Hong
Kong Med J 2019 Jun;25(3):183–91 | Epub 29 May 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Questionnaire survey on medical futility and
termination of resuscitation in cardiac arrest patients among emergency
physicians in Hong Kong
CW So, MB, ChB1; CT Lui, FHKCEM, FHKAM
(Emergency Medicine)1; KL Tsui, FHKCEM, FHKAM (Emergency
Medicine)2; KL Chan, FHKCEM, FHKAM (Emergency Medicine)3;
Alex KK Law, FHKCEM, FHKAM (Emergency Medicine)4; YK Wong,
FHKCEM, FHKAM (Emergency Medicine)5; T Li, MB, ChB6;
CL Wong, FHKCEM, FHKAM (Emergency Medicine)7; SC Leung, FHKCEM,
FHKAM (Emergency Medicine)8
1 Department of Accident and Emergency,
Tuen Mun Hospital, Tuen Mun, Hong Kong
2 Department of Accident and Emergency,
Pok Oi Hospital, Yuen Long, Hong Kong
3 Department of Accident and Emergency,
Queen Elizabeth Hospital, Jordan, Hong Kong
4 Department of Accident and Emergency,
Prince of Wales Hospital, Shatin, Hong Kong
5 Department of Accident and Emergency,
Kwong Wah Hospital, Yaumatei, Hong Kong
6 Department of Accident and Emergency,
Tseung Kwan O Hospital, Tseung Kwan O, Hong Kong
7 Department of Accident and Emergency,
Princess Margaret Hospital, Laichikok, Hong Kong
8 Accident and Emergency Department,
Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr CT Lui (luict@ha.org.hk)
Abstract
Introduction: The perceptions of
medical futility and decisions about termination of resuscitation (TOR)
for out-of-hospital cardiac arrest (OHCA) are highly heterogeneous and
dependent on the practice of the attending emergency physicians. The
objective of this study was to report and investigate the knowledge,
attitudes, and practices regarding medical futility and TOR during
management of OHCA in Hong Kong.
Methods: A cross-sectional
survey was conducted among emergency medicine physicians in Hong Kong.
The questionnaire assessed participants’ background, knowledge,
attitudes, and behaviours concerning medical futility and TOR in
management of OHCA. Composite scores were calculated to reflect
knowledge, attitudes, and practices of OHCA treatment. Subgroup analysis
and multiple regression analysis were used to explore the relationship
between participants’ background, knowledge, attitudes, and behaviours.
Results: The response rate to
this survey was 57% (140/247). Independent predictors of less aggressive
resuscitation in OHCA patients included status as a Fellow of the Hong
Kong College of Emergency Medicine (β= -0.314, P=0.028) and being an
Advanced Cardiac Life Support instructor (β= -0.217, P=0.032). There was no
difference in aggressiveness of resuscitation in terms of years of
clinical experience (β=0.015, P=0.921), knowledge of TOR (β=0.057,
P=0.509), or attitudes about TOR (β= -0.103, P=0.214). The correlation
between knowledge and attitudes was low (Spearman’s coefficient=0.02,
P=0.795).
Conclusion: Clinical practice
and behaviour of TOR was not demonstrated to have associations with
knowledge or attitude. Status as a Fellow of the Hong Kong College of
Emergency Medicine or Advanced Cardiac Life Support instructor were the
only two parameters identified that had significant relationships with
earlier TOR in medically futile patients with OHCA.
New knowledge added by this study
- Fellowship in emergency medicine and instructorship in resuscitation courses were two independent predictors of less aggressive resuscitation in medically futile patients with out-of-hospital cardiac arrest. Knowledge level and attitude do not predict behaviour and practice well.
- The survey reports knowledge, attitudes, and practice of termination of resuscitation in medically futile situations of out-of-hospital cardiac arrest among emergency physicians in Hong Kong. Early prognostication to identify medically futile patients for diversion of care to bereavement and family support should be part of resuscitation training.
Introduction
Out-of-hospital cardiac arrest (OHCA) is commonly
encountered in emergency departments (EDs), with an incidence rate of 72
per 100 000 person-years in Hong Kong.1
The 30-day survival or survival-to-discharge rate of OHCA patients has
been reported as 2.3% in Hong Kong,1
with only 1.5% of all OHCA patients having good neurological outcomes.1 Within the group of patients in whom resuscitation
failed, a large proportion presented with unwitnessed prehospital
asystolic cardiac arrest. Resuscitation in this group of patients is
considered medically futile, and termination of resuscitation (TOR) is
supported by validated clinical prediction rules.2
3 4
5 6
Therefore, it is reasonable to perform early prognostication and identify
the group of patients in whom resuscitation is medically futile for
familial bereavement support.
The perception of medical futility and the practice
of TOR for patients with OHCA are highly heterogeneous among emergency
physicians in Hong Kong. In addition to patient factors and the
circumstances of the cardiac arrest, decisions about TOR in emergency
rooms are also affected by the knowledge and attitudes of the
resuscitation team about medical futility, the social and cultural beliefs
of relatives and society, and legal considerations. There have been few
reports in the literature about knowledge, attitudes, and practices on
this issue. The objective of this study was to report the knowledge,
attitudes, and practices regarding medical futility and TOR during
management of OHCA in Hong Kong and investigate the relationships of this
knowledge and these attitudes to practice.
Methods
Study setting and participants
A survey on knowledge, attitudes, and behaviours
(KAB) concerning TOR in OHCA was conducted on emergency medicine (EM)
physicians currently working in nine EDs in Hong Kong from January to June
2018. The survey was conducted in the form of printed questionnaires
written in English. Target participants included trainees or Fellows of
the Hong Kong College of Emergency Medicine (Fellows). Doctors registered
under other specialties who were working in EDs were excluded.
Questionnaire tool
A literature search revealed no validated
questionnaires that assess the KAB of physicians on TOR for OHCA.
Therefore, relevant questions on KAB were designed based on multiple
previous studies concerning similar topics.7
8 9
10 Evaluation of the
questionnaire’s internal consistency was performed using Cronbach’s alpha.
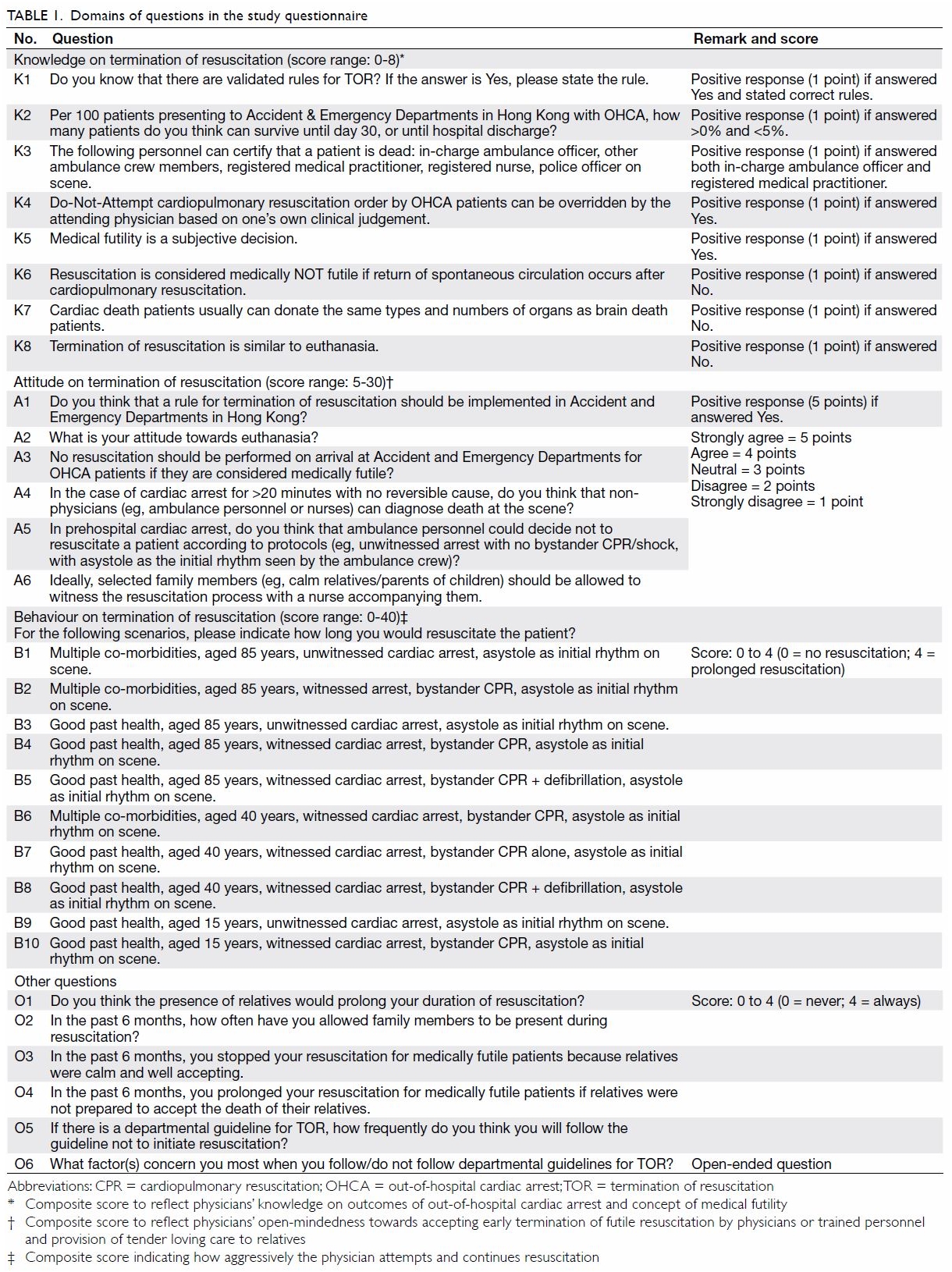
This questionnaire consisted of five domains of
questions in the formats of binary (Yes/No) questions, 5-point Likert
scale questions, and open-ended questions (Table 1). To avoid learning bias, the sequence of
questions was rearranged in the final questionnaire.
The five domains included: (1) demographic data of
the participants; (2) knowledge on TOR; (3) attitudes towards TOR; (4)
behaviours in TOR; and (5) miscellaneous.
The first domain contained questions that obtained
the participants’ baseline characteristics, including their fellowship
status, clinical experience, and any courses attended on topics related to
both resuscitation (such as the Advanced Cardiac Life Support course
[ACLS]) and TOR. The results were used to provide the study’s demographic
data and to analyse the relationship between the participants’ background
and other variables, including KAB.
The second domain consisted of questions about
knowledge of TOR (Table 1). There were eight questions in this domain,
which included facts about OHCA in Hong Kong, current validated rules for
TOR, and issues related to medical futility. Correct answers were given 1
point for each question. A knowledge composite score ranging from 0 to 8
was calculated for each participant by summation of individual questions’
scores. A higher score reflected a higher level of knowledge about OHCA
outcomes and the concept of medical futility.
The third domain included questions assessing
participants’ attitudes towards TOR (Table 1). There was one binary question with a score
of 5 for a positive answer and five Likert-type questions with scores from
1 (strongly disagree) to 5 (strongly agree). An attitude composite score
ranging from 5 to 30 was calculated by summation of individual questions’
scores. A higher score reflected more open-mindedness to accepting early
termination of futile resuscitation and better provision of tender loving
care to relatives.
The fourth domain contained ten clinical scenarios
concerning OHCA (Table 1). Participants were asked their preferred
duration of resuscitation in a range from 0 to 4, with 0 being no
resuscitation and 4 being prolonged resuscitation. A behavioural composite
score was calculated by summation of individual questions’ scores. A
higher score indicated higher aggressiveness towards attempting and
continuing resuscitation. The behavioural composite score does not include
any specification regarding medicolegal consideration, personal beliefs,
or religious context.
The last domain of this questionnaire consisted of
six questions about TOR that were not categorised into KAB domains. This
domain included questions concerning the effects of the presence of
relatives and presence of departmental guidelines on TOR-related
decisions.
The questionnaires were distributed to nine EDs in
Hong Kong by hand and through internal mailings by the Hospital Authority.
One site investigator was designated in each participating ED to
distribute and collect the questionnaires from the participants
anonymously. Anonymous use of the collected data for research purposes was
clearly stated at the start of the questionnaire. All questionnaires were
filled and returned on a voluntary basis.
Statistics
The internal consistency of this questionnaire was
assessed with Cronbach’s alpha. Descriptive analysis is reported for the
questionnaire response of each domain. Median and interquartile range
(IQR) are reported for continuous composite scores, and between-subgroup
comparisons are done using Mann-Whitney U tests. Spearman’s
correlation coefficients were determined between domains. Multiple
regression was modelled to predict the behavioural composite score by
entering the knowledge composite score, attitude composite score, and
relevant participants’ background variables.
Statistical analysis was performed with SPSS
(Windows version 22.0; IBM Corp, Armonk [NY], United States).
Results
A total of 247 doctors in the nine EDs were
eligible for inclusion, and questionnaire forms were distributed to all
eligible physicians. In all, 140 questionnaires were returned (response
rate: 57%). Seventy-nine (56.4%) of the respondents were Fellows, 94
(67.1%) had ≥5 years of experience in EM, 39 (27.9%) had attended the ACLS
within the most recent 2 years, 20 (14.3%) were ACLS instructors, and 45
(32.1%) had attended courses on TOR or breaking bad news.
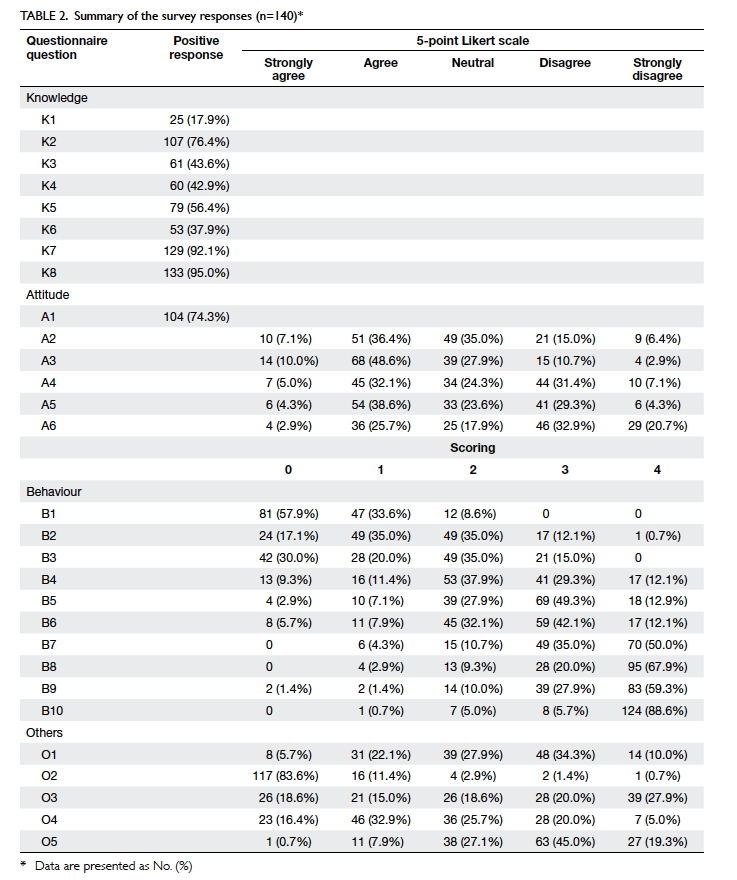
A summary of the responses to the survey is shown
in Table 2. The questions are categorised into
knowledge, attitudes, behaviours, and miscellaneous. The distribution of
responses for each question is shown. The Cronbach’s alpha value of
attitude questions (Questions A2-A5) was 0.603 and that of behaviour
questions (Questions B1-B10) was 0.886. The composite KAB scores of
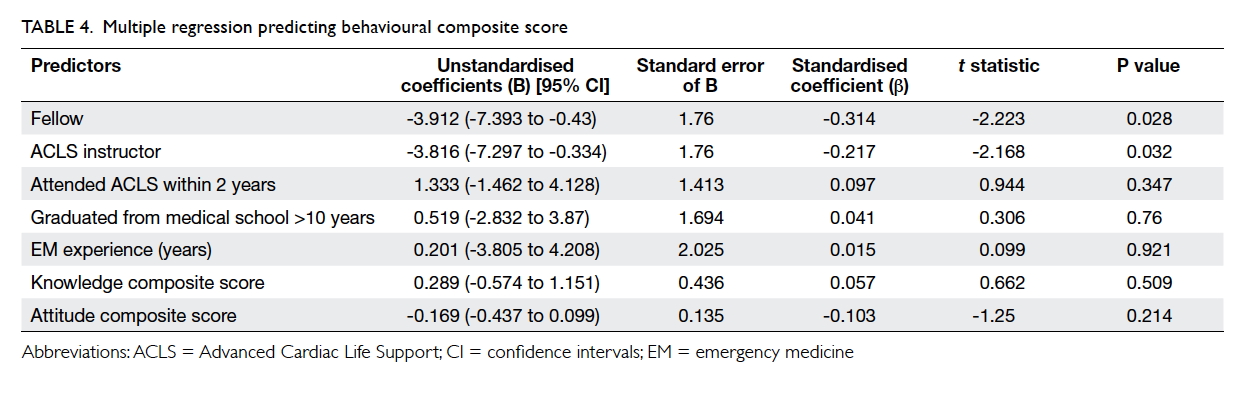
various subgroups are shown in Table 3.
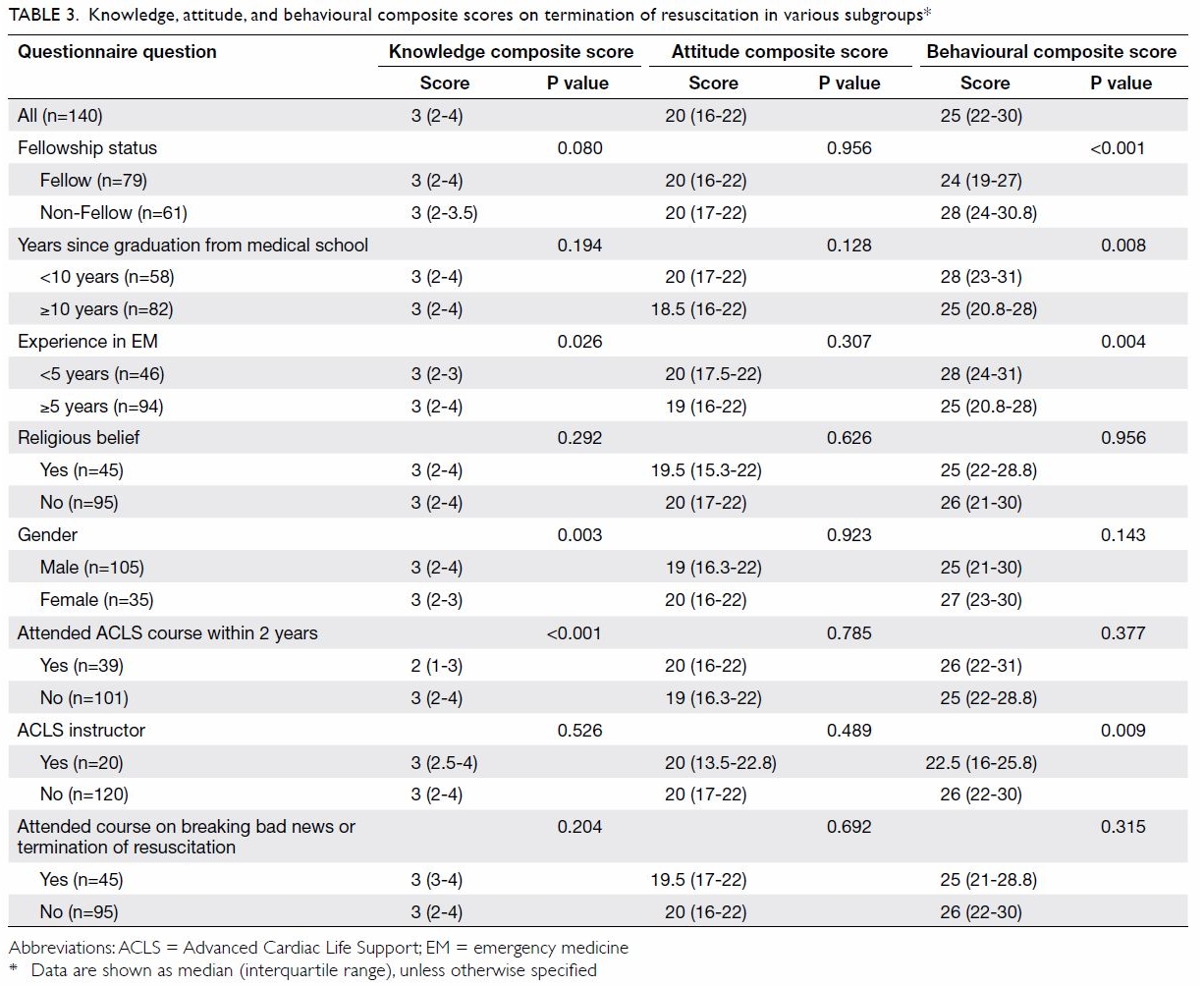
Table 3. Knowledge, attitude, and behavioural composite scores on termination of resuscitation in various subgroups
A comparison of the KAB composite scores in terms
of fellowship status showed no difference between Fellows and non-Fellows
in terms of knowledge composite score (median=3, IQR=2-4 vs median=3,
IQR=2-3.5; P=0.080). There was also no difference between the two groups’
attitude composite scores (median=20, IQR=16-22 vs median=20, IQR=17-22;
P=0.956). However, there was a statistically significant difference in
behavioural composite scores between the two groups (median=24, IQR=19-27
vs median=28, IQR=24-30.8; P<0.001), indicating less aggressive
resuscitation attempted by Fellows despite similar levels of knowledge and
attitudes.
Subgroup analysis showed no differences in
knowledge and attitude composite scores in terms of years postgraduation,
with 10 years as the cut-off (P=0.194 and P=0.128, respectively). However,
a significant difference was found in behavioural composite scores between
the two groups (<10 years vs ≥10 years: median 28 vs 25, P=0.008),
implying that more experienced physicians are less aggressive. Physicians
with ≥5 years of experience in EM, despite having no difference in
knowledge and attitudes, also demonstrated less aggressive resuscitation
practices, with a lower behavioural composite score (median 25 vs 28,
P=0.004).
Regarding attendance of resuscitative courses
(including ACLS), respondents who had attended the course within the
previous 2 years showed no significant differences in either attitude or
behavioural composite scores (P=0.785 and 0.377, respectively) compared
with respondents who had most recently attended a course more than 2 years
ago. In addition, being an ACLS instructor was associated with lower
behavioural composite scores (median 22.5 vs 26, P=0.009) but similar
attitude scores (median 20 vs 20, P=0.489). For respondents who attended
courses on TOR or breaking bad news, there was no difference in KAB
compared with respondents who did not attend any related courses (P=0.204,
0.692, and 0.315, respectively).
Multiple regression to predict behavioural
composite score demonstrated two independent predictors (Table
4). Status as a Fellow was found to be an independent predictor of
lower behavioural composite score, that is, less aggressive resuscitation
(β= -0.314, P=0.028). Status as an ACLS instructor was also found to be an
independent predictor to less aggressive resuscitation (β= -0.217,
P=0.032). Other variables, including ACLS attendance within 2 years, more
than 10 years postgraduation, and years of experience in EM had no
statistically significant association with any difference in behavioural
composite scores.
As this survey aimed to study the relationship
between KAB of TOR, Spearman’s correlation coefficients were calculated to
evaluate the correlations between these three domains. The correlations
between the three domains were all statistically insignificant: knowledge
and attitudes (r=0.02; P=0.795), knowledge and behaviours (r=0.011;
P=0.893), attitudes and behaviours (r=-0.06; P=0.481).
Seventy-five (53.6%) of the participants disagreed
that selected family members (eg, calm relatives/parents of children)
should be allowed to witness the resuscitation process with a nurse
accompanying them. In contrast, 117 (83.6%) indicated that they had never
allowed relatives to be present during resuscitation in the past 6 months.
A Chi squared test with linear-by-linear association indicated a positive
trend (χ2=7.095, P=0.008).
When participants were asked whether a rule for TOR
should be implemented in EDs, 104 (74.3%) gave a positive response. An
open-ended question was asked about the concerns with departmental TOR
guidelines (Question O6). Each written answer given was reviewed by the
authors. The answers were summarised. The main reasons for not following
TOR guidelines were relatives’ concerns (n=25), followed by patient’s
premorbid status/clinical history (n=24), and legal concerns (n=18). A
small number of participants gave answers related to limitations in
flexibility, scientific evidence of TOR rules, usability, etc.
Discussion
An important concept in decisions about TOR is
futility of treatment. This is based on the principle of the patient’s
best interest.11 Medical futility
is a subjective term encompassing a range of possibilities in terms of
whether a patient will benefit from efforts designed to improve his or her
life and survival to discharge from a healthcare facility.12 A treatment that does not benefit the patient, even
if there is a physiological effect, can be considered futile.13 A mere return of spontaneous circulation would not
benefit a patient if a meaningful existence cannot be achieved. On the
contrary, this may even lead to extra burdens on the patients, such as
unmanageable pain and suffering or a traumatic and undignified death.11 Prolonged resuscitation of OHCA patients may also
burden the resources and manpower of EDs and society.14 15 Focusing
resources on patients with very low chances of survival may defer
resuscitative resources away from other patients who are critically ill.16 However, early TOR also has
drawbacks including potential ethical arguments, legal concerns, and
breakdown of communication with relatives of the deceased.
Different guidelines and clinical prediction rules
on TOR have been developed and validated for prognostication and
identification of medically futile patients. Examples include guidelines
from the American Heart Association, the universal TOR guideline, the
modified basic life support TOR rule, the modified advanced life support
TOR rule, and the neurological TOR rule.2
3 4
5 6
Most of these guidelines were validated in the prehospital setting, but
the information is also applicable in the ED setting. In Hong Kong, EM
services do not apply any prehospital TOR rules except in a few
circumstances such as injuries incompatible with life or obvious
post-mortem changes. A 2013 study showed that the percentages of OHCA
patients being resuscitated despite meeting the advanced life support TOR
rule or the neurologic TOR rule were 39.8% and 26.9%, respectively.17 In the group of OHCA patients in whom continuation of
resuscitation was medically futile, care should be focused on
communication with and psychological and bereavement support to the
relatives instead of continuing medical treatment, which would not be
beneficial to patients and relatives.
In this study, two independent variables impacting
less aggressive resuscitation behaviour were identified: status as a
Fellow or ACLS instructor. As we expected, Fellows were less aggressive in
terms of resuscitation of medically futile OHCA patients. However, more
years since graduation and more years of experience in EM, although
expected to be associated with greater general medical knowledge about
resuscitation, were not associated with less aggressiveness in
resuscitation. One of the reasons for this may be the expectations of the
general public, as Fellows are generally more recognised by the public.
They may have more confidence in terminating resuscitation and explaining
the decision to patients’ relatives. Therefore, the concept of medical
futility, TOR clinical prediction rules, communication, and bereavement
skills should receive more emphasis in pre-Fellowship EM training.
Opinions and support from Fellows may also be sought when handling OHCA
patients.
Status as an ACLS instructor was also an
independent predictor of less aggressive resuscitation attempts. Although
their knowledge of TOR was not found to differ significantly from that of
non-ACLS instructors, they should have more knowledge about the
resuscitation process itself. They may potentially know more about the
harm and futility of prolonged resuscitation. Meanwhile, there were no
difference in either attitudes or behaviours regarding TOR between those
who attended an ACLS more or less than 2 years ago. The ACLS focuses on
medical knowledge about advanced life support instead of the
prognostication and management of medically futile cases. For doctors who
had attended courses related to TOR or breaking bad news, no difference
was found in terms of KAB of TOR. One of the reasons for this may be the
content of the course. Some of the courses on breaking bad news focus on
communication skills. Those practices may have a presumptive clinical
scenario, such as explaining the condition of a cardiopulmonary-arrested
patient to his/her relatives with empathy. Rather, the decision of early
TOR and the rationale behind it may not be adequately discussed. More
discussion of medical futility and its ethical basis should be done before
proceeding to the step of communication with relatives.
No correlations were found between physicians’
level of knowledge about TOR, their attitudes towards TOR, and their
aggressiveness with resuscitation. This was not surprising, as many
participants expressed concerns about TOR, including patients’ premorbid
status, clinical histories, reactions from family members, and medicolegal
concerns about early withdrawal and TOR. These factors, which affect the
decision of TOR versus continuation of resuscitation, are likely
independent from physicians’ own knowledge and attitudes. This explains
why having more knowledge or open-mindedness towards acceptance of TOR did
not necessarily lead to less aggressiveness in resuscitation attempts.
Approximately 54% of participants disagreed with
the presence of relatives in resuscitation, and 84% never allowed
relatives to be present during the resuscitation process. This warrants
discussion, as some opinions and studies overseas have suggested that
family members who witnessed the patient’s resuscitation process had
better mental health outcomes irrespective of the patient’s final survival
outcome.18 Family members’
grieving process may also be enhanced.18
However, there are practical considerations, including the limitation of
availability of trained personnel to accompany the family members and
limitations of space in the resuscitation room.
Of our participants, 74% agreed that there is a
need to develop TOR rules in Hong Kong. When participants were asked their
concerns about following TOR rules, many of them responded that potential
medicolegal liability was one of the main problems. This is
understandable, as the tendency towards defensive medical practices has
progressed in recent years. However, prolongation of the resuscitative
process for futile patients, apart from being non-empathetic, might not
make a doctor less vulnerable to complaints. Instead, good communication
with relatives and bereavement support is always the key to reduction of
family members’ misunderstanding and emotional reactions.
Limitations
This study had a few limitations. First, the
response rate was 57%, which is borderline satisfactory. This may result
in volunteer response bias, as doctors who returned the questionnaires
were likely to have more interest in and stronger opinions about TOR. This
may cause an underestimation of the overall aggressiveness of
resuscitation (falsely low behavioural composite scores). In addition, the
study does not include sample size planning.
Another limitation of this study was the
questionnaire contents. As discussed previously, no validated
questionnaires concerning similar topics were discovered by a literature
search. Further, no previous similar studies had been done in Hong Kong.
Therefore, the questions in this survey were designed based on multiple
previous studies with similar topics. There was no external validation of
the questionnaire tool.
The questions on attitudes about TOR assessed the
participants’ attitudes towards aggressiveness of resuscitation (as the
opposite of TOR) and medically futile resuscitation. For questions
concerning TOR-related behaviours, the calculation of composite scores was
based on participants’ self-reported behaviour rather than their actual
practices. Therefore, reporting bias may exist. The reported answers may
underestimate the participants’ aggressiveness in resuscitation, as they
knew that the theme of this study was TOR. Participants may have answered
as if they were being less aggressive.
Another drawback of the behavioural questions is
the arbitrary scale for the scoring. A more objective assessment would be
to quantify the duration of resuscitation in terms of minutes or number of
adrenaline injections. However, as the scenarios only contained simple
patient information, it may be difficult for the participants to comment
quantitatively on the duration of resuscitation. This may lead to further
inaccuracy. Therefore, an arbitrary scale was used, with a reference range
of 0 being no resuscitation and 4 being relatively prolonged resuscitation
for a young, healthy adult.
To minimise this discrepancy, further observational
studies on doctors’ actual performance during TOR could be performed.
Conclusion
Clinical practice and behaviour of TOR were not
demonstrated to have any association with knowledge or attitudes. Status
as a Fellow or ACLS instructor were the only two parameters identified to
have a significant relationship with earlier TOR in medically futile OHCA
patients.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept and design of study: CW So, CT Lui, KL
Tsui.
Acquisition of data: CW So, KL Chan, AKK Law, YK Wong, T Li, CL Wong, SC Leung.
Analysis or interpretation of data: CW So, CT Lui, KL Tsui.
Drafting of the manuscript: CW So, CT Lui, KL Tsui.
Critical revision for important intellectual content: All authors.
Acquisition of data: CW So, KL Chan, AKK Law, YK Wong, T Li, CL Wong, SC Leung.
Analysis or interpretation of data: CW So, CT Lui, KL Tsui.
Drafting of the manuscript: CW So, CT Lui, KL Tsui.
Critical revision for important intellectual content: All authors.
Acknowledgement
The authors thank the Emergency Care Research
Consortium of the Hong Kong College of Emergency Medicine for assistance
with liaison between the participating site investigators. We acknowledge
the coordinators of all participating centres.
Conflicts of interest
The authors have no conflicts of interest to
disclose.
Declaration
This paper was presented to the Education Committee
of the Hong Kong College of Emergency Medicine during the Scientific
Symposium on Emergency Medicine (SSEM) on 26 October 2018 for examination
purpose.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The Research Ethics Office of New Territories West
Cluster waived the need for ethical approval for this questionnaire
survey. This study was conducted in accordance with the Declaration of
Helsinki. The nature and purpose of the study was explained to
participants, and those who returned completed questionnaires were assumed
to have provided consent.
References
1. Fan KL, Leung LP, Siu YC.
Out-of-hospital cardiac arrest in Hong Kong: a territory-wide study. Hong
Kong Med J 2017;23:48-53. Crossref
2. Mancini ME, Diekema DS, Hoadley TA, et
al. Part 3: Ethical issue: 2015 American Heart Association guidelines
update for cardiopulmonary resuscitation and emergency cardiovascular
care. Circulation 2015;132(18 Suppl 2):S383-96. Crossref
3. Kim TH, Shin SD, Kim YJ, Kim CH, Kim JE.
The scene time interval and basic life support termination of
resuscitation rule in adult out-of-hospital cardiac arrest. J Korean Med
Sci 2015;30:104-9. Crossref
4. Ruygrok ML, Byyny RL, Haukoos JS;
Colorado Cardiac Arrest & Resuscitation Collaborative Study Group and
the Denver Metro EMS Medical Directors. Validation of 3 termination of
resuscitation criteria for good neurological survival after
out-of-hospital cardiac arrest. Ann Emerg Med 2009;54:239-47. Crossref
5. Chiang WC, Ko PC, Chang AM, et al.
Predictive performance of universal termination of resuscitation rules in
an Asian community: are they accurate enough? Emerg Med J 2015;32:318-23.
Crossref
6. Cheong RW, Li H, Doctor NE, et al.
Termination of resuscitation rules to predict neurological outcomes in
out-of-hospital cardiac arrest for an intermediate life support
prehospital system. Prehosp Emerg Care 2016;20:623-9.Crossref
7. Bae H, Lee S, Jang HY. The ethical
attitude of emergency physicians towards resuscitation in Korea. J Emerg
Med 2008;34:485-90. Crossref
8. Elo G, Diószeghy C, Dobos M, Andorka M.
Ethical considerations behind the limitation of cardiopulmonary
resuscitation in Hungary—the role of education and training. Resuscitation
2005;64:71-7. Crossref
9. Baird G, Sammy I, Nunes P, Paul J.
Attitudes and practices regarding resuscitation in emergency departments
in Trinidad and Tobago. Emerg Med J 2014;31:889-93. Crossref
10. Einav S, Alon G, Kaufman N, et al. To
resuscitate or not to resuscitate: a logistic regression analysis of
physician-related variables influencing the decision. Emerg Med J
2012;29:709-14. Crossref
11. Hospital Authority, Hong Kong SAR
Government. HA guideline on Do-Not-Attempt cardiopulmonary resuscitation
(DNACPR). 2016. Available from:
http://www.ha.org.hk/haho/ho/psrm/CEC-GE-6_en.pdf. Accessed 26 Aug 2018.
12. The Free Dictionary by Farlex. Medical
futility. Available from:
https://medical-dictionary.thefreedictionary.com/medical+futility.
Accessed 27 Aug 2017.
13. Jecker NS. Medical futility. School of
Medicine, University of Washington. Available from:
https://depts.washington.edu/bioethx/topics/futil.html. Accessed 26 Aug
2018.
14. Millin MG, Khandker SR, Malki A.
Termination of resuscitation of nontraumatic cardiopulmonary arrest:
resource document for the National Association of EMS Physicians position
statement. Prehosp Emerg Care 2011;15:547-54. Crossref
15. Valenzuela TD, Criss EA, Spaite D,
Meislin HW, Wright AL, Clark L. Cost-effectiveness analysis of paramedic
emergency medical services in the treatment of pre-hospital
cardiopulmonary arrest. Ann Emerg Med 1990;19:1407-11. Crossref
16. Millin MG, Galvagno SM. More than 15
minutes of resuscitation prior to termination of resuscitation results in
undue harm to the public health. Am J Emerg Med 2016;34:1689-90. Crossref
17. Chan KM, Lui CT, Tsui KL, Tang YH.
Comparison of clinical prediction rules for termination of resuscitation
of out-of-hospital cardiac arrests on arrival to emergency department.
Hong Kong J Emerg Med 2013;20:343-51. Crossref
18. DeWitt S. Should family-witnessed
resuscitation become our standard? J Emerg Med 2015;49:500-2. Crossref