DOI: 10.12809/hkmj177024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE CME
Medication overuse headache: strategies for prevention
and treatment using a multidisciplinary approach
M van Driel, MD, PhD1; E Anderson, MSc,
PhD2; T McGuire, BPharm, PhD3,4,5; R Stark, MB, BS,
FRACP6
1 Faculty of Medicine, University of
Queensland, Brisbane, Queensland, Australia
2 In Vivo Academy Ltd, In Vivo
Communications, Sydney, New South Wales, Australia
3 Faculty of Health Sciences and
Medicine, Bond University, Gold Coast, Queensland, Australia
4 School of Pharmacy, The University of
Queensland, Brisbane, Queensland, Australia
5 Mater Pharmacy Services, Mater Health
Services, South Brisbane, Queensland, Australia
6 Neurology Department, Alfred Hospital,
Melbourne, Victoria, Australia
Corresponding author: Prof M van Driel (m.vandriel@uq.edu.au)
Abstract
Medication overuse headache, which affects
patients who have migraines and frequent headaches, is prevalent
worldwide and can severely impact daily functioning. Medication overuse
headache is often not recognised by primary care physicians or general
practitioners, as patients may overuse medications that are freely
available without a prescription. Overuse of codeine-containing
analgesics is particularly problematic and contributes to ongoing
morbidity and opioid-related mortality. This article aims to provide an
overview of the detection, prevention, and management of medication
overuse headache. The definition of medication overuse headache and the
risk levels of commonly used symptomatic headache medications are
presented. An algorithm consisting of a number of simple questions can
assist general practitioners with identifying at-risk patients.
Treatment strategies are discussed in the context of a multidisciplinary
approach.
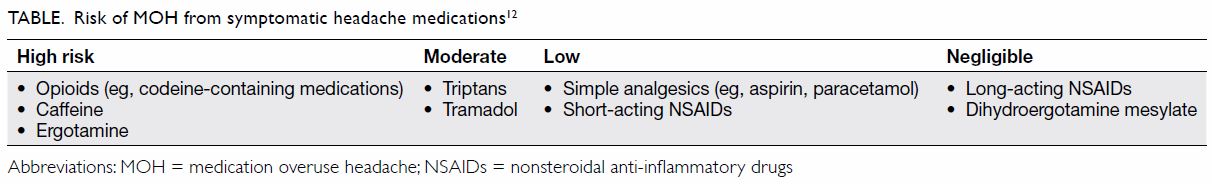
The estimated prevalence of medication overuse
headache (MOH) in the general population ranges from 0.6% to 7%.1 2 3 4 5 6 7 8 A number of
acute headache treatments may cause MOH,7
and the medications that are predominantly associated with MOH vary from
country to country.1 7 9 10 Opioids such as codeine are particularly problematic,
as they are consistently associated with increasingly severe headaches11 (Table12) and
poor outcomes after withdrawal.13
In a number of regions, including Hong Kong and Japan, codeine-containing
medication is only available by prescription.14
In Australia, beginning in 2018, codeine (and its combinations with simple
analgesics) will only be available by prescription, following a 2015
decision by the Australian Therapeutic Goods Administration (TGA).15 This policy change is supported by evidence
demonstrating an increase in unintentional codeine-related deaths in
Australia.16
A systematic analysis of the global, regional, and
national burden of neurological disorders from 1990 to 2015 (using data
from the Global Burden of Disease Study 2015) found that neurological
disorders were the leading cause of disability-adjusted life years (DALYs)
in 2015, with the most prevalent neurological disorders being tension-type
headache (1505.9 million DALYs), migraine (958.8 million DALYs), and MOH
(58.5 million DALYs).17 As large
numbers of people are potentially at risk of MOH, including anyone with
frequent primary episodic headaches, strategies for primary prevention,
treatment, and prevention of relapse may have substantial public health
benefits.
Definition of medication overuse headache
The definition of MOH is headache occurring on ≥15
days per month as a consequence of regular overuse of acute or symptomatic
headache medication (≥10 days per month for triptans, ergotamines, or
opioids; ≥15 days per month for simple or combined analgesics) for more
than 3 months. It usually, but not invariably, resolves after the overuse
is stopped.18
Problems with detection and treatment of medication
overuse headache
Patients’ lack of awareness of medication overuse
as a cause of headaches, reluctance to acknowledge how much medication
they take, and poor adherence to recommended treatment have been
identified as barriers to detection and management of MOH. A survey of
Australian general practitioners (GPs)19
showed that GPs’ awareness of MOH is low, although the awareness of
codeine overuse in general may have increased following the TGA’s
decision, which was widely discussed in the media. In Singapore, a general
practice survey of patients and their attending physicians in a primary
care setting found that 22.6% of the patient population reported taking
acute pain medication for headaches at least 4 days per week. However, the
physicians only identified this in 5.3% of the study population,
indicating that physicians did not recognise a large percentage of
patients at risk of MOH.20 Khu et
al20 commented that overuse of
analgesic medications may lead to ‘doctor-hopping’ by patients in search
of increasingly elusive headache relief. There may be a need to provide
greater awareness of MOH during medical training, as a survey of final
year medical students in Singapore found that 47% were unfamiliar with MOH
as a disease entity, and 96% were unfamiliar with local clinical practice
guidelines about headaches.21
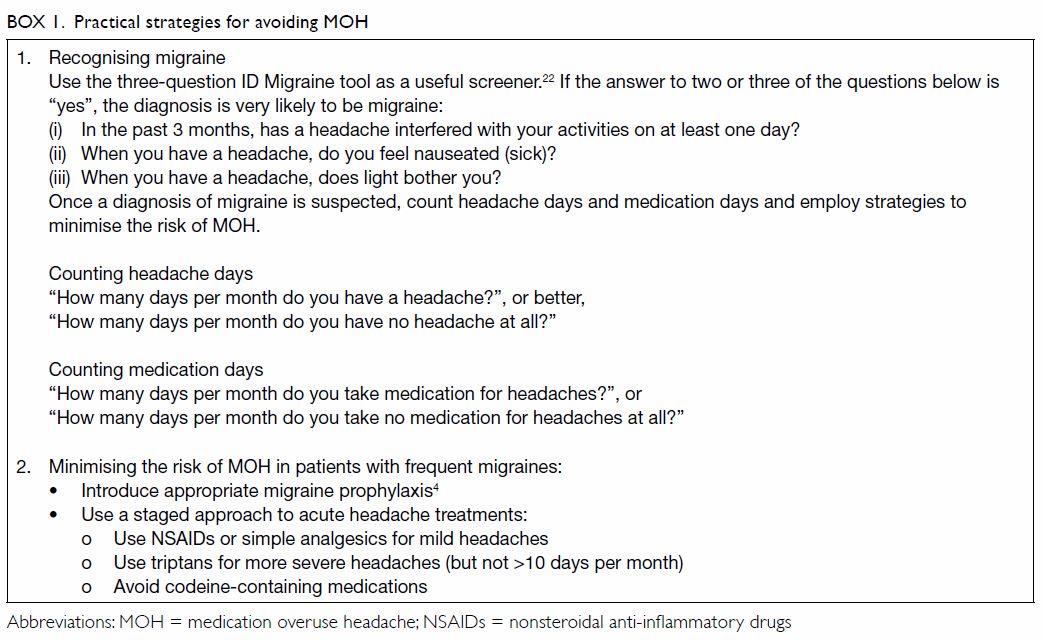
Patients with frequent episodic migraines
(headaches on 8-15 days per month) or chronic migraines (headaches on
>15 days per month) are at particular risk of developing MOH. General
practitioners play a crucial role in identifying these patients, assessing
their medication intake, and offering strategies to minimise the risk of
MOH (Box 14 22).
Patients may be reluctant to reveal how many
analgesics they take or may be unaware or unwilling to accept that the
medication they use to treat their headaches is actually contributing to
the continuation of their headaches. They may also be reluctant to
discontinue medication that they have found to provide some relief for
their headaches in the past. Patients who are anxious about their
headaches interfering with essential activities, such as work, may use
medication routinely as a preventive measure. In addition, a common
misperception among consumers is that medication that can be purchased
without a prescription (‘over the counter’) is harmless.23 Unfortunately, once established, MOH (particularly
that caused by opioids) has a high relapse rate after treatment.24 Adherence to recommended treatment is generally
suboptimal in patients with MOH, but the majority of relapses occur in the
first year after withdrawal.25 It
is therefore important to educate patients about the pathophysiology and
treatment of MOH and to continue supporting them beyond the immediate
period of withdrawal.
Some patients who report “excessive” medication use
and very frequent headache do not respond to medication withdrawal.
Patients who develop MOH are usually those with intrinsically
high-frequency headaches, and withdrawal tends to lead to reversion to
their natural background headache pattern, which may range from infrequent
episodic migraines to higher-frequency patterns. Scher et al26 questioned the benefit of withdrawal or restriction
of medication on the grounds that the patient may not benefit from it.
However, withdrawal allows the underlying headache pattern to be
determined and a reappraisal of headache control to be conducted. Study
results have demonstrated that withdrawal of headache medication benefits
many patients with MOH. For example, in a recent study, patients diagnosed
with MOH were randomised to 2 months’ detoxification with either complete
withdrawal of medication or acute medication restricted to 2 days/week.
The number of migraine-days/ month was significantly reduced after 6
months with both treatments, with a greater reduction of
migraine-days/month in the complete withdrawal group, indicating that
complete withdrawal is generally more effective than medication
restriction and that medication overuse was a major factor in the
patients’ headache pathology.27
A multidisciplinary approach
As patients with MOH often do not present to their
GPs in response to the first instance, pharmacists can play a role in
educating patients who self-medicate with analgesics when analgesics are
purchased without a prescription.28
They could encourage patients who may be overusing pain relief medication
to consult their GPs to discuss other treatment options. However, it may
not be easy to identify at-risk patients, as some obtain large quantities
of headache medications by shopping at different pharmacies.
Identification of these patients could be facilitated by using a tracking
system to detect patients who buy headache medication at multiple
pharmacies.
Conditions associated with self-medication, such as
MOH, could be prevented by community pharmacists. Community pharmacists
have overviews of both prescriptions and non-prescription medications that
patients are taking (provided that patients are not visiting several
different pharmacies) and are easily accessible to patients.29 30 Thus, the
sale of headache medications is an opportunity to discuss their potential
adverse effects and their role in MOH. A survey in Japan on the role of
community pharmacists in self-medication of patients with headache found
that 32% of the surveyed doctors were concerned about the increase of
patients who overuse headache medication. Both doctors and pharmacists
thought that pharmacists should not only provide patients with
“instruction on the use of drugs” but also suggest “when to consult a
hospital or clinic”.31 However,
strategies may need to be devised to motivate patients to do this, as
another Japanese survey of pharmacists and doctors found that 22% of
pharmacists had experienced refusal by patients with headache to consult a
clinic, despite the pharmacist’s recommendation.32
Community pharmacists have an important role in
supporting patients with headache. This can be fostered by all key
stakeholders—pharmacists, doctors, and patients—being provided with
multidisciplinary opportunities to improve their MOH health literacy and
to maintain an open and collaborative relationship.
Although MOH often develops outside of GPs’
immediate view through patients’ self-medication, GPs are important in its
prevention, detection, and treatment. The first step is educating
patients, and when they do not understand the cause of and treatment for
MOH, taking time to inform them and clarify their misunderstandings.29 The next step is to develop a plan with the patient
and provide clear and continuing support for what is often a challenging
journey. General practitioners also need to be aware of situations in
which patients should be referred to a neurologist, preferably one who
specialises in headache management.
Discussions between GPs or pharmacists and patients
who overuse headache medication are often delicate. The patient may
perceive an accusation of ‘recreational use’ of (particularly
codeine-containing) drugs. It is vital for productive communication that
the health care professional clarify that there is no suspicion of this
type and that the medications are recognised as being used to deal with
genuinely troublesome symptoms. It is vital to subsequently emphasise that
ongoing use of particular headache medications may contribute to
perpetuation of headaches and that better strategies are available.
Management and prevention strategies
Prevention of headaches is better than curing them.
Pharmacists and GPs who are aware of MOH can detect patients with
increasing frequencies of headaches and medication use. Strategies to
assist such patients before they progress into frank MOH include lifestyle
adjustments and appropriate prophylaxis, as discussed below as part of MOH
treatment (Box 2).
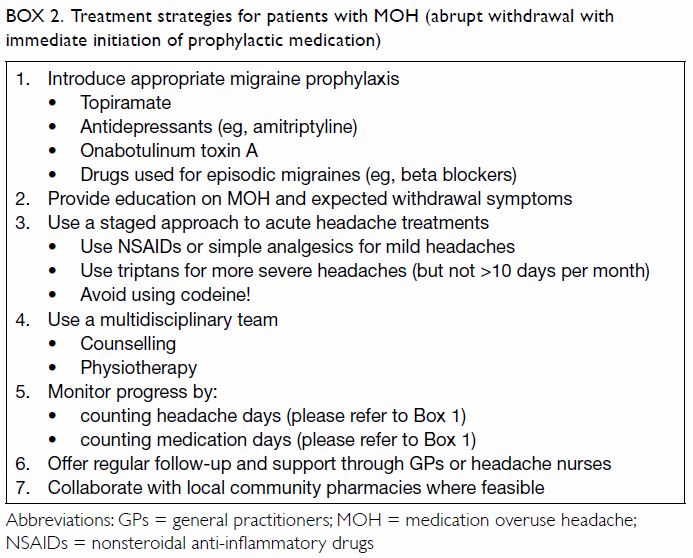
Box 2. Treatment strategies for patients with MOH (abrupt withdrawal with immediate initiation of prophylactic medication)
Complete withdrawal from overused headache
medications is a key component of the management strategy, along with
education, counselling, and support. Abrupt withdrawal is usually
preferred, but tapered withdrawal may be more appropriate when codeine is
implicated.25 Coexisting
psychiatric conditions should also be assessed and managed. As medication
discontinuation results in withdrawal headaches—often associated with
nausea, vomiting, and sleep disturbance—patients frequently need
assistance coping with withdrawal symptoms and persevering with
discontinuation.4 12 33 34 Symptoms usually last between 2 and 10 days, with
withdrawal from triptans lasting approximately 4 days and that from
nonsteroidal anti-inflammatory drugs lasting about 10 days. Withdrawal can
be managed through primary care; however, opioid discontinuation may
require hospitalisation.34 35
Accurate diagnosis based on the third edition of
the International Classification of Headache Disorders17 and referral of complex cases to a
neurologist/headache specialist is recommended for individualised
treatments. Psychiatric assessment may also be indicated in some cases.
However, in many countries, limited specialist availability means that
referrals need to be selective. Psychologists and physical therapists have
a role, as psychotherapy, relaxation techniques, physical exercise, and
cognitive behaviour therapy may be useful adjuncts to supervised
pharmacotherapy.4 12 23 28 34 36 37 The
combination of behavioural treatment and prophylactic medication may
significantly reduce the risk of relapse.37
Preventive medications for chronic migraines include antiepileptic drugs
(particularly topiramate), antidepressants (eg, amitriptyline),
onabotulinum toxin A, and drugs used for episodic migraines (eg, beta
blockers). For example, topiramate (oral) and onabotulinum toxin A (by
local injection) are recommended by the Taiwan Headache Society 2017
medical treatment guidelines as first-line treatments for prophylaxis of
chronic migraines.38 Education
about acute and prophylactic treatment may improve adherence to both
pharmacological and non-pharmacological therapies.28
In some circumstances, withdrawal may require
hospital admission. Patients with MOH who have been detoxified as
in-patients should be followed up by their GPs. Support by a headache
nurse (available in some neurological practices) can improve adherence to
detoxification.39
Multidisciplinary treatment of patients with MOH,
including pharmacological prophylaxis, relaxation therapy, and aerobic
sports, is associated with reduction in headaches, as long as patients
adhere to the recommended therapies.28
Motivational telephone interviewing may also help to promote adherence.40 To supplement regular GP
support, practice nurses could be involved in patient support, and they
could liaise with pharmacists to monitor medication use.
Conclusion
There is an urgent need for increased awareness of
MOH among both patients and health care professionals.41 Medication overuse headache causes considerable
morbidity but is preventable. Headache frequency (and the associated
disability, depression, and anxiety) can be considerably reduced in
patients with MOH through withdrawal from the overused medication and
appropriate supportive treatment. A multidisciplinary approach involving
primary care physicians (GPs), community pharmacists, nurses, and allied
health providers,36 with referral
to neurologists/headache specialists (where available) for complex cases,
is recommended.
Author contributions
All authors contributed to the concept of the
paper, acquisition and interpretation of data and critical revision of the
manuscript for important intellectual content. EA and MVD drafted the
article. All authors approved the final version.
Declaration
M van Driel, T McGuire, and R Stark have received
consulting fees from In Vivo Academy Ltd for development of education
materials for a multidisciplinary programme about MOH. In Vivo Academy Ltd
received an unrestricted educational grant from Pfizer to develop
educational material about MOH. R Stark has also received lecture and/or
consulting fees from Allergan, Novartis, TEVA, MSD, Abbvie and SciGen
(Australia) and from In Vivo Academy Ltd relating to a Pfizer-sponsored
project, and has undertaken clinical trials for Allergan. E Anderson is an
employee of In Vivo Academy Ltd.
References
1. Cha MJ, Moon HS, Sohn JH, et al. Chronic
daily headache and medication overuse headache in first-visit headache
patients in Korea: a multicenter clinic-based study. J Clin Neurol
2016;12:316-22. Crossref
2. Cheung V, Amoozegar F, Dilli E.
Medication overuse headache. Curr Neurol Neurosci Rep 2015;15:509. Crossref
3. Herekar AA, Ahmad A, Uqaili UL, et al.
Primary headache disorders in the adult general population of Pakistan—a
cross sectional nationwide prevalence survey. J Headache Pain 2017;18:28.
Crossref
4. Kristoffersen ES, Lundqvist C.
Medication-overuse headache: epidemiology, diagnosis and treatment. Ther
Adv Drug Saf 2014;5:87-99. Crossref
5. Steiner TJ, Stovner LJ, Katsarava Z, et
al. The impact of headache in Europe: principal results of the Eurolight
project. J Headache Pain 2014;15:31. Crossref
6. Yu S, Liu R, Zhao G, et al. The
prevalence and burden of primary headaches in China: a population-based
door-to-door survey. Headache 2012;52:582-91. Crossref
7. Westergaard ML, Munksgaard SB, Bendtsen
L, Jensen RH. Medication-overuse headache: a perspective review. Ther Adv
Drug Saf 2016;7:147-58. Crossref
8. Zebenholzer K, Andree C, Lechner A, et
al. Prevalence, management and burden of episodic and chronic headaches—a
cross-sectional multicentre study in eight Austrian headache centres. J
Headache Pain 2015;16:531. Crossref
9. Dong Z, Chen X, Steiner TJ, et al.
Medication-overuse headache in China: clinical profile, and an evaluation
of the ICHD-3 beta diagnostic criteria. Cephalalgia 2015;35:644-51. Crossref
10. Manandhar K, Risal A, Steiner TJ,
Holen A, Linde M. The prevalence of primary headache disorders in Nepal: a
nationwide population-based study. J Headache Pain 2015;16:95. Crossref
11. Johnson JL, Hutchinson MR, Williams
DB, Rolan P. Medication-overuse headache and opioid-induced hyperalgesia:
A review of mechanisms, a neuroimmune hypothesis and a novel approach to
treatment. Cephalalgia 2013;33:52-64. Crossref
12. Smith TR, Stoneman J. Medication
overuse headache from antimigraine therapy: clinical features,
pathogenesis and management. Drugs 2004;64:2503-14. Crossref
13. Bøe MG, Salvesen R, Mygland A. Chronic
daily headache with medication overuse: predictors of outcome 1 year after
withdrawal therapy. Eur J Neurol 2009;16:705-12. Crossref
14. Butler J. You won’t be able to buy
codeine over the counter anymore. Huffington Post 2016 Dec 20. Available
from:
http://www.huffingtonpost.com.au/2016/12/19/you-wont-be-able-to-buy-codeine-over-the-counteranymore_a_21631170/.
Accessed 25 Oct 2018.
15. Therapeutic Goods Administration,
Department of Health, Australian Government. Proposal for the
re-scheduling of codeine products. 2015. Available from:
https://www.tga.gov.au/media-release/proposal-re-scheduling-codeineproducts.
Accessed 2 Mar 2017.
16. Roxburgh A, Hall WD, Burns L, et al.
Trends and characteristics of accidental and intentional codeine overdose
deaths in Australia. Med J Aust 2015;203:299. Crossref
17. GBD 2015 Neurological Disorders
Collaborator Group. Global, regional, and national burden of neurological
disorders during 1990-2015: a systematic analysis for the Global Burden of
Disease Study 2015. Lancet Neurol 2017;16:877-97. Crossref
18. Headache Classification Committee of
the International Headache Society. The International Classification of
Headache Disorders, 3rd edition (beta version). Cephalalgia
2013;33:629-808. Crossref
19. van Driel ML, McGuire TM, Stark R,
Lazure P, Garcia T, Sullivan L. Learnings and challenges to deploy an
interprofessional and independent medical education programme to a new
audience. J Eur CME 2017;6:1400857. Crossref
20. Khu JV, Siow HC, Ho KH. Headache
diagnosis, management and morbidity in the Singapore primary care setting:
findings from a general practice survey. Singapore Med J 2008;49:774-9.
21. Ong JJ, Chan YC. Medical undergraduate
survey on headache education in Singapore: knowledge, perceptions, and
assessment of unmet needs. Headache 2017;57:967-78. Crossref
22. Lipton RB, Dodick D, Sadovsky R, et
al. A self-administered screener for migraine in primary care: The ID
MigraineTM validation study. Neurology 2003;61:375-82. Crossref
23. Frich JC, Kristoffersen ES, Lundqvist
C. GPs’ experiences with brief intervention for medication-overuse
headache: a qualitative study in general practice. Br J Gen Pract
2014;64:e525-31. Crossref
24. Katsarava Z, Muessig M, Dzagnidze A,
Fritsche G, Diener HC, Limmroth V. Medication overuse headache: rates and
predictors for relapse in a 4-year prospective study. Cephalalgia
2005;25:12-5. Crossref
25. Evers S, Marziniak M. Clinical
features, pathophysiology, and treatment of medication-overuse headache.
Lancet Neurol 2010;9:391-401. Crossref
26. Scher AI, Rizzoli PB, Loder EW.
Medication overuse headache: an entrenched idea in need of scrutiny.
Neurology 2017;89:1296-304. Crossref
27. Carlsen LN, Munksgaard SB, Jensen RH,
Bendtsen L. Complete detoxification is the most effective treatment of
medication-overuse headache: a randomized controlled open-label trial.
Cephalalgia 2018;38:225-36. Crossref
28. Gaul C, Brömstrup J, Fritsche G,
Diener HC, Katsarava Z. Evaluating integrated headache care: a one-year
follow-up observational study in patients treated at the Essen headache
centre. BMC Neurol 2011;11:124. Crossref
29. Giaccone M, Baratta F, Allais G, Brusa
P. Prevention, education and information: the role of the community
pharmacist in the management of headaches. Neurol Sci 2014;35(1
Suppl):1-4. Crossref
30. O’Sullivan EM, Sweeney B, Mitten E,
Ryan C. Headache management in community pharmacies. Ir Med J
2016;109:373.
31. Naito Y, Ishii M, Kawana K, Sakairi Y,
Shimizu S, Kiuchi Y. Role of pharmacists in a community pharmacy for
self-medication of patients with headache [in Japanese]. Yakugaku Zasshi
2009;129:735-40. Crossref
32. Naito Y, Ishii M, Sakairi Y, Kawana K,
Shimizu S, Kiuchi Y. Need for collaboration between community pharmacies
and hospitals or clinics in providing medical treatment for patients with
headache [in Japanese]. Yakugaku Zasshi 2009;129:741-8. Crossref
33. Stark R, Hutton E. Chronic migraine
and other types of chronic daily headache. Medicine Today 2013;14:29-35.
34. Kristoffersen ES, Lundqvist C.
Medication-overuse headache: a review. J Pain Res 2014;26:367-78. Crossref
35. Williams D. Medication overuse
headache. Aust Prescr 2005;28:59-62. Crossref
36. Bendtsen L, Munksgaard S, Tassorelli
C, et al. Disability, anxiety and depression associated with
medication-overuse headache can be considerably reduced by detoxification
and prophylactic treatment. Results from a multicentre, multinational
study (COMOESTAS project). Cephalalgia 2014;34:426-33. Crossref
37. Lake AE 3rd. Medication overuse
headache: biobehavioral issues and solutions. Headache 2006;46(3
Suppl):S88-97. Crossref
38. Huang TC, Lai TH, Taiwan Headache
Society TGSOTHS. Medical treatment guidelines for preventive treatment of
migraine. Acta Neurol Taiwan 2017;26:33-53.
39. Pijpers JA, Louter MA, de Bruin ME, et
al. Detoxification in medication-overuse headache, a retrospective
controlled follow-up study: does care by a headache nurse lead to cure?
Cephalalgia 2016;36:122-30. Crossref
40. Stevens J, Hayes J, Pakalnis A. A
randomized trial of telephone-based motivational interviewing for
adolescent chronic headache with medication overuse. Cephalalgia
2014;34:446-54. Crossref
41. Stark R, McGuire T, van Driel M.
Medication overuse headache in Australia: a call for multidisciplinary
efforts at prevention and treatment. Med J Aust 2016;205:283. Crossref