DOI: 10.12809/hkmj175078
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
Living-related renal transplantation in Hong Kong
KF Chau, FRCP (Lond, Glasg, Edin)
Department of Medicine, Queen Elizabeth Hospital,
Jordan, Hong Kong
Corresponding author: Dr KF Chau (ckfz02@ha.org.hk)
Renal transplantation is the best treatment for
end-stage renal disease, as it allows optimum rehabilitation with better
survival than haemodialysis or peritoneal dialysis: in 2016, the annual
mortality rate per 100 patient-years in Hong Kong was 1.88 for patients
who received a renal transplant, 17.89 for patients on peritoneal
dialysis, and 18.89 for those on haemodialysis.1
With a global shortage of cadaveric organs, living-related kidney donation
has become an important alternative, especially in countries with a low
cadaveric organ donation rate such as Japan. In Hong Kong, living-related
kidney transplants account for an average of 14.8% of all renal
transplants performed over the past 10 years.1
In this issue of the Hong Kong Medical Journal, the
characteristics and clinical outcomes of living renal donors in Hong Kong
are reported.2
Compared with a cadaveric kidney transplant, a
living-related kidney transplant has a higher graft survival rate: the
10-year graft survival rate was 70% for cadaveric and 81% for living
kidney transplant, and the 20-year graft survival rate was 44% for
cadaveric and 61% for living kidney transplant.1
This is due to multiple factors that include matching for the most
suitable donor, and elective surgery to minimise stress to the donor and
cold ischaemic time of the kidney. According to the Hospital Authority
Renal Registry, in 2016 the half-life of a cadaveric kidney transplant was
18 years, whereas that for a living kidney transplant was 30 years.1 Living-related kidney donation, however, carries
potential risks to the donor. The short-term risks include those related
to anaesthesia, bleeding, and infection. In the long term, there is an
increased risk of hypertension and proteinuria,3
4 as well as hypertension,
pre-eclampsia, and proteinuria during pregnancy.5
Laparoscopic nephrectomy rather than an open
procedure is now the preferred approach in many transplant centres for
living-kidney procurement. Comparative studies have shown a shorter
hospital stay and less bleeding, although the ischaemic time is longer
with the laparoscopic approach.6
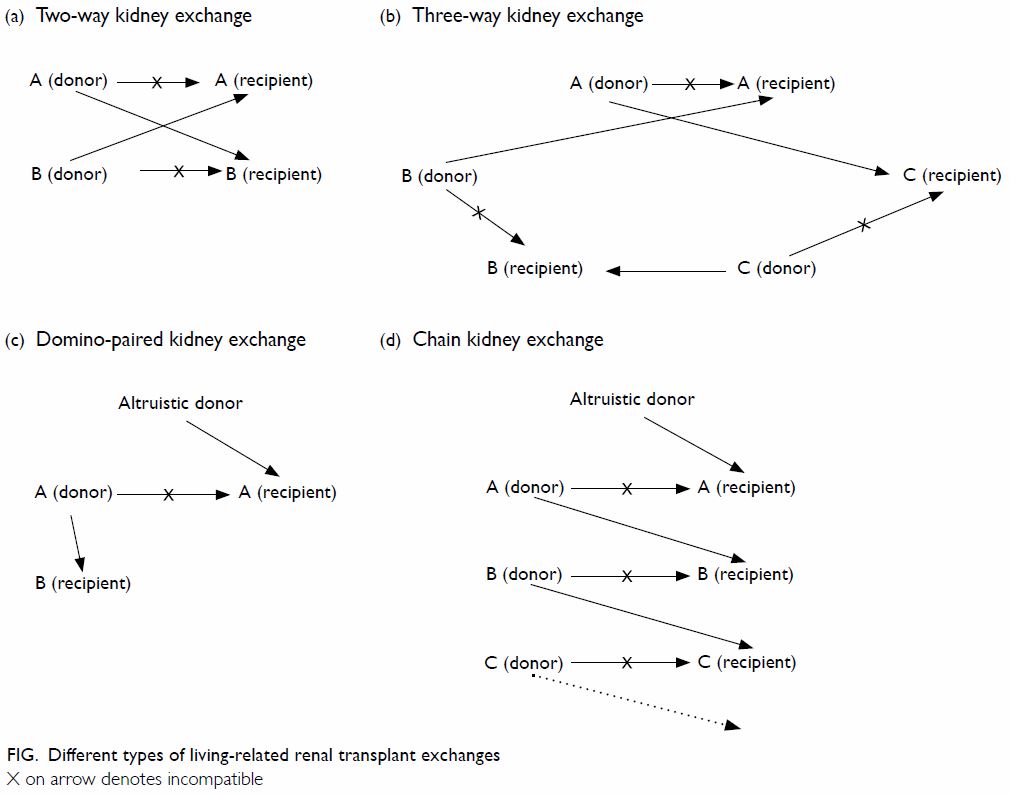
In order to overcome the problem of ABO blood group
or human leukocyte antigen incompatibility in living-related organ
donation, paired kidney exchange is becoming popular in many countries. It
may be a simple two-way exchange, a three-way exchange or, if an
altruistic donor is available, a domino-paired exchange or altruistic
donor chain (Fig). The longest chain was in 2012 in the United
States and involved 30 kidneys and 60 patients. In preparation for paired
kidney exchange in Hong Kong, the Food and Health Bureau plans to clarify
the legal situation by submitting a proposal to the Legislative Council.
Another means by which to overcome ABO blood group incompatibility is by a
pre-transplant immunosuppressive protocol that includes plasmapheresis
alone or together with rituximab.
Because of the potential risks to the donor, a
cadaveric kidney is still preferred. In 2016, the cadaveric organ donation
rate was 6.3 per million population in Hong Kong.1
Owing to the increasing gap between the number of patients requiring a
transplant and the number of organs available, the waiting time for a
cadaveric organ is increasing. The average waiting time is approximately 6
years but may also be as long as 28 years.1
Public education is essential to raise general awareness of the need for
cadaveric organ donation. Other measures include increasing human
resources for organ procurement in acute care hospitals, increasing the
effectiveness of donor referral and management and organ procurement, and
establishing an independent organ procurement organisation. These
initiatives are vital in order to boost organ donation rate in Hong Kong.
Declaration
The author has disclosed no conflicts of interest.
References
1. Hong Kong Hospital Authority Renal
Registry; 2016.
2. Hong YL, Yee CH, Leung CB, et al.
Characteristics and clinical outcomes of living renal donors in Hong Kong.
Hong Kong Med J 2018;24:11-7. Crossref
3. Chu KH, Poon CK, Lam CM, et al.
Long-term outcomes of living kidney donors: a single centre experience of
29 years. Nephrology (Carlton) 2012;17:85-8. Crossref
4. Okamoto M, Akioka K, Nobori S, et al.
Short- and long-term donor outcomes after kidney donation: analysis of 601
cases over a 35-year period at Japanese single center. Transplantation
2009;87:419-23. Crossref
5. Ibrahim HN, Akkina SK, Leister E, et al.
Pregnancy outcomes after kidney donation. Am J Transplant 2009;9:825-34. Crossref
6. Fonouni H, Mehrabi A, Golriz M, et al.
Comparison of the laparoscopic versus open live donor nephrectomy: an
overview of surgical complications and outcome. Langenbecks Arch Surg
2014;399:543-51. Crossref