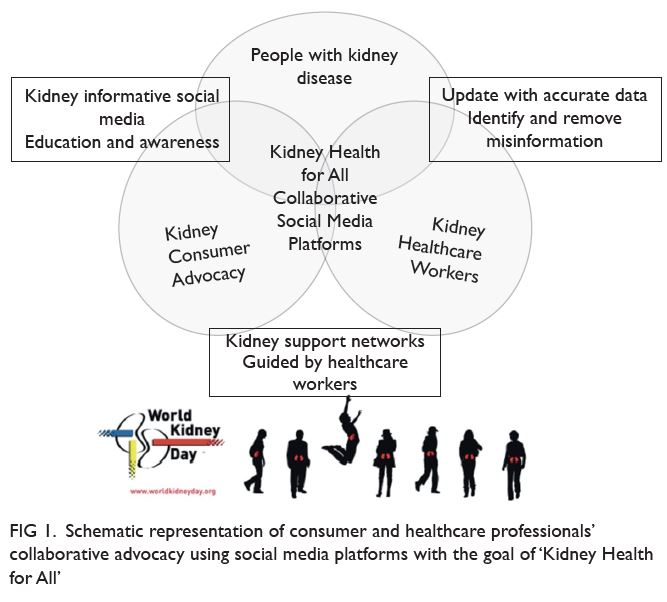 Figure 1.
Figure 1. Schematic representation of consumer and healthcare professionals’
collaborative advocacy using social media platforms with the goal of ‘Kidney Health for All’
Like physicians, many activities of nonphysician
healthcare workers have been increasingly
affected by the rise of electronic health recording
and growing access to internet-based resources,
including social media, that offer educational
materials related to kidney health, including kidney-preserving
therapies with traditional and emerging
interventions.
24 These resources can be used for both
self-education and for networking and advocacy on
kidney disease awareness and learning. Increasingly,
more healthcare professionals are engaged in some
types of social media-based activities, as shown
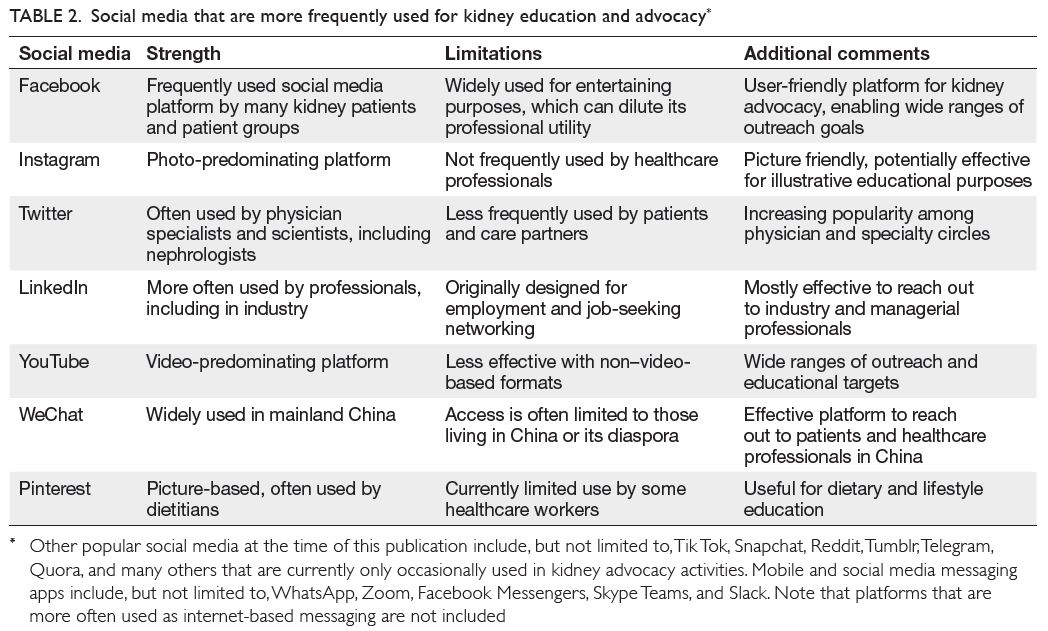
in
Table 2. At the time of this writing, the leading
social media used by many—but not all—kidney
healthcare workers include Facebook, Instagram,
Twitter, LinkedIn, and YouTube. In some regions of
the world, certain social media are more frequently
used than others given unique cultural or access
constellations (eg, WeChat is a platform often used
by healthcare workers and patient groups in China).
Some healthcare professionals, such as managers
and those in leadership and advocacy organisation
positions, may choose to embark on social media to
engage those with CKD and their care partners or
other healthcare professionals in alliance building
and marketing. To that end, effective communication
strategies and outreach skills specific to responsible
use of social media can provide clear advantages
given that these skills and strategies are different
and may need modification in those with LHL. It
is imperative to ensure the needed knowledge and training for an accountable approach to social media
is provided to healthcare providers, so that these
outreach strategies are utilised with the needed
awareness of their unique strengths and pitfalls, as
follows.
25
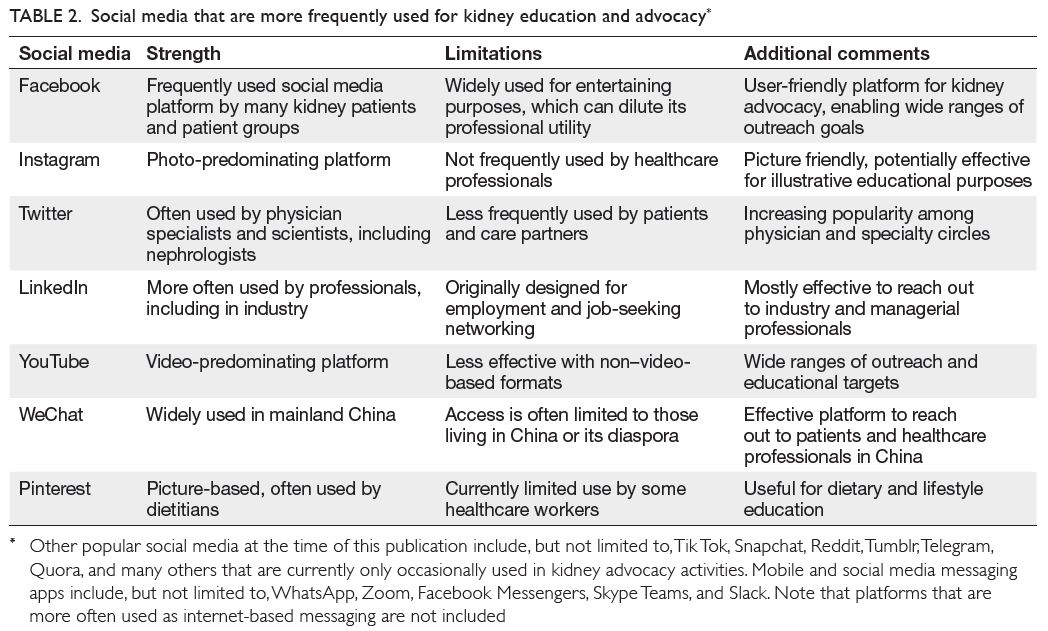 Table 2.
Table 2. Social media that are more frequently used for kidney education and advocacy
(i) Consumers’ and care partners’ confidentiality
may not be breached upon posting anything on
social media, including indirect referencing to
a specific individual or a particular description
of a condition unique to a specific person (eg,
upon soliciting for transplant kidney donors on
social media).
26 27
ii) Confidential information about clinics,
hospitals, dialysis centres, or similar healthcare
and advocacy entities may not be disclosed on
social media without ensuring that the needed
processes, including collecting authorisations
to disclose, are undertaken.
(iii) Healthcare workers’ job security and careers
should remain protected with thorough review
of the content of the messages and illustrations/videos before online posting.
(iv) Careless and disrespectful language and
emotional tones are often counterproductive
and may not be justified under the context of
freedom of speech.
The global kidney community of
policy and advocacy
Policy and advocacy are well-recognised tools
that, if properly deployed, can bring about change
and paradigm shift at the jurisdictional level. The
essence of advocating for policy change to better
address kidney disease is, in itself, an exercise in
improving health literacy of the policy makers.
Policy development, at its core, is a key stakeholder
or stakeholder group (eg, the kidney community,
which believes that a problem exists that should
be tackled through governmental action). There
is increasing recognition of the importance of
formulating succinct, meaningful, and authentic
information, akin to improving health literacy, to
present to governments for action.
Robust and efficacious policy is always
underpinned by succinct and applicable information;
however, the development and communication of
this message, designed to bridge the gap in knowledge
of relevant jurisdictions, is only part of the process of
policy development. An awareness of the process is
important to clinicians who are aiming to advocate
for effective change in prevention or improvement of
outcomes in the CKD community.
Public policies, the plans for future action
accepted by governments, are articulated through
a political process in response to stakeholder
observation, usually written as a directive, law,
regulation, procedure, or circular. Policies are purpose fit and targeted to defined goals and specific
societal problems and are usually a chain of actions
effected to solve those societal problems.
28 Policies
are an important output of political systems. Policy
development can be formal, passing through
rigorous lengthy processes before adoption (such
as regulations), or it can be less formal and quickly
adopted (such as circulars). As already mentioned,
the governmental action envisaged by the key
stakeholders as a solution to a problem is at its core.
The process enables stakeholders to air their views
and bring their concerns to the fore. Authentic
information that is meaningful to the government
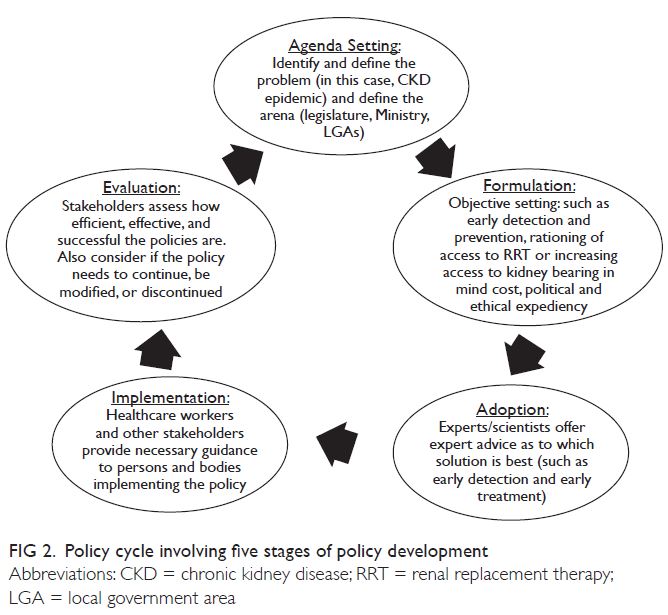
is critical. The policy development process can be
stratified into five stages (ie, the policy cycle), as
depicted by Anderson (1994)
29 and adapted and
modified by other authors
30 (
Fig 2). The policy cycle
constitutes an expedient framework for evaluating
the key components of the process.
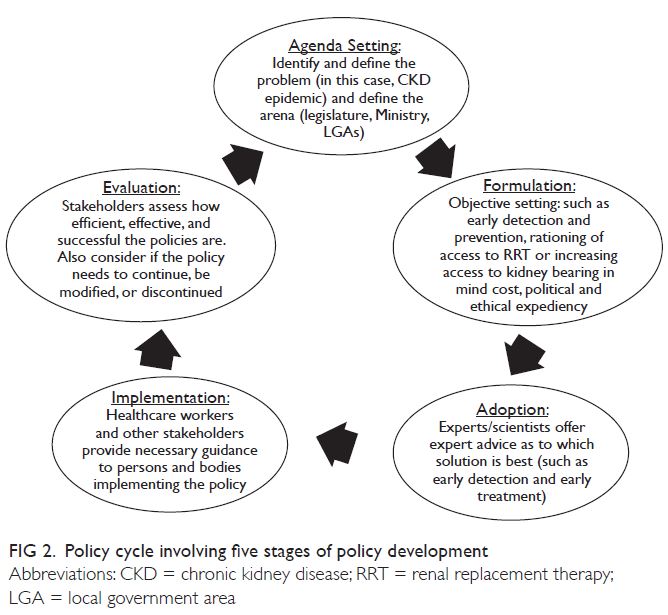 Figure 2.
Figure 2. Policy cycle involving five stages of policy development
Subsequently, the policy moves on to the
implementation phase. This phase may require
subsidiary policy development and adoption of
new regulations or budgets (implementation).
Policy evaluation is integral to the policy processes
and applies evaluation principles and methods to
assess the content, implementation, or impact of
a policy. Evaluation facilitates understanding and
appreciation of the worth and merit of a policy as well
as the need for its improvement. More important, of
the five principles of advocacy that underline policy
making,
31 the most important for clinicians engaged
in this space is that of commitment, persistence, and patience. Advocacy takes time to yield the desired
results.
The Advocacy Planning Framework,
developed by Young and Quinn in 2002, 30 consists
of overlapping circles representing three sets of
concepts (way into the process, the messenger, and
message and activities) that are key to planning any
advocacy campaign:
(i) “Way into the process”: discusses the best
approaches to translate ideas into the target
policy debate and identify the appropriate
audience to target.
(ii) Messenger: talks about the image maker
or face of the campaign and other support
paraphernalia that are needed.
(iii) Message and activities: describe what can
be said to the key target audiences that is
engaging and convincing. And how best it
can be communicated through appropriate
communication tools.
Advocacy is defined as “an effort or campaign
with a structured and sequenced plan of action
which starts, directs, or prevents a specific policy
change.”
31 The goal being to influence decision
makers through communicating directly with them
or getting their commitment through secondary
audiences (advisers, the media, or the public) to
the end that the decision maker understands, is
convinced, takes ownership of the ideas, and finally
has the compulsion to act.
31 As with improving
health literacy, it is the communication of ideas to
policy makers for adoption and implementation as
policy that is key. There is much to be done with
bridging this gap in understanding of the magnitude
of community burden that results from CKD.
Without good communication, many good ideas and
solutions do not reach communities and countries
where they are needed. Again, aligned with the
principles of developing resources for health literacy,
the approach also needs to be nuanced according to
the local need, aiming to have the many good ideas
and solutions be communicated to communities and
countries where they are needed
Advocacy requires galvanising momentum and
support for the proposed policy or recommendation.
The process is understandably slow as it involves
discussions and negotiations for paradigms, attitudes,
and positions to shift. In contemplating advocacy
activities, multiple factors must be considered,
interestingly not too dissimilar to that of building
health literacy resources: What obstructions are
disrupting the policy making process from making
progress? What resources are available to enable the
process to succeed? Is the policy objective achievable
considering all variables? Is the identified problem
already being considered by the policy makers
(government or multinational organisations)?
Any interest or momentum generated around it? Understandably, if there is some level of interest and
if governments already have a spotlight on the issue,
it is likely to succeed.
Approaches to choose from include the
following
31 32:
Advising (researchers are commissioned to
produce new evidence-based proposals to assist
the organisation in decision making).
Activism: involves petitions, public
demonstrations, posters, fliers, and leaflet
dissemination, often used by organisations to
promote a certain value set.
Media campaign: having public pressure on
decision makers helps in achieving results
Lobbying: entails face-to-face meetings with
decision makers; often used by business
organisations to achieve their purpose.
Here lies the importance of effective and
successful advocacy to stakeholders, including policy
makers, healthcare professionals, communities,
and key change makers in society. The WKD, since
inception, has aimed at playing this role. World
Kidney Day has gained people’s trust by delivering
relevant and accurate messaging and supporting
leaders in local engagement, and it is celebrated by
kidney care professionals, celebrities, those with
the disease, and their caregivers all over the world.
To achieve the goal, an implementation framework
of success in a sustainable way includes creativity,
collaboration, and communication.
The ongoing challenge for the International
Society of Nephrology and International Federation
of Kidney Foundations—World Kidney Alliance,
through the Joint Steering Committee of WKD,
is to operationalise how to collate key insights
from research and analysis to effectively feed the
policy making process at the local, national, and
international levels, to inform or guide decision
making (ie, increasing engagement of governments
and organisations, like World Health Organization,
United Nations, and regional organisations,
especially in low-resource settings). There is a clear
need for ongoing renewal of strategies to increase
efforts at closing the gap in kidney health literacy,
empowering those affected with kidney disease
and their families, giving them a voice to be heard,
and engaging with civil society. This year, the Joint
Steering Committee of WKD declares “Kidney
Health for All” as the theme of the 2022 WKD to
emphasise and extend collaborative efforts among
people with kidney disease, their care partners,
healthcare providers, and all involved stakeholders
for elevating education and awareness on kidney
health and saving lives with this disease.
Conclusions
In bridging the gap of knowledge to improve
outcomes for those with kidney disease on a global basis, an in-depth understanding of the needs of the
community is required. The same can be said for
policy development, understanding the processes in
place for engagement of governments worldwide, all
underpinned by the important principle of codesign
of resources and policy that meets the needs of the
community for which it is intended.
For WKD 2022, kidney organisations, including
the International Society of Nephrology and
International Federation of Kidney Foundations—World Kidney Alliance, have a responsibility to
immediately work towards shifting the patient-deficit
health literacy narrative to that of being the
responsibility of clinicians and health policy makers.
Low health literacy occurs in all countries regardless
of income status; hence, simple, low-cost strategies
are likely to be effective. Communication, universal
precautions, and teach-back can be implemented by
all members of the kidney healthcare team. Through
this vision, kidney organisations will lead the shift
to improved patient-centred care, support for care
partners, health outcomes, and the global societal
burden of kidney healthcare.
Author contributions
All authors contributed equally to the conception, preparation, and editing of the manuscript.
Conflicts of interest
K Kalantar-Zadeh reports honoraria from Abbott, Abbvie,
ACI Clinical, Akebia, Alexion, Amgen, Ardelyx, AstraZeneca,
Aveo, BBraun, Cara Therapeutics, Chugai, Cytokinetics,
Daiichi, DaVita, Fresenius, Genentech, Haymarket Media,
Hospira, Kabi, Keryx, Kissei, Novartis, Pfizer, Regulus,
Relypsa, Resverlogix, Dr Schaer, Sandoz, Sanofi, Shire,
Vifor, UpToDate, and ZS-Pharma. V Liakopoulos reports
nonfinancial support from Genesis Pharma. G Saadi
reports personal fees from Multicare, Novartis, Sandoz, and
AstraZeneca. E Tantisattamo reports nonfinancial support
from Natera. Other authors declared no competing interests.
Funding/support
This editorial received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Declaration
This article was published in
Kidney International (Langham
RG, Kalantar-Zadeh K, Bonner A, et al. Kidney health for
all: bridging the gap in kidney health education and literacy.
Kidney International. 2022;101(3):432-440.
https://doi.
org/10.1016/j.kint.2021.12.017), and reprinted concurrently
in several journals. The articles cover identical concepts and
wording, but vary in minor stylistic and spelling changes,
detail, and length of manuscript in keeping with each journal’s
style. Any of these versions may be used in citing this article.
References
1. Centers for Disease Control and Prevention. Healthy
people 2030: What is health literacy? Available from: https://www.cdc.gov/healthliteracy/learn/index.html.
Accessed 16 Jan 2022.
2. Nutbeam D. The evolving concept of health literacy. Soc
Sci Med 2008;67:2072-8.
Crossref3. Lloyd A, Bonner A, Dawson-Rose C. The health
information practices of people living with chronic health
conditions: implications for health literacy. J Librariansh
Inf Sci 2014;46:207-16.
Crossref4. Sørensen K, Van den Broucke S, Fullam J, et al. Health
literacy and public health: a systematic review and
integration of definitions and models. BMC Public Health
2012;12:80.
Crossref5. Nutbeam D, Lloyd JE. Understanding and responding to
health literacy as a social determinant of health. Annu Rev
Public Health 2021;42:159-73.
Crossref6. Shah JM, Ramsbotham J, Seib C, Muir R, Bonner A. A
scoping review of the role of health literacy in chronic
kidney disease self-management. J Ren Care 2021;47:221-33.
Crossref7. Dinh HT, Nguyen NT, Bonner A. Healthcare systems
and professionals are key to improving health literacy in
chronic kidney disease. J Ren Care 2022;48:4-13.
Crossref8. Dodson S, Good S, Osborne R. Health Literacy Toolkit for
Low- and Middle-income Countries: a Series of Information
Sheets to Empower Communities and Strengthen Health
Systems. New Delhi: World Health Organization; 2015.
9. Taylor DM, Fraser S, Dudley C, et al. Health literacy and
patient outcomes in chronic kidney disease: a systematic
review. Nephrol Dial Transplant 2018;33:1545-58.
Crossref10. Taylor DM, Bradley JA, Bradley C, et al. Limited health
literacy is associated with reduced access to kidney
transplantation. Kidney Int 2019;95:1244-52.
Crossref11. Brega AG, Barnard J, Mabachi NM, et al. AHRQ Health
Literacy Universal Precautions Toolkit, Second Edition.
(Prepared by Colorado Health Outcomes Program,
University of Colorado Anschutz Medical Campus under
Contract No. HHSA290200710008, TO#10.) AHRQ
Publication No. 15-0023-EF. Rockville, MD: Agency for
Healthcare Research and Quality; Jan 2015.
12. Australian Commission on Safety and Quality in Health
Care. Health literacy: taking action to improve safety and
quality. Sydney: ACSQHC, 2014. Available from: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/health-literacy-taking-action-improve-safety-and-quality. Accessed 17 Jan 2022.
13. Visscher BB, Steunenberg B, Heijmans M, et al. Evidence
on the effectiveness of health literacy interventions in the
EU: a systematic review. BMC Public Health 2018;18:1414.
Crossref14. Boonstra MD, Reijneveld SA, Foitzik EM, Westerhuis R,
Navis G, de Winter AF. How to tackle health literacy
problems in chronic kidney disease patients? A systematic
review to identify promising intervention targets and
strategies. Nephrol Dial Transplant 2020;36:1207-21.
Crossref15. Nguyen NT, Douglas C, Bonner A. Effectiveness of selfmanagement
programme in people with chronic kidney
disease: a pragmatic randomized controlled trial. J Adv
Nurs 2019;75:652-64.
Crossref16. Synnot A, Bragge P, Lowe D, et al. Research priorities in
health communication and participation: international
survey of consumers and other stakeholders. BMJ Open
2018;8:e019481.
Crossref17. Kalantar-Zadeh K, Li PK, Tantisattamo E, et al. Living
well with kidney disease by patient and care-partner empowerment: kidney health for everyone everywhere.
Kidney Int 2021;99:278-84.
Crossref18. Jager KJ, Kovesdy C, Langham R, Rosenberg M,
Jha V, Zoccali C. A single number for advocacy and
communication-worldwide more than 850 million
individuals have kidney diseases. Kidney Int 2019;96:1048-50.
Crossref19. Li PK, Garcia-Garcia G, Lui SF, et al. Kidney health for
everyone everywhere—from prevention to detection and
equitable access to care. Kidney Int 2020;97:226-32.
Crossref20. Gilford S. Patients helping patients: the Renal Support
Network. Nephrol Nurs J 2007;34:76.
21. Muhammad S, Allan M, Ali F, Bonacina M, Adams M.
The renal patient support group: supporting patients with
chronic kidney disease through social media. J Ren Care
2014;40:216-8.
Crossref22. Li WY, Chiu FC, Zeng JK, et al. Mobile health app with
social media to support self-management for patients with
chronic kidney disease: prospective randomized controlled
study. J Med Internet Res 2020;22:e19452.
Crossref23. Pase C, Mathias AD, Garcia CD, Garcia Rodrigues C.
Using social media for the promotion of education and
consultation in adolescents who have undergone kidney
transplant: protocol for a randomized control trial. JMIR
Res Protoc 2018;7:e3.
Crossref24. Kalantar-Zadeh K, Jafar T, Nitsch D, Neuen BL, Perkovic V.
Chronic kidney disease. Lancet 2021;398:786-802.
Crossref25. Chen L, Sivaparthipan CB, Rajendiran S. Unprofessional
problems and potential healthcare risks in individuals’
social media use. Work 2021;68:945-53.
Crossref26. Henderson ML, Herbst L, Love AD. Social media and
kidney transplant donation in the United States: clinical
and ethical considerations when seeking a living donor.
Am J Kidney Dis 2020;76:583-5.
Crossref27. Henderson ML. Social media in the identification of living
kidney donors: platforms, tools, and strategies. Curr
Transplant Rep 2018;5:19-26.
Crossref28. Newton K, van Deth JW, editors. Foundations of
Comparative Politics Democracies of the Modern World.
2nd ed. Cambridge, UK: Cambridge University Press; 2010.
Crossref29. Anderson JE. Public Policymaking: An Introduction. 2nd ed. Boston, MA: Houghton Mifflin; 1994.
30. Young E, Quinn L, eds. Writing effective public policy
papers: a guide to policy advisers in Central and Eastern
Europe. Budapest, Hungary: Open Society Institute. 2002.
Available from: https://www.icpolicyadvocacy.org/sites/icpa/files/downloads/writing_effective_public_policy_papers_young_quinn.pdf. Accessed 13 Dec 2021.
31. Young E, Quinn L, eds. Making research evidence matter: a
guide to policy advocacy in transition countries. Budapest,
Hungary: Open Society Foundations. 2012. Available from:
https://advocacyguide.icpolicyadvocacy.org/sites/icpa-book.local/files/Policy_Advocacy_Guidebook_2012.pdf.
Accessed 13 Dec 2021.
32. Start D, Hovland I. Tools for policy impact: a handbook
for researchers, research and policy in development
programme. London, UK: Overseas Development
Institute. 2004. Available from: https://www.ndi.org/sites/default/files/Tools-for-Policy-Impact-ENG.pdf. Accessed 13 Dec 2021.