Hong
Kong Med J 2019 Apr;25(2):127–33 | Epub 28 Mar 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE CME
Non-surgical treatment of knee osteoarthritis
HS Kan1; PK Chan, FHKCOS, FHKAM
(Orthopaedic Surgery)2; KY Chiu, FHKCOS, FHKAM (Orthopaedic Surgery)1; CH Yan, FHKCOS, FHKAM (Orthopaedic
Surgery)1; SS Yeung, MScHC(PT), PDPT3; YL Ng, BSc, MHSc4; KW
Shiu, BNurs(Aust)5; Tegan Ho, BMedSc1
1 Department of Orthopaedics and
Traumatology, The University of Hong Kong, Pokfulam, Hong Kong
2 Department of Orthopaedics and
Traumatology, Queen Mary Hospital, Pokfulam, Hong Kong
3 Department of Physiotherapy, MacLehose
Medical Rehabilitation Centre, Pokfulam, Hong Kong
4 Department of Occupational Therapy,
MacLehose Medical Rehabilitation Centre, Pokfulam, Hong Kong
5 Department of Nursing, MacLehose
Medical Rehabilitation Centre, Pokfulam, Hong Kong
Corresponding author: Dr PK Chan (lewis@ortho.hku.hk)
Abstract
Knee osteoarthritis is one of the most common
degenerative diseases causing disability in elderly patients.
Osteoarthritis is an increasing problem for ageing populations, such as
that in Hong Kong. It is important for guidelines to be kept up to date
with the best evidence-based osteoarthritis management practices
available. The aim of this study was to review the current
literature and international guidelines on non-surgical treatments for
knee osteoarthritis and compared these with the current guidelines in
Hong Kong, which were proposed in 2005. Internationally, exercise
programmes for non-surgical management of osteoarthritis have been
proven effective, and a pilot programme in Hong Kong for comprehensive
non-surgical knee osteoarthritis management has been successful.
Long-term studies on the effectiveness of such exercise programmes are
required, to inform future changes to guidelines on osteoarthritis
management.
Introduction
Conventionally, osteoarthritis (OA) is considered
as progressive wear and tear of articular cartilage. However, recent
evidence has suggested that it is an inflammatory disease of the entire
synovial joint, comprising not only mechanical degeneration of articular
cartilage but also concomitant structural and functional change of the
entire joint, including the synovium, meniscus (in the knee),
periarticular ligament, and subchondral bone.1
Knee osteoarthritis (KOA) is one of the most common
degenerative diseases that causes disability in elderly people. An
epidemiological study by Felson et al2
showed that about 30% of all adults have radiological signs of OA; 8.9% of
the adult population has clinically significant OA of the knee or hip, of
which KOA was the most common type. Another study also showed that the
likelihood of OA increases with age.3
The Chinese population has a similar prevalence rate. A nationwide
population-based study in China showed an 8.1% total incidence rate of
symptomatic KOA and increasing prevalence of KOA with age.4 A study in Hong Kong showed that 7% of men and 13% of
women had KOA.5 It is estimated
that the percentage of older adults in the Hong Kong population will
increase from 16.6% in 2016 to 31.1% by 2036.6
Although clinical guidelines for managing lower
limb osteoarthritis (LLOA) in the primary care setting were proposed in
Hong Kong in 2004,7 comparison with
recently updated international guidelines shows some differences from
management in Hong Kong.
In ageing populations, such as that in Hong Kong,
the prevalence of OA is expected to increase. Therefore, it is of
paramount importance to keep updating OA management guidelines so as to
provide the best possible evidence-based management in the primary
setting. This may help to delay progression into end-stage OA and thus
decrease the need for arthroplasty and alleviate long waiting times (the
average waiting time for arthroplasty in public hospitals in Hong Kong is
66 months).5 The aim of the present
study was to compare and contrast the LLOA management guidelines proposed
in Hong Kong7 with international
guidelines, including the Osteoarthritis Research Society International
(OARSI),8 the American Academy of
Orthopedic Surgeons (AAOS),9 and
the American College of Rheumatology (ACR) [Table 1].10
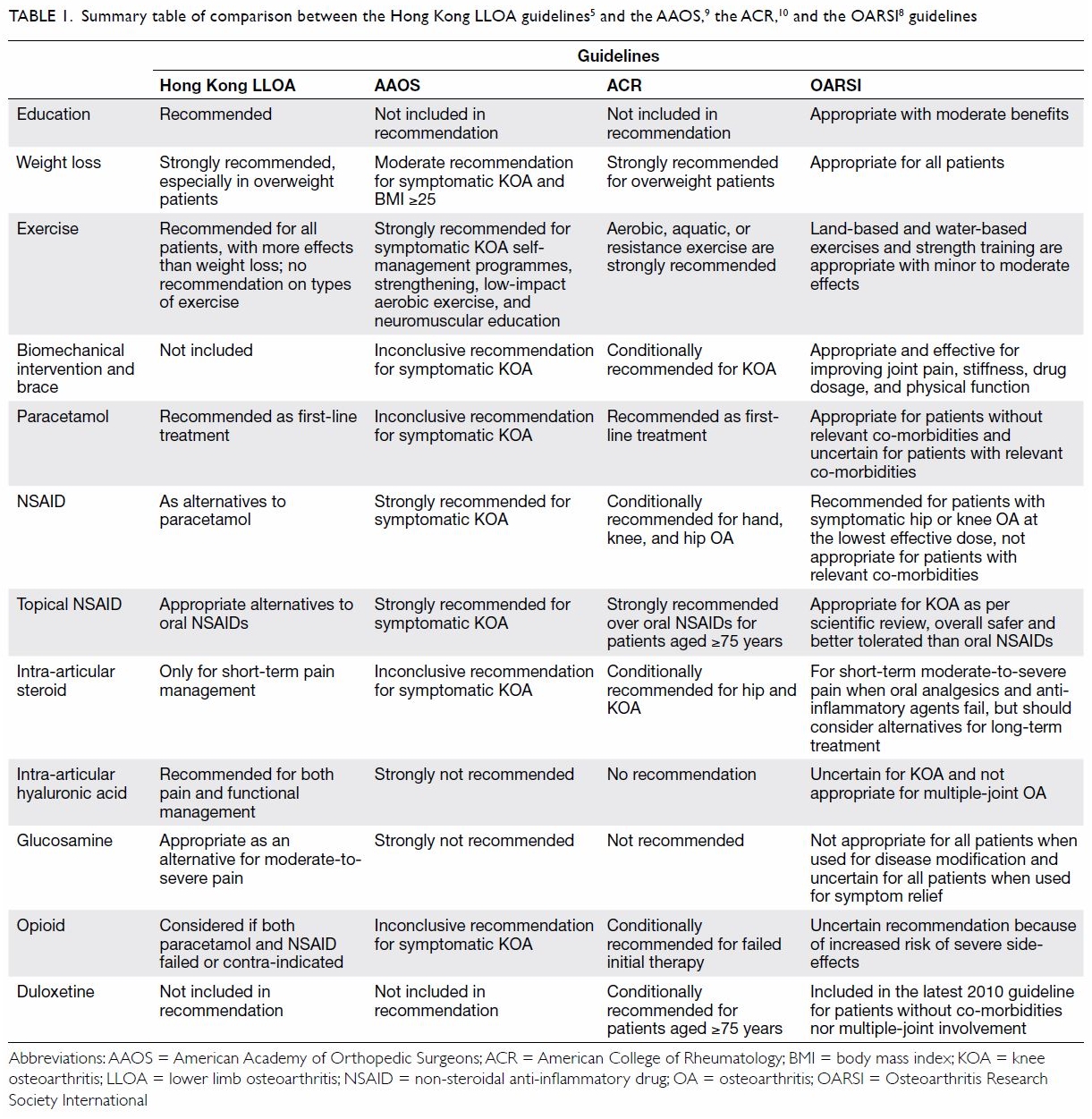
Table 1. Summary table of comparison between the Hong Kong LLOA guidelines5 and the AAOS,9 the ACR,10 and the OARSI8 guidelines
Overview of treatment of knee osteoarthritis
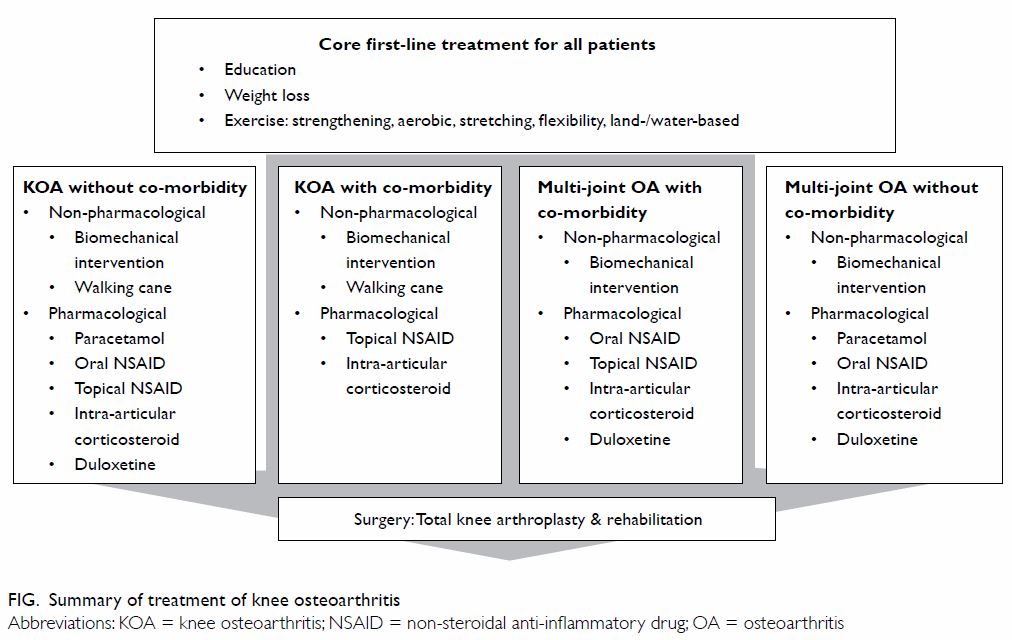
Treatment of KOA can be divided into non-surgical
or surgical treatment. Non-surgical treatment comprises
non-pharmacological and pharmacological treatment, and non-pharmacological
treatment comprises core first-line treatment for all patients with OA,
including education, self-management, exercise, and weight reduction.
Other primary non-pharmacological treatments for KOA include walking canes
and biomechanical interventions like braces and orthosis. Pharmacological
therapy may include the use of paracetamol, topical or oral non-steroidal
anti-inflammatory drugs (NSAIDs), or intra-articular corticosteroids.
Surgical procedures are a last resort for end-stage KOA, the most
effective type of which is total knee arthroplasty with rehabilitation
(Fig).
Non-pharmacological treatment of knee osteoarthritis
Education
Both the Hong Kong LLOA and OARSI guidelines aim to
teach patients more about OA; provide them with information about the
disease process, nature, prognosis, investigation, and treatment options
for OA; facilitate changes in health behaviour; and improve compliance
with doctor advice. Counselling can take the form of telephone-based or
group sessions or spouse-assisted training programmes, and this
counselling works in combination with other treatment approaches.
Weight management
The Hong Kong LLOA and other international
guidelines agree that weight reduction plays a key role in treating all OA
patients. Obesity is strongly associated with an increased risk of
developing OA, the requirement of arthroplasty, and physical disability.11 A meta-analysis reported that
obesity increases the risk of developing KOA five-fold, and overweight
increases the risk two-fold.12 The
main form of weight management is lifestyle modification, which may
include a low-calorie diet, increased physical activity, or anti-obesity
drugs; in severe cases, surgery like gastric bypass, adjustable gastric
banding, or sleeve gastrectomy should be recommended. Recent studies have
proven the significance of weight modification: evidence has shown that
knee pain is reduced by over 50% after body weight reduction by around
10%,13 and weight reduction may
drop the risk of developing symptomatic KOA by 50%.2 It is expected that weight management would also be
effective in Hong Kong. A local study investigating the risk factors of
KOA showed that overweight was the greatest risk factor for KOA in Hong
Kong and that 64% of the investigated Hong Kong patients with KOA were
overweight.5
Exercise
Exercise aims to reduce pain and improve general
mobility and joint function; more intensive exercise can strengthen the
muscle around the knee joint. Exercise is one form of first-line treatment
advocated by the Hong Kong LLOA guidelines. There is no recommendation
regarding the type of exercise to do, suggesting that it has lower
efficacy in reduction of pain and disability compared with weight loss.
Exercise is now universally recommended by the other international
guidelines. Recent studies suggest the important role of exercise in OA
management, and different types of exercise have different benefits in KOA
treatment. Targeted strengthening exercises, aerobic exercise, stretching,
and flexibility exercises are recommended by AAOS, ACR, and OARSI.
A meta-analysis found that land-based exercise
(especially exercise like Tai Chi) has the strongly favourable benefits of
improving pain and physical function in patients with KOA; the duration
and type of exercise programme in the meta-analyses varied widely, but the
general components of the programmes are strength training, active range
of motion exercise, and aerobic activity. Although positive results were
obtained for land-based exercise, they did not favour any specific
exercise regimen or duration.14
A study in 2016 found that water-based exercise has
short-term benefits for function but minor benefits for pain.15 It is suggested for patients with functional or
mobility limitations.
Strength training exercises include primarily
resistance-based lower limb and quadriceps strengthening exercises. A
meta-analysis in 2011 showed moderate benefits of reducing pain and
improving physical function. However, the duration of exercise varied
among these programmes.16
Biomechanical intervention and walking canes
Biomechanical intervention and walking canes are
not included in the Hong Kong LLOA guidelines but are regarded as
appropriate and effective by the OARSI guidelines. A literature review
suggests that knee braces and foot orthoses could have a positive impact
on decreasing pain and stiffness and improving physical function. However,
conclusions about their effectiveness have yet to be made because of the
lack of clinical trials and the heterogeneity of interventions among the
studies reviewed.17 Both the OARSI
and ACR guidelines suggest that walking canes are appropriate for KOA but
not appropriate for multi-joint OA because they may increase weight
loading on other affected joints.18
In contrast, the AAOS guidelines are inconclusive about this topic.
Pharmacological treatment of knee osteoarthritis
Paracetamol
The Hong Kong LLOA guidelines stipulate that
paracetamol is a key medication for knee OA. It is regarded as the
first-line treatment for mild to moderate OA pain because of its efficacy,
safety, and cost, and it is also the preferred essential component of
long-term pain control. However, it is no longer the first-line treatment
suggested by OARSI, as a meta-analysis showed that paracetamol has low
efficacy for pain management.19
The OARSI guidelines recommend that paracetamol be given in conservative
doses and durations, as there is concern regarding an increasing risk of
gastrointestinal disturbance and multi-organ failure.20
Non-steroidal anti-inflammatory drugs
The Hong Kong LLOA and ACR guidelines suggest
NSAIDs as an alternative to paracetamol, whereas the OARSI guidelines
suggest NSAIDs as the preferred first-line pharmacological treatment,
because systematic reviews have found that NSAIDs are superior to
paracetamol for resting and overall pain.21
Although NSAIDs are recommended in patients without risk, OARSI is
reserved in its recommendation for NSAID use in patients with a high risk
of co-morbidities. Non-selective NSAIDs have greater associated upper
gastrointestinal risks, whereas selective NSAIDs have more cardiovascular
side-effects like myocardial infarction; in addition, both selective and
non-selective NSAIDs cause side-effects like hypertension, congestive
heart failure, and renal toxicity. The AAOS recommendations about NSAIDs
are inconclusive for symptomatic KOA. The Hong Kong LLOA guidelines and
all international guidelines strongly suggest that topical NSAIDs (eg,
topical diclofenac) be considered as an option for knee-only OA, but their
applicability for multiple joint OA is still uncertain. Both topical and
oral NSAIDs have similar efficacy and significant benefits over placebo.
Topical ones have less gastrointestinal risk but a higher risk of
dermatological side-effects.22
Intra-articular steroids
The Hong Kong LLOA, ACR, and OARSI guidelines
recommend that steroids only be used in acute exacerbations of joint
inflammation, as frequent use can result in cartilage or joint damage and
increase infection risk. The AAOS recommendation on this topic is
inconclusive.
Intra-articular hyaluronic acid
The Hong Kong LLOA guidelines recommend hyaluronic
acid for management of KOA for both pain reduction and functional
improvement, as it is considered to have effects comparable to those of
oral NSAIDs or steroid injections. However, the AAOS and ACR guidelines do
not recommend the use of hyaluronic acid because of the lack of data from
randomised controlled trials on either its benefits or safety. The OARSI
recommendation is also uncertain because of the inconclusive results of
recent meta-analyses. A meta-analysis with blinded trials found only small
benefits for pain.23
Glucosamine
The Hong Kong LLOA guidelines consider glucosamine
to have moderate to large effects on pain and disability in LLOA compared
with placebo, and it is associated with few side-effects. It is used
commonly as an alternative treatment, especially for mild to moderate KOA.
However, all the international guidelines strongly recommend against the
use of glucosamine because recent randomised controlled trials showed
similar effects to placebo, with independent trials showing smaller
effects than commercially funded ones.24
Opioids
In Hong Kong, opioid analgesics are considered if
paracetamol is inadequate and NSAIDs are contraindicated, ineffective, or
poorly tolerated. The ACR also suggested that opioids may be an
alternative in failed initial therapy. However, with reference to
international guidelines for OA management, we should consider the
long-term overall usefulness of opioids. Although they have benefits for
pain and physical function, compared with those who are not, patients
taking opioids have a chance of adverse withdrawal effects that is 4 times
higher, and a risk of developing serious side events, including fractures
and cardiovascular events, that is 3 times higher.25 International guidelines provide a similar
recommendation, AAOS makes an inconclusive recommendation, and OARSI is
uncertain about opioid use because of the increased risk of side-effects.
Duloxetine
The use of duloxetine is not suggested by the Hong
Kong LLOA guidelines or AAOS. However, OARSI and AAOS suggest that
co-existing depression and neuropathic pain contribute to the overall pain
syndrome, as the pain experienced in OA is multifactorial. A study showed
that duloxetine has pain reduction benefits over placebo.26 Therefore, it is recommended as a potential adjunct
to conventional OA treatment for pain reduction.27
Models of knee osteoarthritis management and comparison
As mentioned above, an increasing number of studies
has proven the effectiveness of exercise and physiotherapy on OA
management; with the increasing ageing of the population, it would be
ideal for Hong Kong to develop a well-established exercise programme for
patients with OA as both a non-surgical treatment and follow-up. There
have already been different well-established exercise programmes for
non-surgical OA management throughout the world, and they have achieved
great outcomes. Successful examples include the Osteoarthritis Chronic
Care Program in Australia (OACCP),28
Better management of patients with OsteoArthritis in Sweden,29 and Good Life with osteoArthritis in Denmark (Table
2).30 All of these
programmes have been proven to improve patients’ pain, mobility, physical
function, and quality of life. The OACCP has also proven that an exercise
programme helps to decrease the demand for arthroplasty; 11% of knee and
4% of hip OA participants who had been waiting for arthroplasty agreed
they no longer needed surgery. Different programmes may have minor
arrangements targeting their patients, but their content and training
duration are generally similar; these programmes consist of education
delivered by physiotherapists and sharing from “expert” patients,
supported self-management, and supervised neuromuscular exercise sessions
of progressive intensity. These programmes usually last at least 3 months
with follow-up for 12 months.
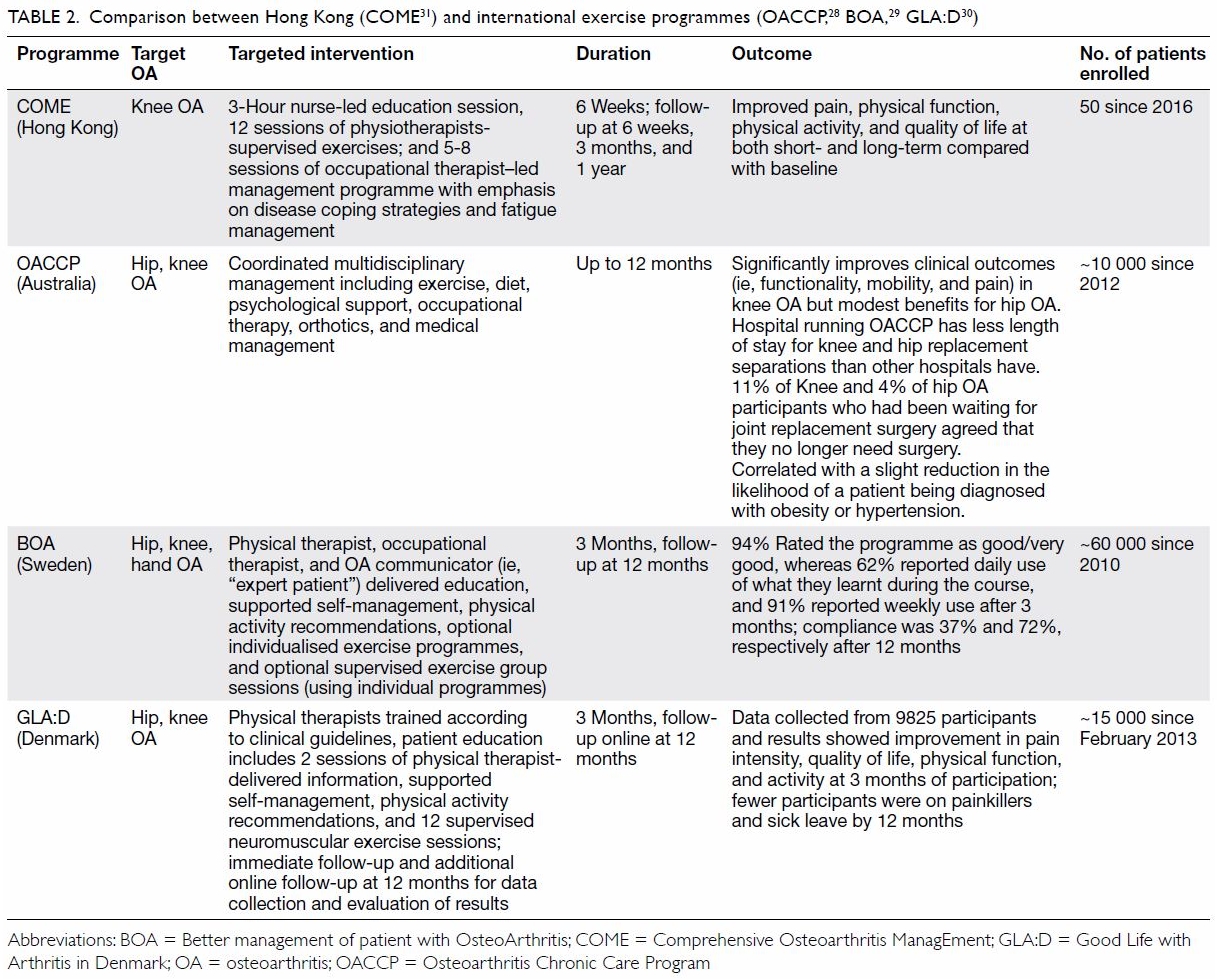
Table 2. Comparison between Hong Kong (COME31) and international exercise programmes (OACCP,28 BOA,29 GLA:D30)
Comprehensive Osteoarthritis ManagEment (COME)
initiated in 2016 is a pioneering programme for Hong Kong.31 The COME programme is a multidisciplinary exercise
programme for non-surgical KOA that consists of a 6-week intensive
training programme: the components include a 3-hour nurse-led education
session, 12 sessions of physiotherapist-supervised exercises; and five to
eight sessions of an occupational therapist–led management programme with
emphasis on disease coping strategies and fatigue management. After 1
year, patients enrolled in the COME programme reported short-term
improvement in Pain Self-Efficacy Questionnaire, Functional Assessment of
Chronic Illness Therapy–Fatigue Scale, physical capacity assessed by
quadriceps strength, and physical function assessed by one-minute chair
test. One-year improvement showed in Patient-Specific Functional Scale,
Chinese version of Self-Efficacy of Exercise, and weekly time spent for
exercise (Table 3).
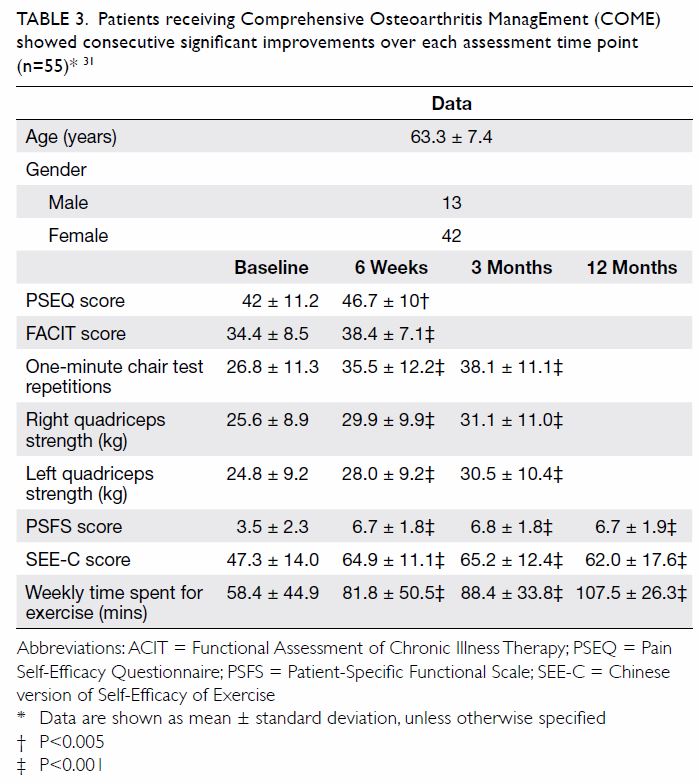
Table 3. Patients receiving Comprehensive Osteoarthritis ManagEment (COME) showed consecutive significant improvements over each assessment time point (n=55)31
Conclusion
In ageing populations, the prevalence of KOA is
expected to increase; thus, there is a need for consensus on non-surgical
OA management, so as to improve outcomes for patients with OA and to
decrease the burden of arthroplasty. Various exercise programmes for
non-surgical OA management have been shown to be effective for improvement
of pain, physical function, mobility, and quality of life, and these
programmes have even decreased the need and waiting times for
arthroplasty. Long-term follow-up of such exercise programmes should be
considered to further assess their outcomes.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design: RHS Kan, PK Chan, KY Chiu, CH
Yan.
Acquisition of data: T Ho.
Analysis or interpretation of data: SS Yeung, YL Ng, KW Shiu.
Drafting of the manuscript: RHS Kan.
Critical revision for important intellectual content: RHS Kan, PK Chan, KY Chiu, CH Yan, T Ho.
Acquisition of data: T Ho.
Analysis or interpretation of data: SS Yeung, YL Ng, KW Shiu.
Drafting of the manuscript: RHS Kan.
Critical revision for important intellectual content: RHS Kan, PK Chan, KY Chiu, CH Yan, T Ho.
Conflicts of interest
No conflicts of interest are declared by the
authors.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
References
1. Mobasheri A, Batt M. An update on the
pathophysiology of osteoarthritis. Ann Phys Rehabil Med 2016;59:333-9. Crossref
2. Felson DT, Zhang Y, Anthony JM, Naimark
A, Anderson JJ. Weight loss reduces the risk for symptomatic knee
osteoarthritis in women. The Framingham Study. Ann Intern Med
1992;116:535-9. Crossref
3. Michael JW, Schlüter-Brust KU, Eysel P.
The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of
the knee. Dtsch Arztebl Int 2010;107:152-62. Crossref
4. Tang X, Wang S, Zhang Y, Niu J, Tao K,
Lin J. The prevalence of symptomatic knee osteoarthritis in China: results
from China health and retirement longitudinal study. Osteoarthritis
Cartilage 2015;23(Suppl 2):A176-7. Crossref
5. The Chinese University of Hong Kong.
Osteoarthritis in Hong Kong Chinese—prevalence, aetiology and prevention.
2001. Available from: http://www.cuhk.edu.hk/ipro/010306e.htm. Accessed 14
Dec 2018.
6. Census and Statistics Department, Hong
Kong SAR Government. Hong Kong population projections for 2017-2066.
Available from:
https://www.censtatd.gov.hk/media_workers_corner/pc_rm/hkpp2017_2066/index.jsp.
Accessed 14 Dec 2018.
7. Department of Community and Family
Medicine, Chinese University of Hong Kong; Centre for Health Education and
Health Promotion. Clinical guidelines for managing lower-limb
osteoarthritis in Hong Kong primary care setting. Department of Community
and Family Medicine, Chinese University of Hong Kong; 2004.
8. McAlindon TE, Bannuru RR, Sullivan MC,
et al. OARSI guidelines for the non-surgical management of knee
osteoarthritis. Osteoarthritis Cartilage 2014;22:363-88. Crossref
9. Jevsevar DS. Treatment of osteoarthritis
of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg
2013;21:571-6. Crossref
10. Hochberg MC, Altman RD, April KT, et
al. American College of Rheumatology 2012 recommendations for the use of
nonpharmacologic and pharmacologic therapies in osteoarthritis of the
hand, hip, and knee. Arthritis Care and Res (Hoboken) 2012;64:465-74. Crossref
11. Wluka AE, Lombard CB, Cicuttini FM.
Tackling obesity in knee osteoarthritis. Nat Rev Rheumatol 2013;9:225-35.
Crossref
12. Zheng H, Chen C. Body mass index and
risk of knee osteoarthritis: systematic review and meta-analysis of
prospective studies. BMJ Open 2015;5:e007568. Crossref
13. Vincent HK, Heywood K, Connelly J,
Hurley RW. Obesity and weight loss in the treatment and prevention of
osteoarthritis. PM R 2012;4(5 Suppl):S59-67. Crossref
14. Kang JW, Lee MS, Posadzki P, Ernst E.
T’ai chi for the treatment of osteoarthritis: a systematic review and
meta-analysis. BMJ Open 2011;1:e000035. Crossref
15. Bartels EM, Juhl CB, Christensen R, et
al. Aquatic exercise for the treatment of knee and hip osteoarthritis.
Cochrane Database Syst Rev 2016;(3):CD005523. Crossref
16. Jansen MJ, Viechtbauer W, Lenssen AF,
Hendriks EJ, de Bie RA. Strength training alone, exercise therapy alone,
and exercise therapy with passive manual mobilisation each reduce pain and
disability in people with knee osteoarthritis: a systematic review. J
Physiother 2011;57:11-20. Crossref
17. Raja K, Dewan N. Efficacy of knee
braces and foot orthoses in conservative management of knee
osteoarthritis: a systematic review. Am J Phys Med Rehabil 2011;90:247-62.
Crossref
18. Jones A, Silva PG, Silva AC, et al.
Impact of cane use on pain, function, general health and energy
expenditure during gait in patients with knee osteoarthritis: a randomised
controlled trial. Ann Rheum Dis 2012;71:172-9. Crossref
19. Bannuru RR, Dasi UR, McAlindon TE.
Reassessing the role of acetaminophen in osteoarthritis: systematic review
and meta-analysis. Osteoarthritis Cartilage 2010;18(Suppl 2):S250. Crossref
20. Craig DG, Bates CM, Davidson JS,
Martin KG, Hayes PC, Simpson KJ. Staggered overdose pattern and delay to
hospital presentation are associated with adverse outcomes following
paracetamol-induced hepatotoxicity. Br J Clin Pharmacol 2012;73:285-94. Crossref
21. Towheed TE, Maxwell L, Judd MG, Catton
M, Hochberg MC, Wells G. Acetaminophen for osteoarthritis. Cochrane
Database Syst Rev 2006;(1):CD004257. Crossref
22. Chou R, Helfand M, Peterson K, Dana T,
Roberts C. Comparative effectiveness and safety of analgesics for
osteoarthritis. Rockville, MD: Agency for Healthcare Research and Quality
(US); 2006.
23. Rutjes AW, Jüni P, da Costa BR, Trelle
S, Nüesch E, Reichenbach S. Viscosupplementation for osteoarthritis of the
knee: a systematic review and meta-analysis. Ann Intern Med
2012;157:180-91. Crossref
24. Zhang W, Nuki G, Moskowitz RW, et al.
OARSI recommendations for the management of hip and knee osteoarthritis:
part III: changes in evidence following systematic cumulative update of
research published through January 2009. Osteoarthritis Cartilage
2010;18:476-99. Crossref
25. da Costa BR, Nüesch E, Kasteler R, et
al. Oral or transdermal opioids for osteoarthritis of the knee or hip.
Cochrane Database Syst Rev 2014;(9):CD003115. Crossref
26. Chappell AS, Desaiah D, Liu-Seifert H,
et al. A double-blind, randomized, placebo-controlled study of the
efficacy and safety of duloxetine for the treatment of chronic pain due to
osteoarthritis of the knee. Pain Pract 2011;11:33-41. Crossref
27. Yu SP, Hunter DJ. Managing
osteoarthritis. Aust Prescr 2015;38:115-9. Crossref
28. Deloitte Access Economics.
Osteoarthritis Chronic Care Program evaluation. Agency for Clinical
Innovation. 2014. Available from:
https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/259794/oaccp-evaluation-feb-2015.pdf.
Accessed 15 Dec 2018.
29. Thorstensson CA, Garellick G, Rystedt
H, Dahlberg LE. Better management of patients with OsteoArthritis:
development and nationwide implementation of an evidence-based supported
osteoarthritis self-management programme. Musculoskeletal Care
2015;13:67-75. Crossref
30. Skou ST, Roos EM. Good Life with
osteoarthritis in Denmark (GLA:DTM): a nationwide implementation of
clinical recommendations of education and supervised exercise in knee and
hip osteoarthritis. Osteoarthritis Cartilage 2017;25(Suppl 1):S389-90. Crossref
31. Chan PK, Yeung SS, Siu SW, et al.
Comprehensive Osteoarthritis Management (COME) Programme—Multidisciplinary
exercise training programme for patients with age-related osteoarthritis
of knee. Hong Kong. Proceedings of the 13th International Symposium on
Healthy Aging “Aging, Health, Happiness”; 2018 Mar 10-11; Hong Kong. Hong
Kong: LKS Faculty of Medicine, The University of Hong Kong; 2018: 70.