DOI: 10.12809/hkmj154810
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Endovascular treatment of erectile dysfunction due to
internal iliac artery atherosclerotic disease
Bryan P Yan, MB, BS, FRACP
Department of Medicine and Therapeutics, The
Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr Bryan P Yan (bryan.yan@cuhk.edu.hk)
Introduction
Erectile dysfunction (ED) is defined as the
recurrent inability to achieve and maintain an erection satisfactory for
sexual intercourse. Worldwide, ED affects approximately 300 million men,
and nearly 30% of men between age 40 and 70 years.1 Current pharmacological options for treatment of ED are
limited, with up to 50% of patients experiencing suboptimal response to
oral phosphodiesterase inhibitor (PDE5i).2
Atherosclerotic occlusive disease of the ilio-pudendal-penile arteries
resulting in arterial insufficiency to the penis has been reported to
affect up to 75% of patients with ED.3
In a recent study of 30 diabetic patients with ED and coronary artery
disease, significant internal iliac artery (IIA) and internal pudendal
artery (IPA) disease was found 20% and 36.7% of patients, respectively.4 Atherosclerotic occlusive disease
may result in arterial insufficiency to the penis, limiting the inflow of
blood required to fill the corpora cavernosa to achieve penile erection.
This report describes the case of a patient with ED caused by
atherosclerotic disease of the left IIA that was successfully treated by
endovascular revascularisation.
Case presentation
A 71-year-old man presented to our hospital with
recurrent claudication and severe erectile dysfunction (ED). The patient
had a history of insulin-requiring type 2 diabetes mellitus, hypertension,
hyperlipidaemia, renal transplant for end-stage renal failure due to
obstructive nephropathy, advanced coronary and peripheral artery disease
status after multiple interventions. The patient had been diagnosed with
ED more than 10 years previously. His ED responded initially to oral
phosphodiesterase inhibitor (PDE5i) therapy. In the 12 months prior to the
present case, the patient’s ED deteriorated and became refractory to PDE5i
therapy. This caused significant distress and loss of quality of life
because the patient wished to remain sexually active.
Peripheral angiography of the ilio-pudendal-penile
arteries was performed opportunistically at time of endovascular
intervention for recurrent lower limb claudication in September 2015. The
peripheral angiography revealed total occlusion of the right IIA and
haemodynamically significant stenoses in the left common and distal IIA
with a significant pressure gradient of 20 mm Hg across the lesions (Fig
1). The penile artery and left IPA were supplied by the diseased
left IIA. Elective endovascular intervention was performed via a 45-cm
6-Fr sheath inserted in the right common femoral artery and advanced over
the aortic bifurcation to the left IIA. The IIA stenosis was dilated with
a 4- × 40-mm balloon (Sterling; Boston Scientific, Marlborough [MA],
United States) followed by a 5- × 40-mm paclitaxel-eluting balloon
(Ranger; Boston Scientific) aiming to lower the risk of restenosis. The
ostium of the left internal IIA was dilated with a 6- × 40-mm scoring
balloon (Angiosculpt; AngioScore, Fremont [CA], United States) and the
left common IIA was dilated with an 8- × 20-mm balloon (Sterling; Boston
Scientific). Excellent angiographic results were achieved with elimination
of the translesional gradient (Fig 2). There were no complications, and the patient
was discharged the following day.
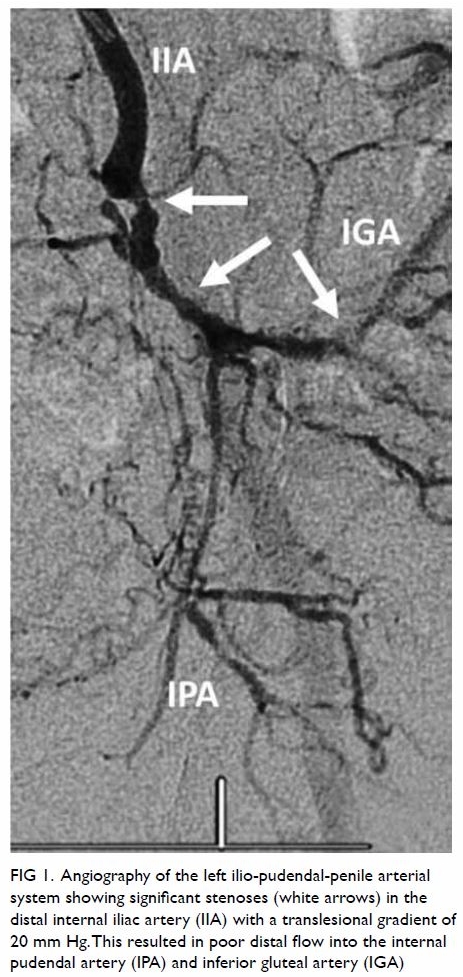
Figure 1. Angiography of the left ilio-pudendal-penile arterial system showing significant stenoses (white arrows) in the distal internal iliac artery (IIA) with a translesional gradient of 20 mm Hg. This resulted in poor distal flow into the internal pudendal artery (IPA) and inferior gluteal artery (IGA)

Figure 2. Excellent angiographic results post-angioplasty of the left internal iliac artery (IIA) using a drug-eluting balloon with resolution of translesional gradient. This resulted in improved distal flow into the internal pudendal artery (IPA) and inferior gluteal artery (IGA)
The patient reported significant improvement in
erectile function at the 3-month follow-up visit. His erectile hardness
score improved from 1 (the penis is larger than normal but not hard) to 3
(the penis is hard enough for penetration but not completely hard). Of the
domains assessed by the international index of erectile function score:
(i) erectile function improved from severe (score 1 out of 30) to moderate
dysfunction (score 9); (ii) orgasmic function from severe (score 0 out of
10) to mild-to-moderate dysfunction (score 6); (iii) intercourse
satisfaction from severe (score 0 out of 15) to moderate dysfunction
(score 4), and (iv) overall satisfaction from moderate (score 4 out of 10)
to mild dysfunction (score 8).
Discussion
With the advancement of endovascular techniques and
technologies, revascularisation of the small-calibre penile artery
(average 1-2 mm) and IPA (2-3 mm) has been shown to be safe, feasible, and
associated with significant improvement in erectile function in selected
ED patients with penile arterial insufficiency.5
6 In a study of 30 patients with ED
and suboptimal response to PDE5i, percutaneous revascularisation of the
IPA using coronary drug-eluting stents was associated with clinically
meaningful improvement in ED.5
Another recently published study on pelvic revascularisation investigated
20 patients with arteriogenic ED.6
After balloon angioplasty for isolated penile artery stenosis, 60% of
those patients demonstrated significant improvement in ED at 6 months.6 Drug-eluting balloons have been shown to be superior to
plain balloon angioplasty in the treatment of infrainguinal peripheral
arterial disease. However, the use of drug-eluting balloons in the IIA is
an off-label indication and should be considered investigational.
In summary, endovascular treatment of
ilio-pudendal-penile arterial disease may offer significant benefits in
patients with ED associated with arterial insufficiency that is refractory
to medical therapy. However, it is important to emphasise that there are
many causes of ED and atherosclerotic disease of erectile-related arteries
is only one of them. Close collaboration with a urologist and exclusion of
other aetiologies of ED prior to angiography is critical in patient
selection and successful outcome.
Author contributions
As an editor of the journal, BP Yan was not
involved in the peer review process of the article. BP Yan contributed to
performance of the procedure, drafting of the article, and critical
revision of the content.
Declaration
The author has disclosed no conflicts of interest.
The author had full access to the data, contributed to the study, approved
the final version for publication, and takes responsibility for its
accuracy and integrity.
References
1. NIH Consensus Conference. Impotence. NIH
Consensus Development Panel on Impotence. JAMA 1993;270:83-90. Crossref
2. Hatzimouratidis K, Hatzichristou DG. A
comparative review of the options for treatment of erectile dysfunction:
which treatment for which patient? Drugs 2005;65:1621-50. Crossref
3. Philip F, Shishehbor MH, Desai MY,
Schoenhagen P, Ellis S, Kapadia SR. Characterization of internal pudendal
artery atherosclerosis using aortography and multi-detector computed
angiography. Catheter Cardiovasc Interv 2013;82:E516-21. Crossref
4. Zaki H, Nammas W, Shawky A, Mortada A,
Zaki T. Prevalence of internal pudendal artery disease in diabetic
patients with erectile dysfunction and angiographically documented
multi-vessel coronary artery disease. Egypt Heart J 2013;65:87-91. Crossref
5. Rogers JH, Goldstein I, Kandzari DE, et
al. Zotarolimus-eluting peripheral stents for the treatment of erectile
dysfunction in subjects with suboptimal response to phosphodiesterase-5
inhibitors. J Am Coll Cardiol 2012;60:2618-27. Crossref
6. Wang TD, Lee WJ, Yang SC, et al. Safety
and six-month durability of angioplasty for isolated penile artery
stenoses in patients with erectile dysfunction: a first-in-man study.
EuroIntervention 2014;10:147-56. Crossref

