Hong Kong Med J 2017 Dec;23(6):556–61
| Epub 10 Nov 2017
DOI: 10.12809/hkmj176840
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Evaluation of the awareness of, attitude to, and
knowledge about fertility preservation in cancer patients among clinical
practitioners in Hong Kong
Jacqueline PW Chung, MRCOG, FHKAM (Obstetrics and
Gynaecology); Terence TH Lao, MD, FRCOG; TC Li, PhD, FRCOG
Department of Obstetrics and Gynaecology, The
Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr Jacqueline PW Chung (jacquelinechung@cuhk.edu.hk)
Abstract
Introduction: Individuals can be
exposed to gonadotoxic agents in the course of treatment for cancers and
other medical conditions. Fertility preservation refers to strategies
that aim to preserve fertility by protecting it against the damage
inflicted by gonadotoxic treatment. Many young patients are prescribed
gonadotoxic treatment without prior counselling. This study aimed to
study the awareness of, attitude to, and knowledge about fertility
preservation among clinicians in Hong Kong.
Methods: This was a
cross-sectional study carried out between June and December 2016 using a
self-administered questionnaire. The questionnaires were sent to
clinicians in the departments of Clinical Oncology, Haematology,
Obstetrics and Gynaecology, Paediatrics, and Surgery in various public
hospitals of Hong Kong.
Results: In this survey, 36.5%
(167 of 457) of clinicians responded. Of the respondents, only 45.6%
were familiar with fertility preservation. The factors considered most
important for referral were, in decreasing order of importance,
prognosis of the patient, patient’s desire to have children, time
available before commencing gonadotoxic treatment, type of cancer, and
type of gonadotoxic treatment. The majority of clinicians did not refer
their patients for fertility preservation due to a lack of available
time before treatment, considerable risk of recurrence, poor prognosis,
financial constraints, need for cancer treatment as top priority at the
time, and lack of awareness of such service. Almost all agreed that a
dedicated centre should be set up for fertility preservation and 76.5%
agreed that fertility preservation should be provided as a public
service.
Conclusion: Awareness among
clinical practitioners of fertility preservation remains weak. Education
of clinicians and the establishment of a dedicated fertility
preservation centre are required.
New knowledge added by this study
- Awareness of and knowledge about fertility preservation among clinical practitioners remains weak.
- Factors considered most important for referral were, in decreasing order of importance, prognosis of the patient, the desire to have children, time available before commencing gonadotoxic treatment, type of cancer, and gonadotoxic treatment.
- Increased awareness of fertility preservation among clinicians is required, especially of new strategies involved in reproductive technology.
- Education of clinicians and establishment of a dedicated fertility preservation centre, and an efficient referral system are required.
Introduction
The human gonads, both the ovaries and testes, are
sensitive organs susceptible to injury by disease, medications, and
chemotherapy and radiation for the treatment of cancers and other medical
conditions including autoimmune diseases such as systemic lupus
erythematosus and haematological diseases.1
2 3
Individuals who survive may later consider starting a family, yet by this
time they often face problems of gonadal injury and ageing. If their
fertility can be preserved before such treatment is performed, especially
at a young age, individuals will be able to retain or regain their
fertility after completion of treatment.
Current advances in reproductive technology have
enabled fertility to be retained by preservation of gonadal function such
that gametes as well as hormones continue to be produced despite damage
inflicted by gonadotoxic treatment. Fertility preservation methods include
fertility-sparing surgery, radiation shielding, and gonadotropin-releasing
hormone agonists for gonadal suppression during chemotherapy. In addition,
assisted reproductive technology—including intracytoplasmic sperm
insemination; and oocyte, embryo and ovarian tissue cryopreservation—have
expanded fertility preservation options that can now be applied to a
broader spectrum of patients including those who are pre-pubertal, and
those with insufficient time prior to initiation of gonadotoxic treatment.4 5
6
Although any adverse effects of treatment on
fertility should have been discussed by clinicians before treatment, up to
half of the patients are not referred to fertility specialists for
fertility preservation.7 To the
best of our knowledge, there is no local literature on the awareness of,
attitude towards, and knowledge about fertility preservation among
clinicians in Hong Kong. We therefore conducted a questionnaire survey to
address this issue.
Methods
This was a cross-sectional survey to evaluate the
awareness of, attitude towards, and knowledge about fertility preservation
among local clinicians in Hong Kong. The study was conducted between June
2016 and December 2016. Ethical approval for the study was obtained from
the institutional Survey and Behavioural Research Ethics Committee.
Eligible subjects were identified from the
Specialist Register of Medical Council of Hong Kong who were clinicians
worked in public hospitals and specialised in the field of Clinical
Oncology, Haematology, Obstetrics and Gynaecology, Paediatrics, and
Surgery. Potential candidates were selected by convenience sampling from
each specialty from various hospitals and their work addresses identified
via the electronic staff directory or organisational chart provided by the
Hospital Authority intranet. The study questionnaire was mailed to them
internally.
The self-administered questionnaire included a
brief explanation of the survey. If the subject agreed to participate,
they were asked to complete the questionnaire and return it in the stamped
addressed envelope. The questionnaires were completed and returned
anonymously.
The questionnaire comprised 29 items in two parts.
The first part included questions about the baseline demographics and
specialty of the participants. Their views on the demand for the fertility
preservation service, factors they considered when making a decision about
fertility preservation, and the difficulties encountered in discussing
fertility issues with their patients were examined. Practical questions
about the potential costs and the need for a dedicated fertility
preservation clinic were also addressed.
The SPSS (Windows version 20.0; IBM Corp, Armonk
[NY], US) was used for data entry and analysis. Demographic data were
summarised by means, medians, and percentages. The Chi squared test (χ2
test) was used for categorical data such as comparing the awareness of
fertility preservation among different specialties, cancer type, and
demographic background. Student’s t test (t test) was used
for continuous variables of age and years of practice. Results with a P
value of <0.05 were considered statistically significant.
Results
Of the 467 questionnaires sent to a convenient
sample of clinicians, 10 were returned unopened because of an outdated
work address. A total of 167 questionnaires of the remaining 457
questionnaires were returned, giving an overall response rate of 36.5%.
The response rates for specific specialties were: 55.3% (68/123) for
obstetricians and gynaecologists, 37.5% (48/128) for surgeons
(general/breast/urology), 18.5% (22/119) for paediatricians, and 16.5%
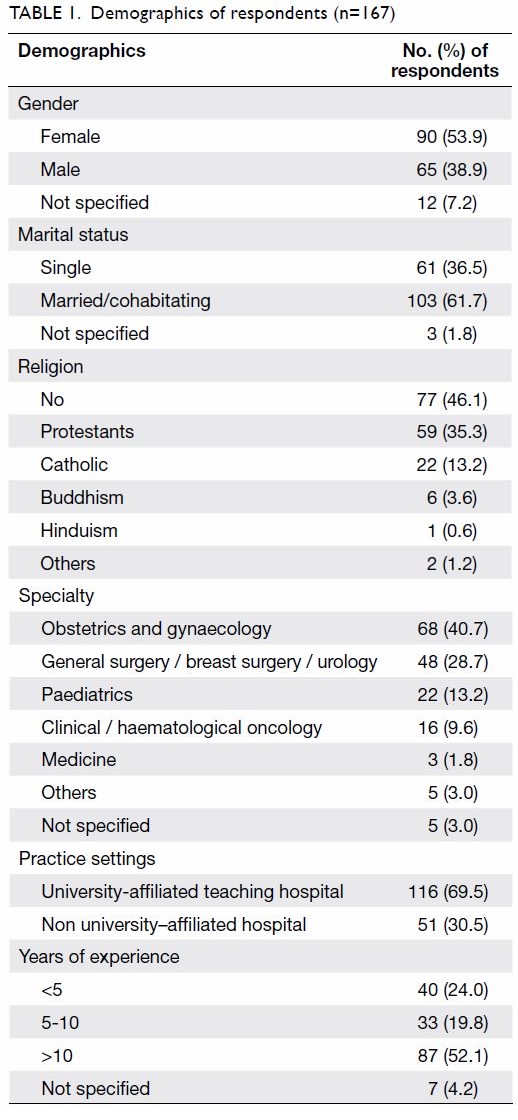
(16/97) for haematologists or clinical oncologists. Table
1 summarises the baseline demographics of the respondents. Some of
the respondents did not answer all questions, hence the denominators of
each response are stated.
Up to 85.0% (142/167) of respondents cared for
cancer patients in their daily practice and 76.0% (127/167) dealt with
treatments that may threaten fertility. The most commonly encountered
cancers were gynaecological cancer (50.0%, 71/142), followed by urological
cancer (25.4%, 36/142), haematological cancer (20.4%, 29/142),
neurological cancer (19.7%, 28/142), musculoskeletal cancer (18.3%,
26/142), gastrointestinal cancer (16.2%, 23/142), and others (6.3%,
9/142).
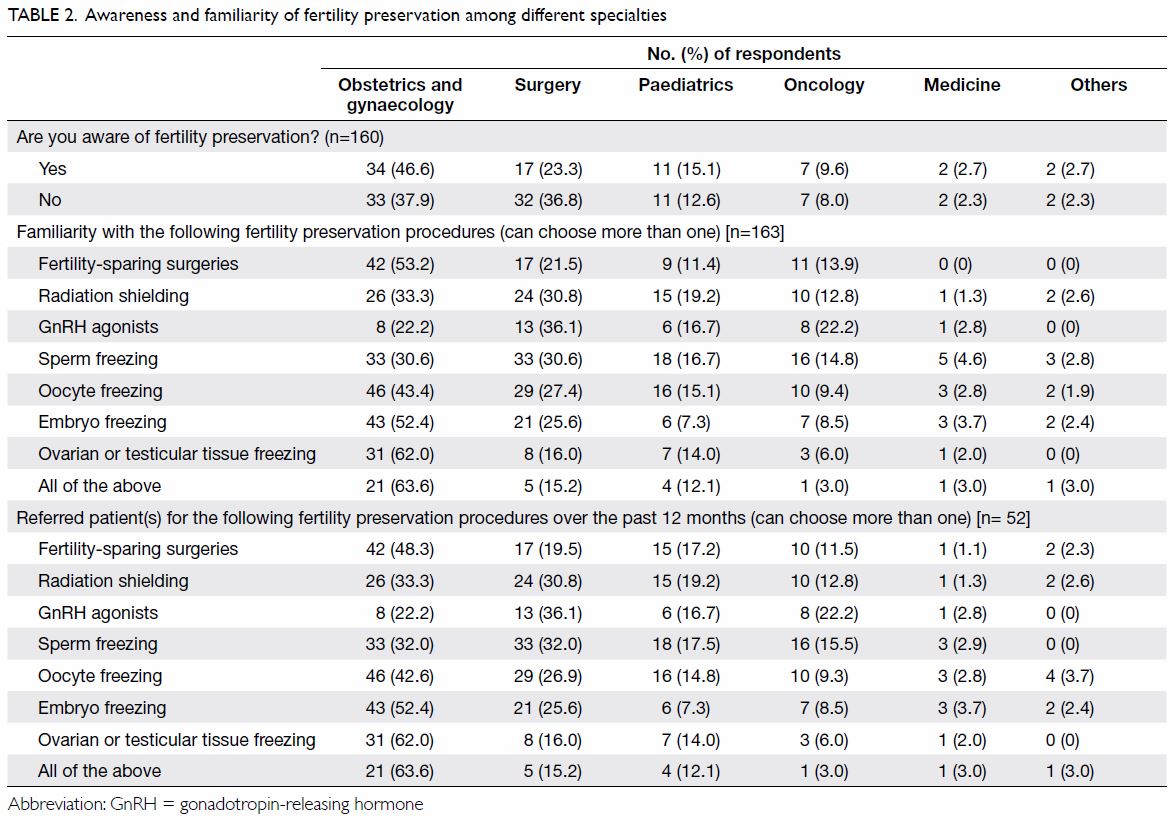
Only 45.6% (73/160) of the respondents were
familiar with fertility preservation. The three most familiar means were
sperm freezing (66.3%, 108/163), followed by oocyte freezing (65.0%,
106/163) and embryo freezing (50.3%, 82/163). Table 2 shows the awareness of various fertility
preservation strategies among clinicians from different specialties.
Nevertheless, 68.3% (112/164) of respondents had
never referred a patient for fertility preservation. Among the 52
respondents who had, 88.5% (46/52) had referred fewer than five patients
and 11.5% had referred more than five patients over the past 12 months.
Sperm cryopreservation was the most commonly referred fertility
preservation method. There was no significant association of the
demographic background of respondents in terms of age (P=0.334), gender
(P=0.325), marital status (P=0.060), presence of any children (P=0.574),
or practice setting (P=0.749) with awareness or frequency of referral for
fertility preservation. Up to 90.7% (146/161) would consider referral of a
patient to a fertility specialist for fertility preservation if it delayed
treatment by 1 week, 83.2% (134/161) if the delay was <2 weeks, 41.6%
(67/161) for <4 weeks, and 6.2% (10/161) for <8 weeks.
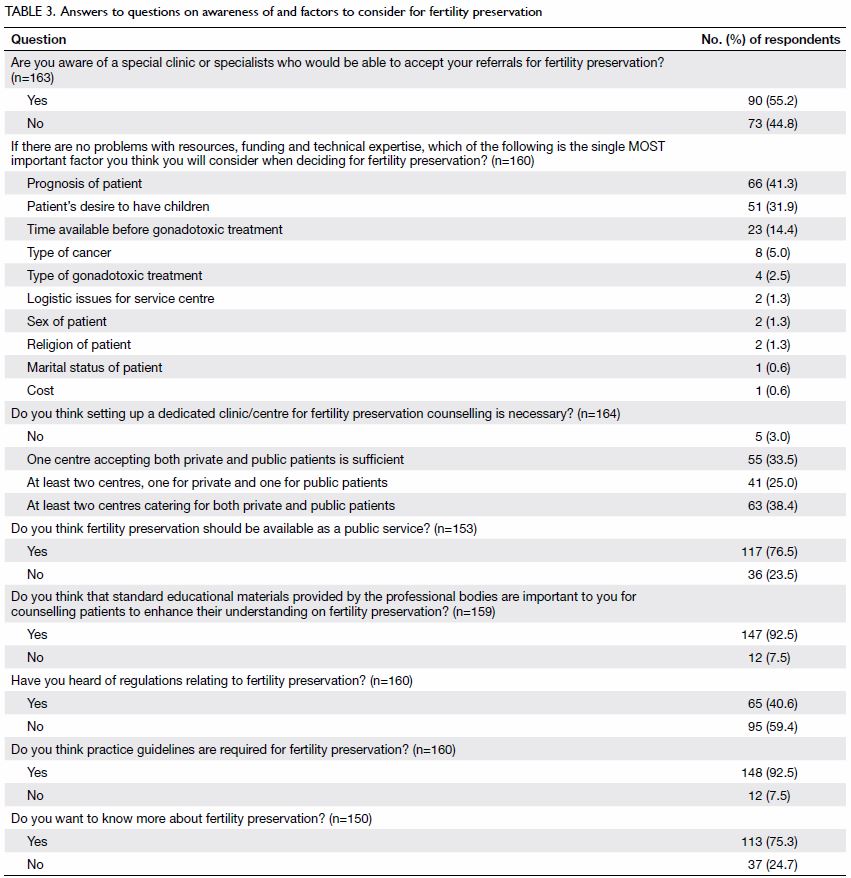
Table 3 shows the responses to questions about
fertility preservation. Up to 76.5% (117/153) of the respondents agree
that fertility preservation should be available as a public service. The
top five difficulties encountered by clinicians in discussing fertility
preservation were: no time before commencement of gonadotoxic treatment
(60.6%, 97/160), high risk of cancer recurrence (53.8%, 86/160) or poor
prognosis, financial constraints (46.9%, 75/160), treating the cancer as
top priority (38.8%, 62/160), and not being aware of any place or person
to whom their patients could be referred to (35.0%, 56/160).
Discussion
Gonadotoxic treatments for cancer, especially those
requiring chemotherapy with alkylating agents and total body irradiation
or pelvic/whole-body radiation, have a significant negative impact on
ovarian and testicular function.1
These impacts may be irreversible depending on the patient’s age, total
dose administered, and gonadal reserve at the time of treatment.
Fertility preservation has gained increasing
attention worldwide over the past decade as treatment advances result in
more and more survivors of childhood cancers and adult malignancies who
are expected to lead a normal life and to start a family of their own.1
Our study revealed several important findings.
First, it showed a rather low awareness of fertility preservation among
our respondents. Most agreed that their patients should be referred for
fertility preservation even if it meant a delay in their treatment.
Although up to three quarters of respondents dealt with treatment that
might impair fertility, less than half were familiar with fertility
preservation. Our previous study showed significant underutilisation of a
sperm cryopreservation service over the past two decades.8 There is an imperative need to provide better education
and campaigns to raise awareness about various options for fertility
preservation available in Hong Kong.
Second, our study evaluated the difficulties or
barriers encountered by clinicians in referring patients for fertility
preservation. Similar to previous studies, a high risk of disease
recurrence and poor prognosis discouraged discussion about future
fertility.9 10 11 More than
half of the respondents also expressed insufficient time for fertility
preservation procedures before initiation of gonadotoxic treatment.
Nonetheless sperm cryopreservation is a simple and effective method of
preserving fertility for male patients who need to produce only a semen
sample by masturbation for cryopreservation at any time before initiation
of gonadotoxic treatment.8 In
female patients, fertility preservation is slightly more complicated and
time-consuming. Ovarian stimulation for oocyte or embryo cryopreservation
takes at least 8 to 12 days although the introduction of random-start
protocols for ovarian stimulation and ovarian tissue cryopreservation now
provide a new option for those with insufficient time and for pre-pubertal
adolescents.5 6 12 13 Early referral to a fertility specialist at the time
of diagnosis of disease and prior to treatment commencement is the key to
maximising the success of fertility preservation and allows a greater
window of opportunity for preserving fertility.14
Again, this highlighted the need for training and education of clinical
practitioners in the most updated advances in assisted reproductive
technology, especially in specialties other than obstetrics and
gynaecology.
Third, almost all respondents agreed there was a
need for a dedicated clinic or referral centre. Most suggested two
centres, catering to both private and public patients. No such referral
centre is currently available in Hong Kong. An important prerequisite is a
quick and efficient system whereby patients can be referred for fertility
preservation counselling by a fertility specialist as soon as their
diagnosis of cancer is made.15
Moreover, proper regulations and guidelines about fertility preservation
should be established and communicated to the public and clinicians.
Printed information about the effect of cancer treatment on fertility and
the options for fertility preservation techniques, including both
established and experimental, should be available for all clinicians to
hand out to their patients. A 24-hour hotline should be set up and contact
addresses disseminated widely on websites or to clinicians who care for
patients with cancer.
Fourth, financial constraints should be addressed.
Cryopreservation of gametes and embryos is expensive and is currently only
available in Hong Kong as a private service. Government and
non-governmental organisations should consider funding this in selected
patients. Up to 76.5% of our respondents agreed that fertility
preservation should be provided as a public service.
In addition, there appeared to be varying levels of
awareness among clinicians from different specialties about fertility
preservation techniques. Different specialists may be more or less exposed
to the most up-to-date trends in the field of assisted reproductive
technology. Our data were not sufficiently representative to explore this
issue. Further studies are required to evaluate this.
Our study is limited by its small sample size and
low response rate. Ideally, all clinicians from both public and private
sectors of all specialties should be included but this would be costly and
impractical. Our study included a higher proportion of clinicians from
university-affiliated hospitals and this might have added additional
self-selection bias to the study as they were more willing to participate
in research. In addition, clinicians with an interest in this area may
have been more likely to respond to this study. Potential candidates were
sampled by convenience from each specialty from various hospitals and
might not have represented the views of all clinicians. Caution should be
exercised when making generalisations about these data from a sample group
that was self-selected. Nonetheless this is the first study to evaluate
the awareness of, attitude towards, and knowledge about fertility
preservation among clinicians in Hong Kong. It provides important
information that can be applied in setting up a fertility preservation
centre and in the design of training modules and educational materials for
clinical practitioners.
Reassuringly, our studies show an overall
encouraging positive attitude among local clinicians towards fertility
preservation, with the majority wanting to know more. Knowledge about
fertility preservation techniques is insufficient. There is a need to
improve awareness of and referral for this service. As the field of
fertility preservation continues to grow, it is important to include the
topic of fertility preservation in the curriculum of our medical schools
to increase the knowledge and awareness of our future clinicians.
Seminars, workshops, and conferences for those interested in this field
should be regularly arranged. Fundraising campaigns and grants for
research in this field should be encouraged. A multidisciplinary team and
dedicated centre with an efficient referral system should be set up as
soon as possible to provide fertility risk assessment and counselling for
patients. Further studies are required to explore how fertility concerns
are being addressed during the management of serious medical conditions,
especially cancer care, and how clinicians can communicate with cancer
patients about the options for fertility preservation.
Acknowledgements
We would like to thank Miss Elaine Yee-lee Ng, Miss
Sze-yan Lo, and Mr Ka-chun Keung for data collection and entry. We would
also like to thank all the clinicians who participated in this study.
Declaration
All authors have disclosed no conflicts of
interest.
References
1. Rodriguez-Wallberg KA, Oktay K.
Fertility preservation during cancer treatment: clinical guidelines.
Cancer Manag Res 2014;6:105-17.
2. Falcone T, Bedaiwy MA. Fertility
preservation and pregnancy outcome after malignancy. Curr Opin Obstet
Gynecol 2005;17:21-6. Crossref
3. Loren AW, Mangu PB, Beck LN, et al.
Fertility preservation for patients with cancer: American Society of
Clinical Oncology clinical practice guideline update. J Clin Oncol
2013;31:2500-10. Crossref
4. Ethics Committee of American Society for
Reproductive Medicine. Fertility preservation and reproduction in patients
facing gonadotoxic therapies: a committee opinion. Fertil Steril
2013;100:1224-31. Crossref
5. Dolmans MM, Jadoul P, Gilliaux S, et al.
A review of 15 years of ovarian tissue bank activities. J Assist Reprod
Genet 2013;30:305-14. Crossref
6. Donnez J, Martinez-Madrid B, Jadoul P,
Van Langendonckt A, Demylle D, Dolmans MM. Ovarian tissue cryopreservation
and transplantation: a review. Hum Reprod Update 2006;12:519-35. Crossref
7. Forman EJ, Anders CK, Behera MA. A
nationwide survey of oncologists regarding treatment-related infertility
and fertility preservation in female cancer patients. Fertil Steril
2010;94:1652-6. Crossref
8. Chung JP, Haines CJ, Kong GW. Sperm
cryopreservation for Chinese male cancer patients: a 17-year retrospective
analysis in an assisted reproductive unit in Hong Kong. Hong Kong Med J
2013;19:525-30.
9. Shimizu C, Bando H, Kato T, Mizota Y,
Yamamoto S, Fujiwara Y. Physicians’ knowledge, attitude, and behavior
regarding fertility issues for young breast cancer patients: a national
survey for breast care specialists. Breast Cancer 2013;20:230-40. Crossref
10. Arafa MA, Rabah DM. Attitudes and
practices of oncologists toward fertility preservation. J Pediatr Hematol
Oncol 2011;33:203-7. Crossref
11. Collins IM, Fay L, Kennedy MJ.
Strategies for fertility preservation after chemotherapy: awareness among
Irish cancer specialists. Ir Med J 2011;104:6-9.
12. Cakmak H, Rosen MP. Random-start
ovarian stimulation in patients with cancer. Curr Opin Obstet Gynecol
2015;27:215-21. Crossref
13. Rashidi BH, Tehrani ES, Ghaffari F.
Ovarian stimulation for emergency fertility preservation in cancer
patients: a case series study. Gynecol Oncol Rep 2014;10:19-21. Crossref
14. Yee S, Fuller-Thomson E, Lau A,
Greenblatt EM. Fertility preservation practices among Ontario oncologists.
J Cancer Educ 2012;27:362-8. Crossref
15. Ghazeeri G, Zebian D, Nassar AH, et
al. Knowledge, attitudes and awareness regarding fertility preservation
among oncologists and clinical practitioners in Lebanon. Hum Fertil (Camb)
2016;19:127-33. Crossref