Faculty development for postgraduate medical education in Hong Kong
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
Faculty development for postgraduate medical
education in Hong Kong
HY So, FHKAM (Anaesthesiology)1; Philip KT Li, FHKAM (Medicine)2; Benny CP Cheng, FHKAM (Anaesthesiology)3; Faculty Development Workgroup, Hong Kong Jockey Club Innovative Learning Centre for Medicine#; Gilberto KK Leung, FHKAM (Surgery)4
1 Educationist, Hong Kong Academy of Medicine, Hong Kong SAR, China
2 Vice-President (Education and Examinations), Hong Kong Academy of Medicine, Hong Kong SAR, China
3 Honorary Director, Hong Kong Jockey Club Innovative Learning Centre for Medicine, Hong Kong SAR, China
4 President, Hong Kong Academy of Medicine, Hong Kong SAR, China
# Members of Faculty Development Workgroup:
Albert KM Chan (The Hong Kong College of Anaesthesiologists),
Dominic KL Ho (The College of Dental Surgeons of Hong Kong),
Franklin TT She (The College of Dental Surgeons of Hong Kong),
YF Choi (Hong Kong College of Emergency Medicine),
Peter Anthony Fok (The Hong Kong College of Family Physicians),
KK Tang (The Hong Kong College of Obstetricians and Gynaecologists),
Jason CS Yam (The College of Ophthalmologists of Hong Kong),
PT Chan (The Hong Kong College of Orthopaedic Surgeons),
KC Wong (The Hong Kong College of Otorhinolaryngologists),
SP Wu (Hong Kong College of Paediatricians),
Rock YY Leung (The Hong Kong College of Pathologists),
YM Kan (Hong Kong College of Physicians),
CW Law (The Hong Kong College of Psychiatrists),
Kevin KF Fung (Hong Kong College of Radiologists),
Skyi YC Pang (The College of Surgeons of Hong Kong)
Albert KM Chan (The Hong Kong College of Anaesthesiologists),
Dominic KL Ho (The College of Dental Surgeons of Hong Kong),
Franklin TT She (The College of Dental Surgeons of Hong Kong),
YF Choi (Hong Kong College of Emergency Medicine),
Peter Anthony Fok (The Hong Kong College of Family Physicians),
KK Tang (The Hong Kong College of Obstetricians and Gynaecologists),
Jason CS Yam (The College of Ophthalmologists of Hong Kong),
PT Chan (The Hong Kong College of Orthopaedic Surgeons),
KC Wong (The Hong Kong College of Otorhinolaryngologists),
SP Wu (Hong Kong College of Paediatricians),
Rock YY Leung (The Hong Kong College of Pathologists),
YM Kan (Hong Kong College of Physicians),
CW Law (The Hong Kong College of Psychiatrists),
Kevin KF Fung (Hong Kong College of Radiologists),
Skyi YC Pang (The College of Surgeons of Hong Kong)
Corresponding author: Dr HY So (sohingyu59@gmail.com)
Competency-based medical education and faculty development
By the late 20th century, traditional teaching methods
in postgraduate medical education were considered
inadequate for preparing doctors to navigate modern
healthcare systems, thereby posing risks to patient
safety. This realisation led to a global shift towards
competency-based medical education.1 2 3 The Hong
Kong Academy of Medicine (HKAM) identifies
seven key competencies essential for contemporary
medical practitioners, namely, professional
expertise, interpersonal communication, teamwork,
leadership, professionalism, academia, and health
promotion. The achievement of proficiency in these
areas requires novel approaches to teaching and
learning.
Traditional postgraduate medical education
is often centred around two main principles: the
transmission of knowledge and the ‘see one, do one,
teach one’ model. Although knowledge acquisition
is essential, mere memorisation of facts and
information does not lead to excellence in medical
practice. Effective education requires more than the
delivery of information. It involves selecting content
aligned with learning objectives, organising and
presenting material in ways that reflect how people
learn, and fostering motivation to engage with the
material.4 It had been demonstrated that knowledge
acquisition alone does not result in expertise.5
Individuals may successfully recall information
and perform well on examinations, but they often
encounter difficulties when addressing real-life clinical problems. The application of knowledge is
critical, and hands-on clinical experience is invaluable.
However, the tasks encountered in postgraduate
medicine are more complex and challenging than
those in traditional apprenticeships, rendering the
‘see one, do one, teach one’ method insufficient.
Teaching methods that provide support and promote
a deeper understanding of material are necessary to
develop true expertise in medicine.6 The importance
of such teaching methods underscores the critical
need for faculty development—commonly referred
to as training for trainers—which involves acquiring
new skills and knowledge while undergoing a shift in
mindset.
The Faculty Development Workgroup
Faculty development is central to the successful
implementation of competency-based medical
education. It includes activities undertaken by
healthcare professionals to enhance teaching,
leadership, research, and scholarly abilities in both
individual and group contexts.7 This emphasis on
faculty development was highlighted in the Position
Paper on Postgraduate Medical Education, published
in 2023.8 The Hong Kong Jockey Club Innovative
Learning Centre for Medicine (ILCM), established
by HKAM, was created to modernise postgraduate
medical education in Hong Kong. Initially focused
on simulation-based medical education, the ILCM
has since broadened its scope to address all aspects of postgraduate medical education.9 Recognising the
importance of faculty development, the ILCM has
assumed a leading role in advocating for this concept
within the medical community. To advance these
efforts, the ILCM formed the Faculty Development
Workgroup (the ‘Workgroup’), which includes
representatives from all 15 Colleges under HKAM,
to collaborate on faculty development initiatives.
To ensure that faculty development in
postgraduate medical education is competency-based,
the Workgroup conducted a literature review
to identify existing frameworks and identified seven
relevant models.10 11 12 13 14 15 16 After careful deliberation, the
frameworks proposed by Hesketh et al12 and the
Academy of Medical Educators16 were deemed the
most comprehensive and appropriate for adaptation
to the local context in Hong Kong.
The Faculty Development Framework of the Academy
Steinert7 defines faculty as all individuals involved
in teaching and educating learners across the
educational continuum (eg, undergraduate,
graduate, postgraduate, and continuing professional
development), leadership and management within
universities, hospitals, and the community, as well
as research and scholarship in the health professions
(eg, communication sciences, dentistry, nursing, and
rehabilitation sciences). Based on this definition, the
Workgroup delineated four categories of faculty
within the framework: trainers, examiners, supervisors
of training, and collegial leads in medical education
within each College of HKAM. The initial phase of
development focused on creating the Framework
for Faculty Development of Trainers, which outlines the key competencies required for trainers. This
framework facilitates the identification of individual
learning needs, supports effective delivery of course
content, and guides the evaluation of outcomes of the
faculty development programme.17
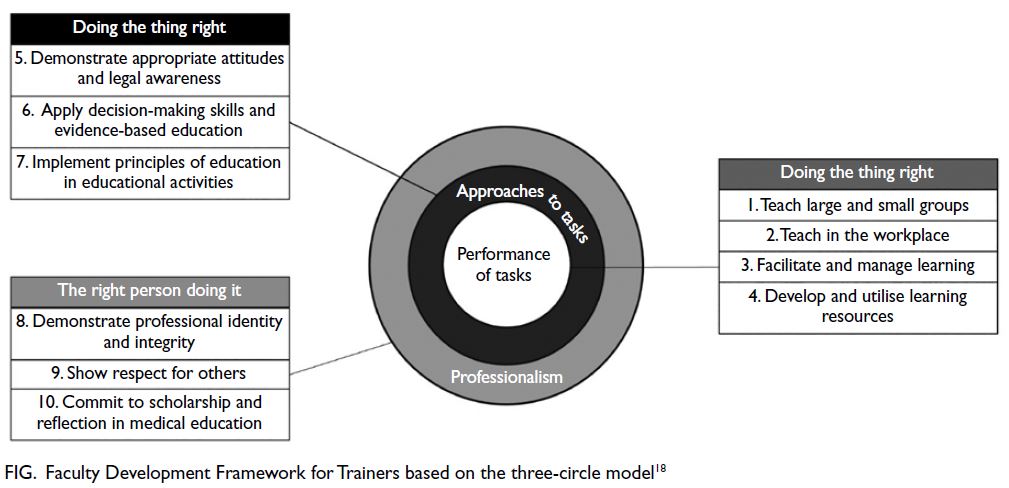
The Workgroup adopted the three-circle model
to classify learning outcomes proposed by Simpson
et al.18 This model categorises competencies into core
tasks, approaches to tasks, and professional identity,
ensuring that trainers perform their roles effectively
while approaching these roles with appropriate
attitudes and professionalism (Fig).18
Workshops and beyond for faculty development
The Framework for Faculty Development of Trainers17
was approved earlier this year by the Education
Committee and the Council of HKAM (Fig). In the
future, the ILCM will design and implement training
workshops guided by the following principles19:
Evidence-informed educational design
Relevant content
Experiential learning with opportunities for practice and application
Opportunities for feedback and reflection
Intentional community building
Moreover, a recent systematic review has
highlighted key principles for effective faculty
development that extend beyond workshops and
individual teaching effectiveness. These principles
include strengthening participants’ identities as
educators, promoting recognition of educational
excellence and leadership development, and fostering
communities of practice to support ongoing learning
and skill refinement.20 This comprehensive approach
reflects the learning process for clinical skills, which requires practice, feedback, and continuous
development in the workplace. Therefore, effective
faculty development will require sustained support
from HKAM and collaboration with stakeholders
across all Colleges to ensure that faculty continue to
advance their skills after completing workshops.
Conclusion
Faculty development is essential for the advancement
of postgraduate medical education in Hong
Kong. By equipping trainers with the appropriate
competencies and skills, the framework ensures that
doctors in training receive high-quality education
and mentorship, ultimately enhancing patient care
and outcomes within the healthcare system.6
Author contributions
All authors have contributed equally to the concept,
development and critical revision of the manuscript. All
authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have declared no conflicts of interest.
Funding/support
This editorial received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Kohn LT, Corrigan JM, Donaldson MS, editors. To Err Is
Human: Building a Safer Health System. Washington (DC):
National Academies Press; 2000.
2. Institute of Medicine (US) Committee on Quality of Health
Care in America. Crossing the quality chasm: a new health
system for the 21st century. Washington (DC): National
Academies Press (US); 2001.
3. Whitehead CR, Austin Z, Hodges BD. Flower power: the
armoured expert in the CanMEDS competency framework?
Adv Health Sci Educ Theory Pract 2011;16:681-94. Crossref
4. Swanwick T, Forrest K, O’Brien BC, editors. Understanding
Medical Education: Evidence, Theory, and Practice. The
Association for the Study of Medical Education (ASME);
2019. Crossref
5. Dreyfus SE, Dreyfus HL. A five-stage model of the mental
activities involved in direct skill acquisition. Operations
Research Center, University of California, Berkeley; 1980.
6. So HY. Postgraduate medical education: see one, do one,
teach one…and what else? Hong Kong Med J 2023;29:104. Crossref
7. Steinert Y. Faculty development: core concepts and principles. In: Steinert Y, editor. Faculty Development in
the Health Professions: A Focus on Research and Practice.
Innovation and Change in Professional Education, 11.
Dordrecht [NY]: Springer; 2014: 3-25. Crossref
8. So HY, Li PK, Lai PB, et al. Hong Kong Academy of Medicine
position paper on postgraduate medical education 2023.
Hong Kong Med J 2023;29:448-52. Crossref
9. Chen PP, So HY, Lo JS, Cheng BC. Modernising
postgraduate medical education: evolving roles of the
Hong Kong Jockey Club Innovative Learning Centre for
Medicine in the Hong Kong Academy of Medicine. Hong
Kong Med J 2023;29:480-3. Crossref
10. Skeff KM, Stratos GA, Bergen MR, Regula DP Jr. A pilot
study of faculty development for basic science teachers.
Acad Med 1998;73:701-4. Crossref
11. Harden RM, Crosby J. AMEE Guide No. 20: The good teacher is more than a lecturer—the twelve roles of the teacher. Med Teach 2000;22:334-47. Crossref
12. Hesketh EA, Bagnall G, Buckley EG, et al. A framework
for developing excellence as a clinical educator. Med Educ
2001;35:555-64. Crossref
13. Molenaar WM, Zanting A, van Beukelen P, et al. A
framework of teaching competencies across the medical
education continuum. Med Teach 2009;31:390-6. Crossref
14. Milner RJ, Gusic ME, Thorndyke LE. Perspective:
toward a competency framework for faculty. Acad Med
2011;86:1204-10. Crossref
15. Srinivasan M, Li ST, Meyers FJ, et al. “Teaching as a
Competency”: competencies for medical educators. Acad
Med 2011;86:1211-20. Crossref
16. Academy of Medical Educators. Professional standards for
medical, dental and veterinary educators (fourth edition).
2022. Available from: https://www.medicaleducators.org/write/MediaManager/Documents/AoME_Professional_Standards_4th_edition_1.0_(web_full_single_page_spreads).pdf . Accessed 1 Nov 2024.
17. Hong Kong Academy of Medicine. Framework for
Faculty Development Part 1: Trainers. September 2024.
Available from: https://www.hkam.org.hk/sites/default/files/PDFs/2024/HKAM_Faculty%20Development%20Framework_Part%201.pdf?v=1729586789500. Accessed 20 Sep 2024.
18. Simpson JG, Furnace J, Crosby J, et al. The Scottish
doctor—learning outcomes for the medical undergraduate
in Scotland: a foundation for competent and reflective
practitioners. Med Teach 2002;24:136-43. Crossref
19. Steinert Y, Mann K, Centeno A, et al. A systematic review
of faculty development initiatives designed to improve
teaching effectiveness in medical education: BEME Guide
No. 8. Med Teach 2006;28:497-526. Crossref
20. Steinert Y, Mann K, Anderson B, et al. A systematic review
of faculty development initiatives designed to enhance
teaching effectiveness: a 10-year update: BEME Guide No.
40. Med Teach 2016;38:769-86. Crossref