Hong Kong Med J 2017 Aug;23(4):416.e4–5
DOI: 10.12809/hkmj165022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Birt-Hogg-Dubé syndrome: a rare cause of familial spontaneous pneumothorax
HM Luk, FHKAM (Paediatrics); Tony MF Tong, MSc; Ivan FM Lo, FHKAM (Paediatrics)
Clinical Genetic Service, Department of Health, 3/F Cheung Sha Wan Jockey Club Clinic, 2 Kwong Lee Road, Shamshuipo, Hong Kong
Corresponding author: Dr HM Luk (luksite@gmail.com)
A family with a strong history of pneumothorax
was referred to our genetic clinic for assessment.
There were three siblings who had all developed
spontaneous pneumothorax at the age of 30, 58,
and 59 years. All were non-smokers with no pre-existing
pulmonary disease. High-resolution
computed tomography of the thorax for all showed multiple thin-walled pulmonary cysts of variable
size on both sides, mainly located at the basal and
peripheral lung regions (Fig). Lung biopsy was not
informative. Physical examination revealed multiple
smooth, dome-shaped papules over the face and
ears in one of siblings (Fig b). There were no other
features of tuberous sclerosis or history of renal disease in the family. Based on the dermatological
findings and diffuse multicystic lung disease, Birt-Hogg-Dubé (BHD) syndrome was suspected.
FLCN gene analysis revealed a heterozygous
FLCN{NM_144997.5}:c.1285dupC mutation in all
affected members. The diagnosis of BHD syndrome
was substantiated. Renal imaging was arranged for
surveillance of potential renal cell carcinoma.
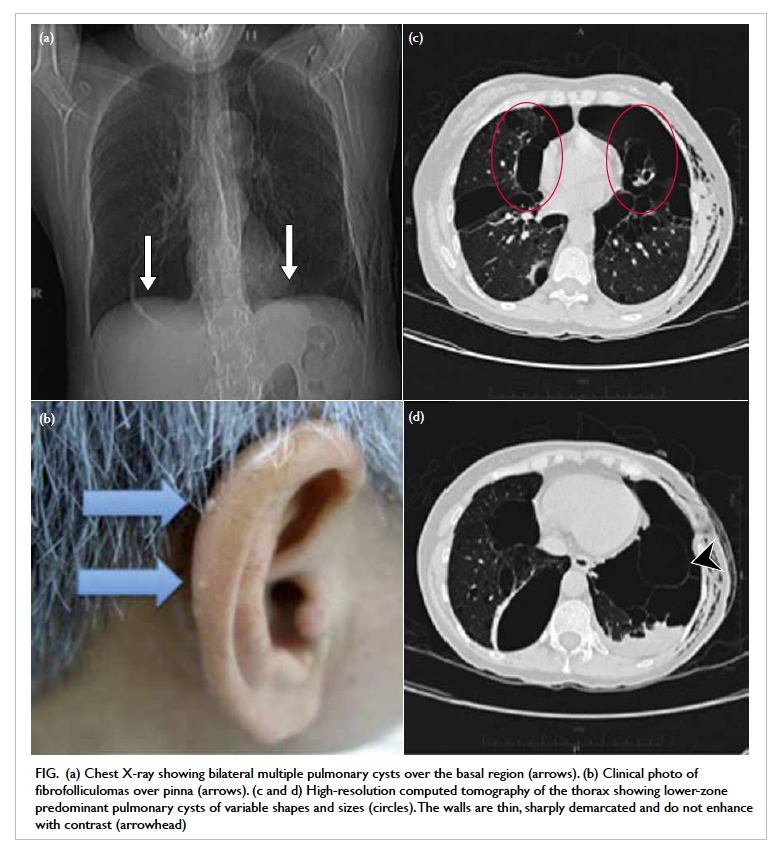
Figure. (a) Chest X-ray showing bilateral multiple pulmonary cysts over the basal region (arrows). (b) Clinical photo of fibrofolliculomas over pinna (arrows). (c and d) High-resolution computed tomography of the thorax showing lower-zone predominant pulmonary cysts of variable shapes and sizes (circles). The walls are thin, sharply demarcated and do not enhance with contrast (arrowhead)
The BHD syndrome is a rare autosomal
dominant disease characterised by three major
organ manifestations1:
(1) Fibrofolliculomas and other benign skin tumours
such as trichodiscomas and acrochordons;
these skin lesions are predominantly located on
the facial, cervical, and upper truncal regions
as smooth, dome-shaped, and white to flesh-coloured
papules.
(2) Increased susceptibility to renal cell carcinoma
of mixed histologies; the most frequent subtype
is a hybrid oncocytic tumour with features of
renal oncocytoma and chromophobe renal cell
carcinoma.
(3) Multiple bilateral pulmonary cysts and
spontaneous pneumothorax.
The clinical features of BHD syndrome are
heterogeneous with wide intra-familial and inter-familial
variation. It is caused by mutations of the
FLCN gene. Any combination of the cutaneous,
renal, and pulmonary features mentioned above
present in an individual or multiple family members
should alert the clinician to the possibility of BHD
syndrome.
Bilateral multiple pulmonary cysts are a highly
penetrant feature in BHD syndrome. As a result,
the risk of pneumothorax in BHD patients is 50
times higher than that of the general population.2
Approximately 80% to 90% of BHD patients develop
lung cysts, usually after early mid-adulthood. The
BHD-associated lung cysts tend to be located at
the basilar and mediastinal regions of the lungs, in
contrast to the typically apical location in primary spontaneous pneumothorax and emphysema.
Radiologically, the BHD-associated lung cysts are
usually irregularly shaped, variable in size and
number, and with sharply demarcated thin walls that
do not enhance on computed tomographic imaging.
Fibrofolliculomas are present in more than
80% of patients with BHD syndrome and typically
appear after the age of 20 years. They are dome-shaped,
white to flesh-coloured, non-painful and
non-pruritic papules located on the facial, cervical,
and upper truncal regions.
The most threatening complication of BHD
syndrome is renal cell carcinoma. It occurs in
approximately 15% of BHD patients by the age of 70
years.3 Therefore regular surveillance is mandatory.
Physicians should be alert to the possibility of
BHD syndrome in a patient who presents with diffuse
cystic lung disease, particularly in the presence of
a positive family history. Early referral to a clinical
genetic service and multidisciplinary management
is recommended. Early diagnosis and regular
renal surveillance aim to greatly reduce renal cell
carcinoma–associated morbidity and mortality.
References
1. Menko FH, van Steensel MA, Giraud S, et al. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet
Oncol 2009;10:1199-206. Crossref
2. Gupta N, Seyama K, McCormack FX. Pulmonary
manifestations of Birt-Hogg-Dubé syndrome. Fam Cancer
2013;12:387-96. Crossref
3. Stamatakis L, Metwalli AR, Middelton LA, Marston
Linehan W. Diagnosis and management of BHD-associated
kidney cancer. Fam Cancer 2013;12:397-402. Crossref

