DOI: 10.12809/hkmj166061
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
En-bloc paediatric dual kidney transplantation in Hong
Kong: a case series and literature review
YS Chan, MB, ChB; MK Yiu, MB, BS, FHKAM (Surgery)
Division of Urology, Department of Surgery, Queen
Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr MK Yiu (yiumk2@ha.org.hk)
Case series
En-bloc paediatric dual kidney transplantation
presents specific challenges but provides a viable option for patients
with end-stage renal disease. In this case series, we report four cases of
paediatric cadaveric en-bloc donor kidney transplantation and review the
literature on reported complications and functional outcomes of this
procedure.
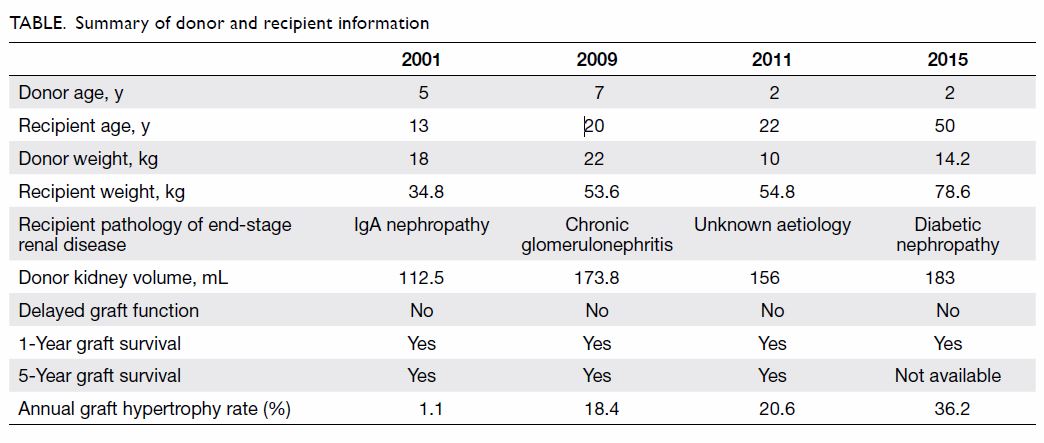
From 2001 to 2015, there were four paediatric
cadaveric en-bloc donor kidney transplantation procedures undertaken in
Hong Kong. Deceased donors’ mean age was 3.6 ± 2.6 years and recipients’
mean age was 26.3 ± 16.3 years. Mean total operating time was 214 ± 28.2
minutes, mean cold ischaemic time was 222 ± 150 minutes, mean warm
ischaemic time was 26 ± 11.3 minutes, and mean graft kidney volume was
156.3 ± 31.3 mL. The Table provides a summary of individual donor and
recipient information.
The kidneys were retrieved en bloc with the donor’s
aorta and vena cava. The proximal end of the aorta and vena cava was
oversewn at the supra-renal level and the ureters were transected as close
to the bladder as possible. Recipients were prepared for extra-peritoneal
implantation with modified Gibson’s incision. The distal ends of the aorta
and vena cava were anastomosed to the recipient’s external iliac artery
and external iliac vein respectively in an end-to-side manner using 5-0
Prolene (Fig). The donor ureters were anastomosed in the
Wallace I manner and neocystoureterostomy was completed with 4-0 Vicryl
according to the Lich-Gregoir technique with a double J stent in each
ureter.1 The two graft kidneys were
placed in the right iliac fossa in the extraperitoneal space created in
routine kidney transplantation surgery. Two drains were placed in the
surgical site.
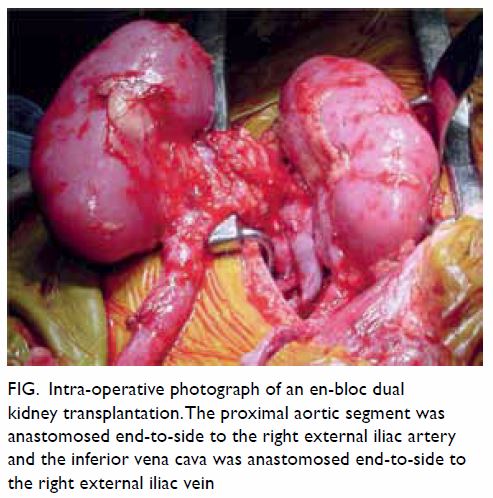
Figure. Intra-operative photograph of an en-bloc dual kidney transplantation. The proximal aortic segment was anastomosed end-to-side to the right external iliac artery and the inferior vena cava was anastomosed end-to-side to the right external iliac vein
Discussion
Historically, paediatric cadaveric kidney en-bloc
donor transplantation was associated with increased early vascular
complications. Furthermore, paediatric en-bloc kidneys need not be
strictly allocated based on recipient weight or age criteria.2
In our series, all patients had good graft function
following transplantation with normal serum creatinine levels and
compensatory hypertrophy of the transplanted dual kidney occurring in all
cases to overcome the size difference between the paediatric and adult
kidney size. Our experience and the functional outcome achieved appear
consistent with the current evidence on dual kidney transplantation in the
literature.
It is well recognised that paediatric kidney
transplantation is difficult, especially when donor kidneys are from
children younger than 6 years of age.3
En-bloc dual kidney transplantation from paediatric donors aims to
increase the nephron mass of the transplanted kidney.
En-bloc dual kidney transplantation is associated
with an increase in the surgical complications rate of up to 16%, of
which, 69% of complications reported were arterial or venous thrombosis.4 In addition, studies have reported
a higher early graft loss in the first postoperative year for paediatric
en-bloc kidney transplantation.5 6 However, Thomusch et al5 reported that long-term graft survival and function
were better in the paediatric dual kidney transplant than from a cadaveric
adult donor.
Early graft failure is commonly caused by vascular
complications. Studies have reported a vascular thrombosis rate of between
2.5% and 12%7 8 9 with small
paediatric donor kidneys compared with a rate of 1.8% for adult donor
kidneys.9 Risk factors for thrombosis include: donor less than 5 years
old,8 10
11 cold ischaemic time longer than
24 hours,10 11 previous recipient transplantation,10 and increased reactive antibodies.
Although paediatric cadaveric dual kidney
transplantation is associated with a higher risk of early vascular
complications, paediatric donor kidneys should not be considered as
marginal, as long-term graft survival and function have been shown to be
superior.
When comparing the benefits of en-bloc dual kidney
transplantation, a study using the Scientific Registry of Transplant
Recipients registries data set has shown that for donor weight between 10
kg and 34 kg, en-bloc dual kidney transplantation resulted in superior
outcomes compared with single kidney transplantation.12
Another concern is the nephron mass of the
transplanted paediatric kidneys. In adult cohorts, studies have shown a
43% higher risk of late graft failure for a large body surface area
recipient receiving a kidney from a small donor, compared with
matched-size transplantation.13
However, this finding is not relevant to paediatric donors as their kidney
will undergo compensatory hypertrophy to improve function and glomerular
filtration rate over time.14 15 In addition, it has been shown that increasing
recipient body mass index was not a clear risk factor for poor outcome or
poor graft function with small paediatric donors.12
The current evidence suggests that paediatric dual
kidney transplantation is a feasible procedure, with superior long-term
graft function and outcome. Therefore, paediatric dual kidney
transplantation is a valuable option for patients with end-stage renal
disease and paediatric cadaveric kidneys should be sourced when available.
Author contributions
All authors contributed to the concept, acquisition
of data, analysis of data, drafting of the article, and critical revision
of important intellectual content.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity.
References
1. Moreno-Alarcón C, López-Cubillana P,
López-González PÁ, et al. Lich-Gregoir technique and routine use of double
J catheter as the best combination to avoid urinary complications in
kidney transplantation. Transplant Proc 2014;46:167-9. Crossref
2. Hobart MG, Modlin CS, Kapoor A, et al.
Transplantation of pediatric en bloc cadaver kidneys into adult
recipients. Transplantation 1998;66:1689-94. Crossref
3. Fine RN. Renal transplantation of the
infant and young child and the use of pediatric cadaver kidneys for
transplantation in pediatric and adult recipients. Am J Kidney Dis
1988;12:1-10. Crossref
4. Snanoudj R, Rabant M, Timsit MO, et al.
Donor-estimated GFR as an appropriate criterion for allocation of ECD
kidneys into single or dual kidney transplantation. Am J Transplant
2009;9:2542-51. Crossref
5. Thomusch O, Tittelbach-Helmrich D, Meyer
S, Drognitz O, Pisarski P. Twenty-year graft survival and graft function
analysis by a matched pair study between pediatric en bloc kidney and
deceased adult donors grafts. Transplantation 2009;88:920-5. Crossref
6. Hafner-Giessauf H, Mauric A, Müller H,
et al. Long-term outcome of en bloc pediatric kidney transplantation in
adult recipients—up to 22 years of center experience. Ann Transplant
2013;18:101-7. Crossref
7. Sureshkumar KK, Reddy CS, Nghiem DD,
Sandroni SE, Carpenter BJ. Superiority of pediatric en bloc renal
allografts over living donor kidneys: a long-term functional study.
Transplantation 2006;82:348-53. Crossref
8. Mohanka R, Basu A, Shapiro R, Kayler LK.
Single versus en bloc kidney transplantation from pediatric donors less
than or equal to 15 kg. Transplantation 2008;86:264-8. Crossref
9. Kayler LK, Magliocca J, Kim RD, Howard
R, Schold JD. Single kidney transplantation from young pediatric donors in
the United States. Am J Transplant 2009;9:2745-51. Crossref
10. Bresnahan BA, McBride MA, Cherikh WS,
Hariharan S. Risk factors for renal allograft survival from pediatric
cadaver donors: an analysis of United Network for Organ sharing data.
Transplantation 2001;72:256-61. Crossref
11. Singh A, Stablein D, Tejani A. Risk
factors for vascular thrombosis in pediatric renal transplantation: a
special report of the North American Pediatric Renal Transplant
Cooperative Study. Transplantation 1997;63:1263-7. Crossref
12. Kayler LK, Zendejas I, Gregg A, Wen X.
Kidney transplantation from small pediatric donors: does recipient body
mass index matter? Transplantation 2012;93:430-6. Crossref
13. Kasiske BL, Snyder JJ, Gilbertson D.
Inadequate donor size in cadaver kidney transplantation. J Am Soc Nephrol
2002;13:2152-9. Crossref
14. Dubourg L, Cochat P, Hadj-Aïssa A,
Tydén G, Berg UB. Better long-term functional adaptation to the child’s
size with pediatric compared to adult kidney donors. Kidney Int
2002;62:1454-60. Crossref
15. Halldorson JB, Bakthavatsalam R,
Salvalaggio PR, et al. Donor-recipient size matching influences early but
not late graft function after pediatric en-bloc kidney transplantation.
Transplantation 2010;89:208-14. Crossref