Hong
Kong Med J 2019 Feb;25(1):13–20 | Epub 18 Jan 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Survey on prevalence of lower urinary tract symptoms in
an Asian population
CH Yee, MB, BS, FRCSEd; CK Chan, MB, ChB, FRCSEd;
Jeremy YC Teoh, MB, BS, FRCSEd; Peter KF Chiu, MB, ChB, FRCSEd; Joseph HM
Wong, MB, BS, FRCSEd; Eddie SY Chan, MB, ChB, FRCSEd; Simon SM Hou, MB,
BS, FRCSEd; CF Ng, MB, BS, FRCSEd
SH Ho Urology Centre, The Chinese University of
Hong Kong, Shatin, Hong Kong
Corresponding author: Dr CH Yee (yeechihang@surgery.cuhk.edu.hk)
Abstract
Introduction: Lower urinary
tract symptoms (LUTS) have a strong effect on socio-economic and
individual quality of life. The aim of the present study was to
investigate the prevalence of LUTS in an Asian population.
Methods: A telephone survey of
individuals aged ≥40 years and of Chinese ethnicity was conducted. The
survey included basic demographics, medical and health history, drinking
habits, International Prostate Symptom Score, overactive bladder symptom
score, Patient Health Questionnaire (PHQ-9) score, and Short Form
(SF)–12v2 score.
Results: From March to May 2017,
18 881 calls were made, of which 1543 fulfilled the inclusion criteria.
In the end, 1000 successful respondents were recruited (302 men and 698
women). Age-adjusted prevalence of overactive bladder syndrome was
15.1%. The older the respondent, the more prevalent the storage symptoms
and voiding symptoms (storage symptoms: r=0.434, P<0.001;
voiding symptom: r=0.190, P<0.001). Presence of hypertension
and diabetes were found to be significantly and positively correlated
with storage and voiding symptoms. Storage and voiding symptoms were
found to affect PHQ-9 scores (storage symptoms: r=0.257,
P<0.001; voiding symptoms: r=0.275, P<0.001) and SF-12v2
scores (storage symptoms: r=0.467, P<0.001; voiding symptoms:
r=0.335; P<0.001). Nocturia was the most prominent symptom
among patients who sought medical help for their LUTS.
Conclusions: Lower urinary tract
symptoms are common in Asian populations. Both storage and voiding
symptoms have a negative impact on mental health and general well-being
of individuals.
New knowledge added by this study
- Past studies on lower urinary tract symptoms (LUTS) prevalence have mainly involved men. The present study provides data on the prevalence of LUTS in both sexes.
- The present study is among the few studies which have correlated LUTS with general well-being and mental health.
- There is a discrepancy between LUTS and medical help seeking behaviour. The present study provides insight into symptoms that drive patients to seek medical help.
- Understanding the prevalence of LUTS will help estimate the associated workload and expense needed to take care of this group of patients.
- The discrepancy between LUTS prevalence and the medical help seeking behaviour of patients with LUTS suggests a need for public health education.
Introduction
Lower urinary tract symptoms (LUTS) can affect
patients of both sexes and of all ages.1
Although LUTS are regarded by the most cultures as an inevitable
consequence of ageing, bother from LUTS varies among populations.2 Assessment of bother from symptoms is important,
because the degree of bother affects quality of life (QoL) and medical
help seeking behaviour.3 4
There are few studies investigating the correlation
between LUTS and drinking habits, especially among Asian populations.
Daily routines and dietary habits are largely dependent on cultural
background; therefore, LUTS might vary in this perspective. In addition,
up-to-date evidence on the impact of LUTS on mental health, as well as on
the general well-being of an individual, is scarce. Most studies have
investigated LUTS as a collective symptom entity.5
Few studies have investigated the relationship between individual symptoms
and psychological stress.
The purpose of the present study is to provide an
updated perspective on LUTS in an Asian population including both men and
women. The present study aimed to clarify the prevalence of the
subcategories of LUTS—voiding symptoms, storage symptoms, and
nocturia—through a telephone survey. Furthermore, we investigated medical
background and lifestyle factors that might have precipitated LUTS. Last,
we assessed the effect of LUTS on the mental health and general well-being
of individual patients. We also evaluated the level of bother caused by
individual symptoms in relation to medical help seeking behaviour.
Methods
This was a random telephone survey of the general
population in Hong Kong. Inclusion criteria were men or women aged ≥40
years of Chinese ethnicity. Subjects who were not able to comprehend the
telephone survey were excluded from the study. Local census data report a
≥40-year-old population of 3 875 800 in 2013.6
Anticipating a confidence level of 95% and margin of error of 3%, 1000
respondents were targeted to complete the survey.
The survey consisted of seven parts. Basic
demographics were collected, including age, sex, marital status, education
level, occupation, and individual monthly income. Medical background and
drinking habits were explored by questions on smoking history, beverage
consumption habits, general medical and mental health history, urological
history, and medical help seeking behaviour. Any LUTS were assessed with
the International Prostate Symptom Score (IPSS) or the overactive bladder
symptom score.7 The Patient Health
Questionnaire-9 (PHQ-9) was used to assess depressive symptoms among the
respondents. The PHQ-9 scores ≥10 have a sensitivity of 88% and a
specificity of 88% for major depression. The PHQ-9 scores of 5, 10, 15,
and 20 represent mild, moderate, moderately severe, and severe depression,
respectively.8 The Short Form
(SF)–12v2 Health Survey was used to assess health-related QoL. The
International Index of Erectile Function was used to assess sexual
function in male respondents who were sexually active in the preceding 4
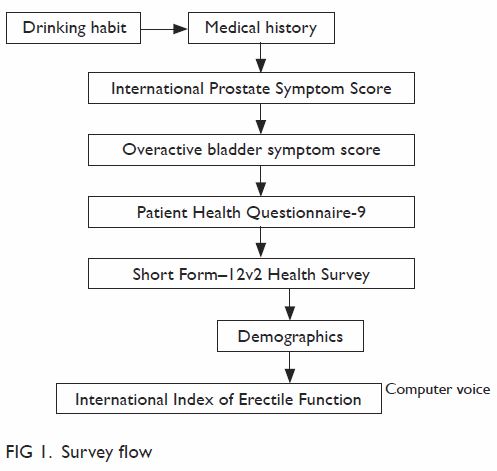
weeks.9 Figure 1 shows the survey question flow. To avoid
unnecessary embarrassment and to improve compliance, questions on sexual
health were asked by a pre-recorded computer-generated voice programme.
Subjects answered the questions by pressing the appropriate number key on
the phone keypad.
The interviews were carried out from March to May
2017. To minimise the sampling error, telephone numbers were first
selected randomly from an updated telephone directory as seed numbers.
Another three sets of numbers were then generated using randomisation of
the last two digitals to recruit unlisted numbers. Duplicate numbers were
screened out, and the remaining numbers were mixed in a random order to
become the final sample. Interviews were carried out by experienced
interviewers, between 18:00 and 22:00 on weekdays or at other convenient
times, including weekends and public holidays, arranged with suitable
subjects. Upon successful contact with a target household, one qualified
member of the household was selected among those family members using the
last-birthday random selection method (ie, the respondent aged ≥40 years
in a household who had most recently had a birthday would be selected to
participate in the telephone interview). Principles of the Declaration of
Helsinki were followed. The study was performed in compliance with Good
Clinical Practice. All participants provided informed consent before
participating in the study.
Descriptive statistics were used to characterise
the clinical characteristics of the survey cohort. Spearman correlation
was used to investigate the relationships between different age-groups and
severity of LUTS. Chi squared test or Fisher’s exact test was applied for
categorical data. Univariate and multivariable logistic regression
analyses were performed to identify clinical covariates that were
significantly associated with LUTS. The P value of <0.05 were
considered statistically significant. The SPSS (Windows version 24.0; IBM
Corp, Armonk [NY], US) was used for all calculations.
Results
A total of 18 881 calls were made, among which 17
338 were invalid cases, including non-residential lines, invalid lines,
non-eligible respondents, or having the line cut immediately before the
survey could start. Another 543 eligible respondents were excluded because
they refused to participate in the survey after being informed of the
nature of the study. In the end we received 1000 valid responses,
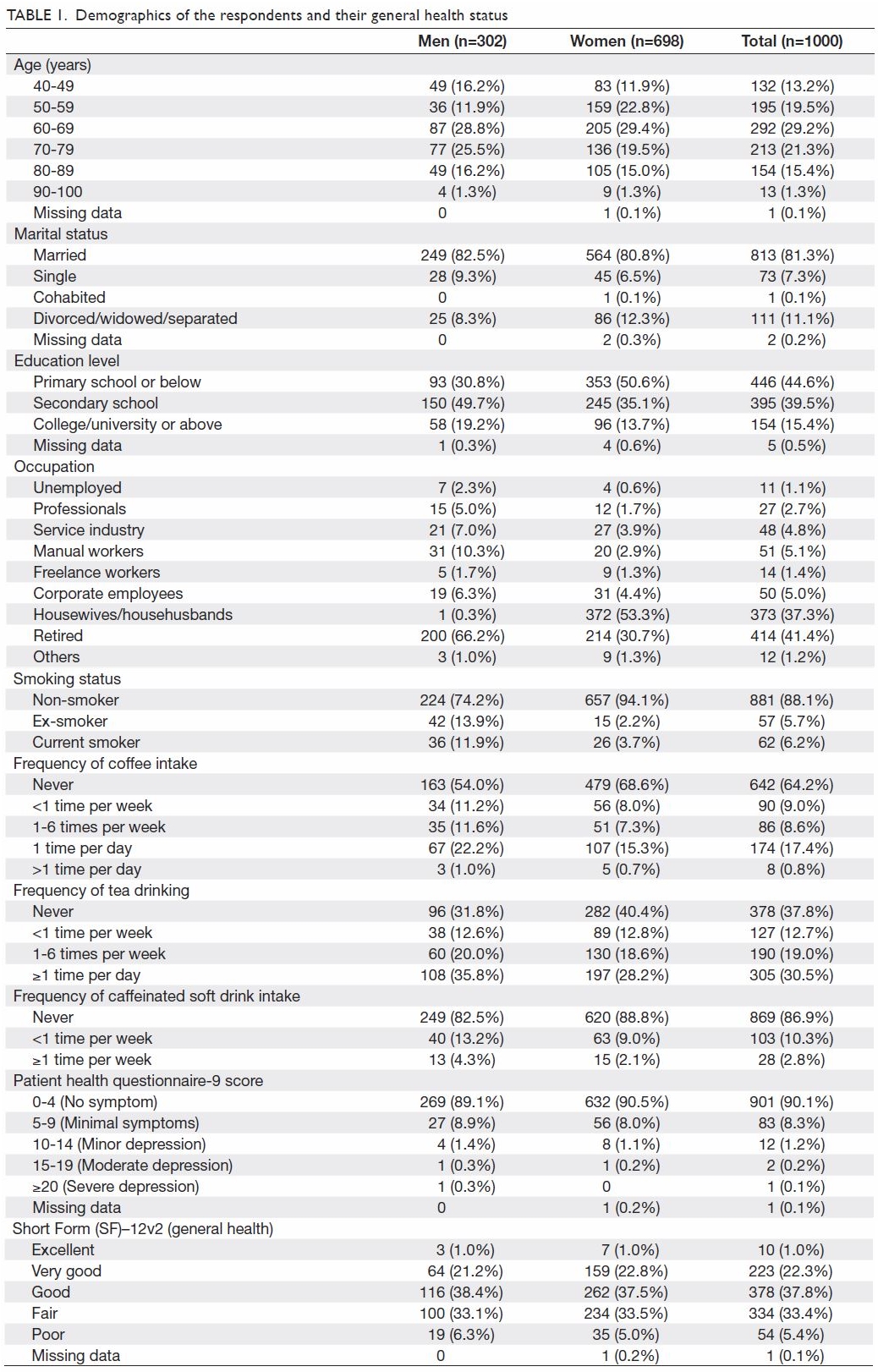
achieving a response rate of 64.8% after excluding the invalid numbers. Table 1 includes the demographics of the respondents
and their drinking habits. Most respondents did not regularly drink
coffee, but 30.5% of respondents reported drinking tea more than once per
day.
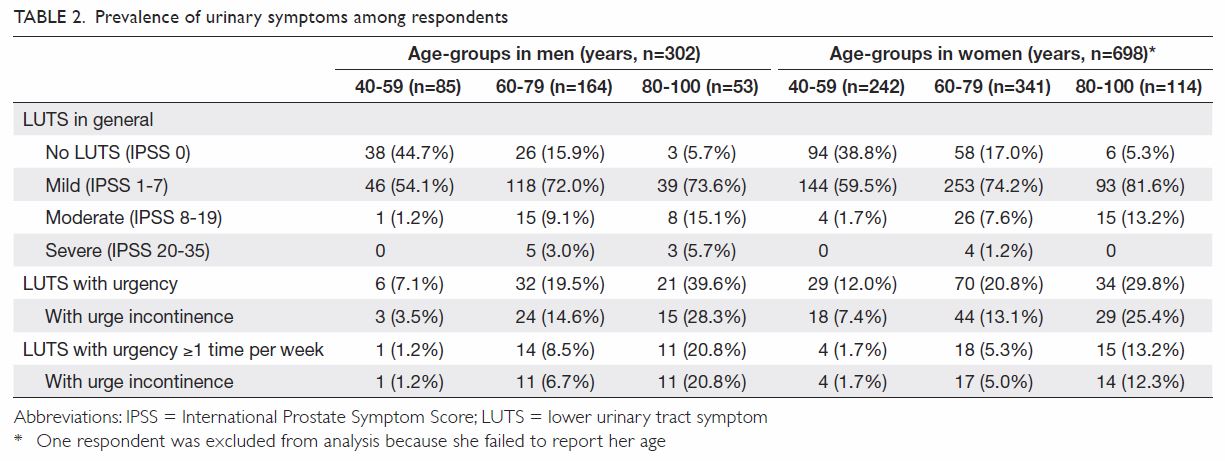
In total, 774 respondents (77.4%) reported a
certain degree of LUTS (Table 2). Among respondents with LUTS, 89.5% had
mild symptoms, 8.9% had moderate symptoms, and 1.6% experience severe
symptoms. Men had more LUTS than did women (mean ± standard deviation
[SD]: men, 3.62 ± 4.86; women, 2.56 ± 3.34; P=0.002). The older the
subject, the poorer the LUTS and QoL scores (mean IPSS: 40-59 years, 1.37
± 2.05; 60-79 years, 3.32 ± 4.28; ≥80 years, 4.48 ± 4.45; P<0.001; mean
QoL score: 40-59 years, 1.15 ± 0.91; 60-79 years, 1.85 ± 1.13; ≥80 years,
2.25 ± 1.13; P<0.001). In the storage symptom domain of IPSS, sex did
not show any significant difference in mean total storage symptom score
(men, 2.32 ± 2.48; women, 1.91 ± 1.97; P=0.052). The older the age, the
more prevalent the storage and voiding symptoms (storage symptom score: r=0.434,
P<0.001; voiding symptom score: r=0.190, P<0.001). Mean
total storage symptom score across different age-groups were: 40-59 years,
1.01 ± 1.29; 60-79 years, 2.30 ± 2.27; ≥80 years, 3.23 ± 2.25; P<0.001.
The age-adjusted prevalence of any urgency symptom in our survey was 15
096 per 100 000 population. If we only include symptoms of urgency more
than once per week, the age-adjusted prevalence was 4070 per 100 000
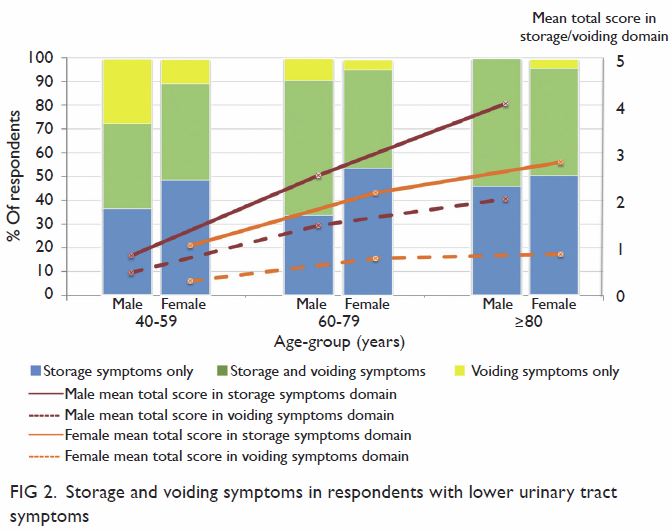
population. Furthermore, more storage symptoms than voiding symptoms were
experienced by respondents at any age-group (Fig 2).
If we exclude nocturia 1 time per night only as
part of LUTS or part of storage symptoms, a total of 191 (63.2%) men were
found to have LUTS in this survey. In this group of respondents, 71
(37.2%) reported only having storage symptoms, 19 (9.9%) reported only
having voiding symptoms, and 101 (52.9%) reported having both storage and
voiding symptoms. Similarly, 348 (49.9%) women were found to have LUTS:
181 (52.0%) reported only having storage symptoms, 19 (5.5%) reported only
having voiding symptoms, and 148 (42.5%) reported having both storage and
voiding symptoms.
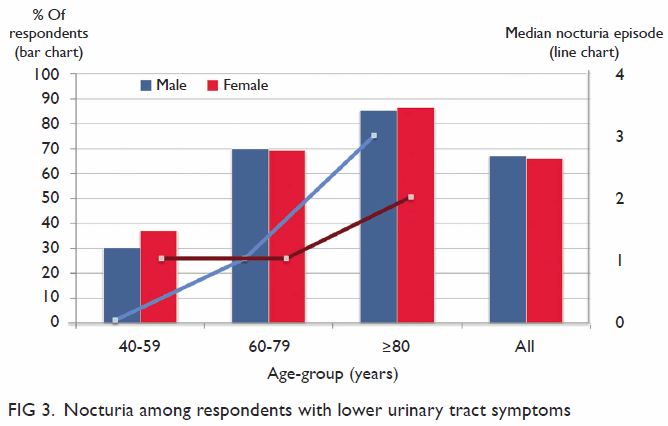
Figure 3 shows the prevalence of nocturia among the
respondents with LUTS. Among those with LUTS, 128 (67.0%) men and 230
(66.1%) women reported having nocturia twice or more per night. The median
number of nocturia episodes increased with age (men, r=0.510;
P<0.001; women, r=0.418; P<0.001).
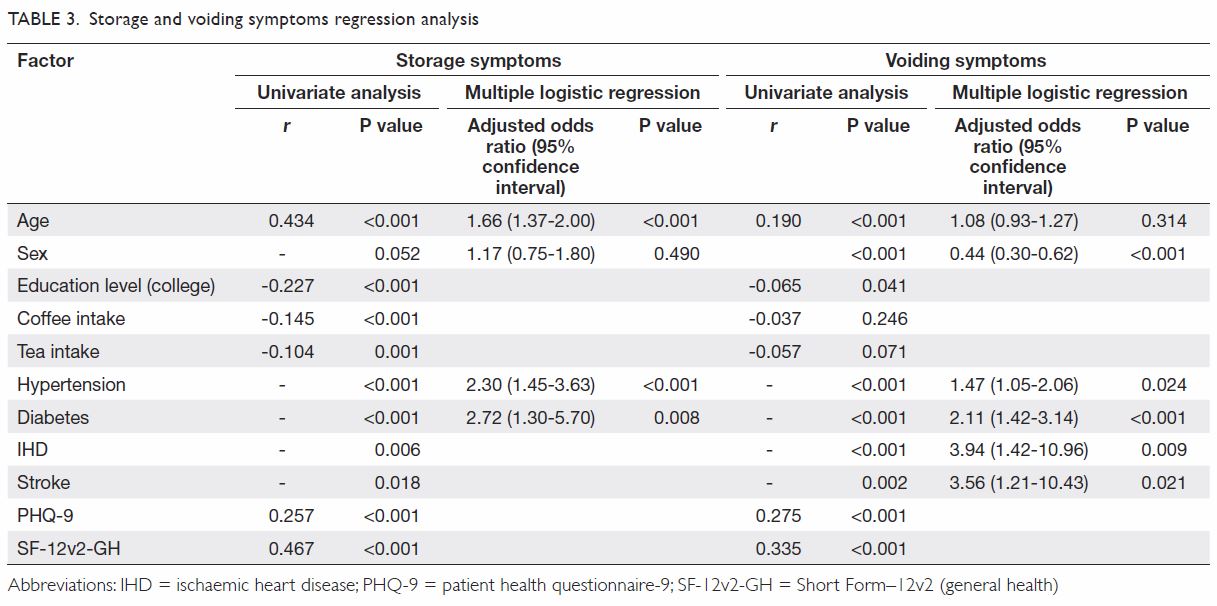
Table 1 includes the general health status and
mental health status of the respondents by means of SF-12v2 score and PHQ
score, respectively. As shown in Table 3, both PHQ-9 scores and SF-12v2 scores were
found to be correlated with both storage symptoms and voiding symptoms.
The higher the PHQ-9 score—indicating more prominent depressive
symptoms—the more significant the LUTS. Similarly, in the SF-12v2
assessment of general health, the higher the score—indicating poorer
health—the more significant LUTS. Storage symptoms and voiding symptoms
were found to be negatively correlated with all components of the SF-12v2.
The results of storage and voiding symptoms
regression analysis are shown in Table 3. Age, presence of hypertension, and diabetes
were found to be significantly correlated with storage symptoms. In
contrast, male sex, presence of hypertension, diabetes, ischaemic heart
disease, and stroke were found to be significantly positively correlated
with voiding symptoms.
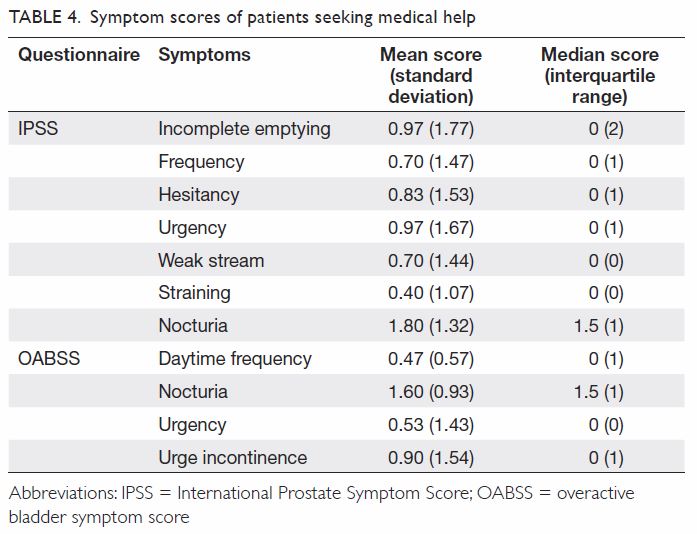
Concerning medical help seeking behaviour among
men, 37.5% of men with severe LUTS, 16.7% with moderate LUTS, and 7.9%
with mild LUTS sought medical help. No women with moderate LUTS sought
medical help. For women with mild LUTS, 2.5% sought medical help. Among
the patients with LUTS who sought medical help, the most prominent
symptoms were nocturia (mean IPSS, 1.80±1.32) and urgency (mean IPSS,
0.97±1.67).
Discussion
In general, LUTS include storage symptoms and
voiding symptoms. Storage symptoms include urinary frequency, nocturia,
urinary urgency, and urinary incontinence. Voiding symptoms include slow
stream, intermittent stream, hesitancy, and straining.10
According to our survey, 77.8% of men and 77.3% of
women aged ≥40 years reported at least mild degree of LUTS according to
IPSS assessment. This prevalence was relatively lower than an internet
survey carried out in mainland China, Taiwan and South Korea, which
reported 86.8% of participants having at least mild symptoms on IPSS.1 However, our findings were comparable to the EpiLUTS
study performed in the US, the United Kingdom and Sweden, which
demonstrated the prevalence of at least one LUTS was 72.3% for men and
76.3% for women.11 In a study of
LUTS in Canada, Germany, Italy, Sweden, and the United Kingdom, Irwin et
al12 reported an even lower
prevalence of LUTS, with an overall prevalence of any LUTS of 62.5% in men
and 66.6% in women. Although such differences in LUTS prevalence across
studies could be attributed to different populations, different cultural
backgrounds or methodological variations could also account for this
observation. Linguistic interpretation discrepancy and different levels of
severity or frequency being used to determine the presence of symptoms
would also generate different results. In addition, changes in general
health awareness and in the socio-economic environment might also effect
survey outcomes. Furthermore, some studies have suggested seasonal
variations of LUTS, with symptoms being more prominent in winter.13 14 Our
survey was carried out in spring and early summer, which could possibly
account for our results falling into the median range in the literature.
Overactive bladder is a subset of storage LUTS,
currently defined by the International Continence Society as urgency, with
or without urgency incontinence, usually with frequency and nocturia.10 Our survey included overactive bladder symptom score
as one of the tools to assess the prevalence of storage symptoms in our
population. In the present study, the prevalence of any experience of
urgency was 19.5% for men and 19.1% for women. This is in line with survey
results from Europe, where Milsom et al15
reported the prevalence of overactive bladder symptoms to be 16.6%, and
from the US, where Stewart et al16
reported the prevalence of overactive bladder symptoms to be 16.0% in men
and 16.9% in women. However, for clinically significant overactive bladder
symptoms, urgency must be happening more than once per week. With this
refinement, our study found that 8.6% of men and 5.3% of women reported
urgency more than once per week. This group of patients warrants
urological attention and intervention.
Voiding symptoms that are often associated with
bladder outlet obstruction in men were also found to be common among
women. In accordance with other studies in the literature,1 11 12 our survey confirmed that the prevalence of LUTS
increases with age. In particular, storage symptoms were reported more
often than voiding symptoms (Fig 2). Furthermore, age, hypertension, and diabetes
were found to correlate with storage symptoms on multiple logistic
regression (Table 3). Such observations conform to the findings
by Ng et al,17 who noticed that in
their cohort of 617 men with LUTS, 43% had hypertension and 29% had
dysglycaemia. In addition, Ng et al17
also reported that patients with moderate-to-severe LUTS had a
significantly higher chance of having at least one cardiovascular risk
factor during assessment. These results are echoed in an updated and more
detailed analysis of 966 men with LUTS.18
Yee et al18 demonstrated that the
severity of LUTS was significantly positively correlated with Framingham
score, which is an estimate of the risk of coronary heart disease taking
into account of age, sex, smoking status, cholesterol levels, blood
pressure, and hypertensive treatments. This supports the hypothesis that
atherosclerosis leads to pelvis and bladder ischaemia, and that this might
be one of the mechanisms leading to LUTS.19
Studies on the effect of caffeinated drinks on LUTS
are scarce, and most have been on urinary incontinence. Davis et al20 reported that caffeine consumption was significantly
associated with moderate-to-severe urinary incontinence in men from the US
National Health and Nutrition Examination Survey. A similar finding was
reported by Baek et al21 from the
Korean National Health and Nutritional Examination Survey among
postmenopausal women. However, our study did not find such a correlation.
On the contrary, the consumption of caffeinated drink correlates
negatively with storage symptoms in general (Table 3). One possible explanation for this
contradiction is that respondents with significant storage symptoms had
usually already cut down their caffeine intake. Thus, our survey could not
illustrate the true impact of caffeinated drinks on overactive bladder
symptoms. In addition to beverage consumption habits, a lower education
level was another factor we found correlating with storage and voiding
symptoms (Table 3). Another study proposed that knowledge on
health and disease perception, which might be a function of education
level, would lower the perceived severity of LUTS.22
In a prospective cohort of elderly men, Chung et al23 showed that the presence of
moderate-to-severe LUTS at baseline was significantly associated with
increased risk for being depressed at 2-year follow-up. The current study
found that, individually, storage symptoms and voiding symptoms were
correlated with a higher PHQ score, translating into a higher risk of
depression. Furthermore, both storage and voiding symptoms were negatively
correlated with all components of general health as measured by SF-12v2.
These findings highlight the importance of LUTS management, considering
its prevalence and its effect on individual well-being.
A significant percentage of respondents with LUTS
did not seek medical help. A similar result has been observed in other
Southeast Asian countries.1
Possible reasons for a low rate of medical help seeking behaviour include
social stigma or a common belief that LUTS is unavoidable with ageing. A
multinational cross-sectional survey on men seeking medical help for LUTS
found that nocturia was the most common symptom among these patients
(88%).24 Our study demonstrated
that, not only was nocturia a common symptom which drove respondents to
seek medical help, it was also the most bothering symptom with the highest
symptom score (Table 4). This suggests that nocturia is one of the
most important symptoms that drive patients to seek medical help. However,
management of nocturia is still a challenge for urologists. Cutting fluid
intake alone was not found to be useful in prolonging the duration between
the time retiring to bed and the first nocturia episode.25 Antidiuretics are presently the only treatment that
provide consistent response in the setting of nocturnal polyuria.26
Limitations of the present study include the bias
from self-reports to measure LUTS, which might be prone to inaccuracy when
compared with physician assessment. However, a meticulous physical
examination would not be possible in the setting of a large-scale
epidemiological study. The telephone interview cam eliminate the
limitation of illiteracy that might be present in self-administered
questionnaires; however, such interviews might introduce bias from each
interviewer’s technique, as well as time pressure on respondents. The
interviewers in our study were professional interviewers with vast
experience in medical research. This minimised potential interview bias.
This population-based survey confirms that LUTS is
common among both men and women. Symptoms increase with age, significantly
affecting patient mental and general health. Storage symptoms are more
prominent than voiding symptoms, with nocturia being the most bothering
symptom. A significant percentage of respondents with LUTS did not seek
medical help. Future research and investigation should address this
deficit.
Author contributions
All authors have made substantial contributions to
the concept or design of this study; acquisition of data; analysis or
interpretation of data; drafting of the manuscript; and critical revision for
important intellectual content. All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of interest
The authors have no conflicts of interest to
disclose.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was obtained from the Joint Chinese
University of Hong Kong-New Territories East Cluster Clinical Research
Ethics Committee (Ref. CRE-2016.588).
References
1. Chapple C, Castro-Diaz D, Chuang YC, et
al. Prevalence of lower urinary tract symptoms in China, Taiwan, and South
Korea: results from a cross-sectional, population-based study. Adv Ther
2017;34:1953-65. Crossref
2. Hutchison A, Farmer R, Chapple C, et al.
Characteristics of patients presenting with LUTS/BPH in six European
countries. Eur Urol 2006;50:555-61. Crossref
3. Sagnier PP, MacFarlane G, Teillac P,
Botto H, Richard F, Boyle P. Impact of symptoms of prostatism on level of
bother and quality of life of men in the French community. J Urol
1995;153(3 Pt 1):669-73. Crossref
4. Botelho EM, Elstad EA, Taubenberger SP,
Tennstedt SL. Moderating perceptions of bother reports by individuals
experiencing lower urinary tract symptoms. Qual Health Res
2011;21:1229-38. Crossref
5. Wong SY, Hong A, Leung J, Kwok T, Leung
PC, Woo J. Lower urinary tract symptoms and depressive symptoms in elderly
men. J Affect Disord 2006;96:83-8. Crossref
6. Census and Statistics Department, Hong
Kong SAR Government. Available from: https://www.censtatd.gov.hk/home/.
Accessed Nov 2016.
7. Homma Y, Yoshida M, Seki N, et al.
Symptom assessment tool for overactive bladder syndrome—overactive bladder
symptom score. Urology 2006;68:318-23. Crossref
8. Kroenke K, Spitzer RL, Williams JB. The
PHQ-9: validity of a brief depression severity measure. J Gen Intern Med
2001;16:606-13. Crossref
9. Rosen RC, Riley A, Wagner G, Osterloh
IH, Kirkpatrick J, Mishra A. The international index of erectile function
(IIEF): a multidimensional scale for assessment of erectile dysfunction.
Urology 1997;49:822-30. Crossref
10. Abrams P, Cardozo L, Fall M, et al.
The standardisation of terminology in lower urinary tract function: report
from the standardisation sub-committee of the International Continence
Society. Urology 2003;61:37-49. Crossref
11. Coyne KS, Sexton CC, Thompson CL, et
al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the
UK and Sweden: results from the Epidemiology of LUTS (EpiLUTS) study. BJU
Int 2009;104:352-60. Crossref
12. Irwin DE, Milsom I, Hunskaar S, et al.
Population-based survey of urinary incontinence, overactive bladder, and
other lower urinary tract symptoms in five countries: results of the EPIC
study. Eur Urol 2006;50:1306-14. Crossref
13. Kobayashi M, Nukui A, Kamai T.
Seasonal changes in lower urinary tract symptoms in Japanese men with
benign prostatic hyperplasia treated with α1-blockers. Int
Neurourol J 2017;21:197-203. Crossref
14. Choi HC, Kwon JK, Lee JY, Han JH, Jung
HD, Cho KS. Seasonal variation of urinary symptoms in Korean men with
lower urinary tract symptoms and benign prostatic hyperplasia. World J
Mens Health 2015;33:81-7. Crossref
15. Milsom I, Abrams P, Cardozo L, Roberts
RG, Thüroff J, Wein AJ. How widespread are the symptoms of an overactive
bladder and how are they managed? A population-based prevalence study. BJU
Int 2001;87:760-6. Crossref
16. Stewart WF, Van Rooyen JB, Cundiff GW,
et al. Prevalence and burden of overactive bladder in the United States.
World J Urol 2003;20:327-36.
17. Ng CF, Wong A, Li ML, Chan SY, Mak SK,
Wong WS. The prevalence of cardiovascular risk factors in male patients
who have lower urinary tract symptoms. Hong Kong Med J 2007;13:421-6.
18. Yee CH, Yip JS, Cheng NM, et al. The
cardiovascular risk factors in men with lower urinary tract symptoms.
World J Urol 2018 Aug 6. Epub ahead of print. Crossref
19. McVary K. Lower urinary tract symptoms
and sexual dysfunction: epidemiology and pathophysiology. BJU Int 2006;97
Suppl 2:23-8. Crossref
20. Davis NJ, Vaughan CP, Johnson TM 2nd,
et al. Caffeine intake and its association with urinary incontinence in
United States men: results from National Health and Nutrition Examination
Surveys 2005-2006 and 2007-2008. J Urol 2013;189:2170-4. Crossref
21. Baek JM, Song JY, Lee SJ, et al.
Caffeine intake is associated with urinary incontinence in Korean
postmenopausal women: results from the Korean National Health and
Nutrition Examination Survey. PLoS One 2016;11:e0149311. Crossref
22. Yee CH, Li JK, Lam HC, Chan ES, Hou
SS, Ng CF. The prevalence of lower urinary tract symptoms in a Chinese
population, and the correlation with uroflowmetry and disease perception.
Int Urol Nephrol 2014;46:703-10. Crossref
23. Chung RY, Leung JC, Chan DC, Woo J,
Wong CK, Wong SY. Lower urinary tract symptoms (LUTS) as a risk factor for
depressive symptoms in elderly men: results from a large prospective study
in Southern Chinese men. PLoS One 2013;8:e76017. Crossref
24. Ho LY, Chu PS, Consigliere DT, et al.
Symptom prevalence, bother, and treatment satisfaction in men with lower
urinary tract symptoms in Southeast Asia: a multinational, cross-sectional
survey. World J Urol 2018;36:79-86. Crossref
25. Teoh JY, Chan C, Ng CA, et al.
Desmopressin oral lyophilisate lessens the burden of nocturia in the
post-TURP men sooner they go asleep—an action unreachable by fluid
restriction alone but attenuated by aging. International Continence
Society 2017 Florence. Available from:
https://www.ics.org/2017/abstract/626. Accessed 11 Mar 2018.
26. Sakalis VI, Karavitakis M,
Bedretdinova D, et al. Medical treatment of nocturia in men with lower
urinary tract symptoms: systematic review by the European Association of
Urology Guidelines Panel for male lower urinary tract symptoms. Eur Urol
2017;72:757-69. Crossref