DOI: 10.12809/hkmj133750
PICTORIAL MEDICINE
Transient myeloproliferative disorder and non-immune hydrops fetalis in a neonate with trisomy 21
KL Hon, MD, FCCM1; TY Leung, FHKCOG, FHKAM (Obstetrics and Gynaecology)2
1 Department of Paediatrics, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin,
Hong Kong
2 Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin,
Hong Kong
A 39-year-old Rhesus-positive mother had been well.
She had been screened low risk (1:2496) for Down
syndrome (DS) at the first-trimester combined
screening in late 2012. The fetal morphology scan
at 20 weeks of gestation was normal. Nevertheless,
an ultrasound scan at 32 weeks of gestation showed
bilateral pleural effusions. Amnioreduction and left
pleural tap yielded 35 mL of pleural chyle. There was
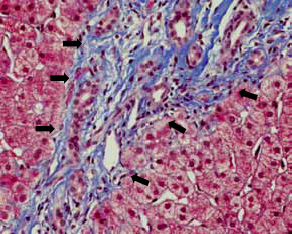
no evidence of a viral infection. A girl was delivered at 33-weeks-6-days of gestation by emergency
caesarean section because of recurrent fetal pleural
effusions. The neonate was mildly oedematous with
a distended abdomen and hepatomegaly
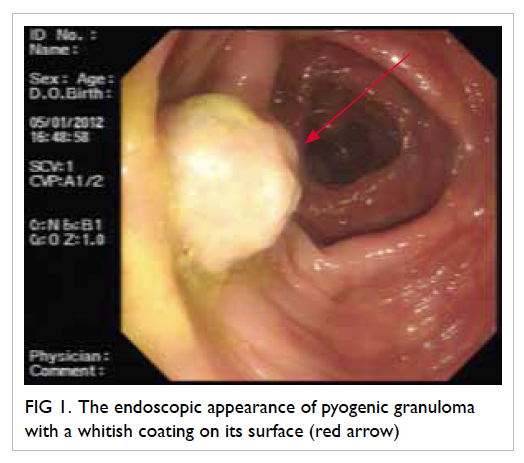
(Fig 1). The
baby was intubated and transferred to the neonatal
intensive care unit (ICU) for further management.
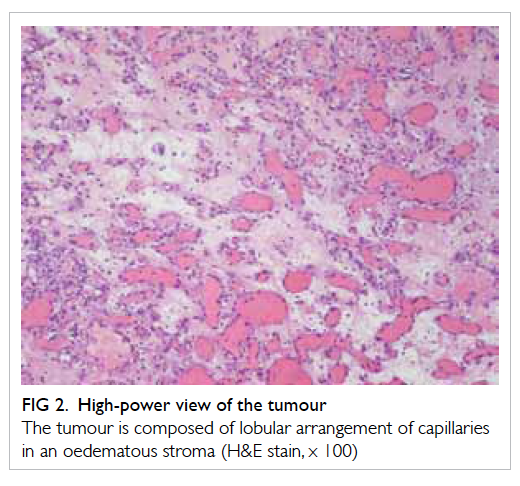
Pleural effusions
(Fig 2) were drained by pleural
tapping and chest drains. Echocardiography showed
that her cardiac structure and function appeared
normal, but a high pulmonary pressure and a
patent ductus arteriosus were evident. Plasma total
protein was 35 g/L (reference range, 65-82 g/L) and
albumin 22 g/L (reference range, 35-52 g/L). The
highest blood white cell count was 84.2 x 109 /L (50%
blasts). What is the underlying diagnosis for this
infant’s chylothoraces, hypoproteinaemia, and
leukocytosis?
1. Immune hydrops
2. Trisomy syndrome
3. Congenital infection
4. Congenital lymphoma
5. Inborn error of protein metabolism
 Figure 1.
Figure 1. Neonate immediately intubated following delivery
 Figure 2.
Figure 2. Bilateral pleural effusions
In the neonatal ICU, she improved with
full intensive support (mechanical ventilation,
thoracostomy drainage of pleural fluids, and
treatment with intravenous octreotide). Trisomy 21
(47,XY,+21) was subsequently confirmed following
chromosomal evaluation.
Hydrops fetalis (fetal hydrops) is a serious fetal
condition defined as an abnormal accumulation of
fluid in two or more fetal compartments, and includes
ascites, pleural effusion, pericardial effusion, and
skin oedema.
1 It may be due to immune or nonimmune
aetiologies.
1 2 Rhesus isoimmunisation
is the commonest immune aetiology, and alpha-thalassaemia
is a non-immune cause.
1
Immediate diagnosis of other aetiologies is often not
possible without extensive investigations. A prompt
spot diagnosis of DS was made in this neonate with
typical facial features, which obviated the need for
an extensive search for an underlying aetiology and
enabled target therapies to be instituted
(Fig 1).
Trisomy 21 is a known association with hydrops
fetalis and myeloproliferative disorder.
1 2
Transient myeloproliferative disorder
(TMD) is a self-limiting disorder characterised by
leukocytosis and the presence of megakaryoblasts
in the peripheral blood and bone marrow, anaemia,
thrombocytopenia, and organomegaly. It occurs in approximately 10% of newborn infants with DS.
2
Hepatic fibrosis is encountered in the severe form
of TMD with DS, and is characterised by diffuse
intralobular sinusoidal fibrosis and extramedullary
haematopoiesis.
3 Although TMD in most patients
resolves spontaneously within the first 3 months of
life, in a few severe cases there can be hepatic fibrosis
or cardiopulmonary failure. Acute megakaryocytic
leukaemia (AML-M7) is noted in 20 to 30% of
babies with DS and TMD within the first 4 years
of life.
4 Cytokines produced by megakaryocytes
(including transforming growth factor-beta,
platelet-derived growth factor, and platelet factor 4)
could be responsible for the pathogenesis of TMD.
3
The imbalance between intravascular or capillary
hydrostatic pressure and transcapillary filtration
may be responsible from hydrops fetalis.
2 3 4 5
Prompt recognition of the facial features of DS
is important to facilitate immediate diagnosis and
management of this neonate with hydrops fetalis.
References
1. Bellini C, Hennekam RC, Fulcheri E, et al. Etiology of nonimmune hydrops fetalis: a systematic review. Am J Med Genet A 2009;149A:844-51.
Crossref2. Oetama BK, Tucay RF, Morgan DL. Pathologic quiz case: nonimmune hydrops in a newborn. Down syndrome with acute (transient) leukemia. Arch Patho Lab Med 2001;125:1609-10.
3. Hongeng S, Pakakasama S, Hathirat P, Phuapradid P, Worapongpaiboon S. Diffuse hepatic fibrosis with transient myeloproliferative disorders in Down syndrome. J Pediatr Hematol Oncol 2000;22:543-4.
Crossref4. Al-Kasim F, Doyle JJ, Massey GV, Weinstein HJ, Zipursky A, Pediatric Oncology Group. Incidence and treatment of potentially lethal diseases in transient leukemia of Down syndrome: Pediatric Oncology Group Study. J Pediatr Hematol Oncol 2002;24:9-13.
Crossref5. De Groot CJ, Oepkes D, Egberts J, Kanhai HH. Evidence of endothelium involvement in the pathophysiology of hydrops fetalis? Early Hum Dev 2000;57:205-9.
Crossref