Hong Kong Med J 2017 Aug;23(4):374–80 | Epub 28 Jun 2017
DOI: 10.12809/hkmj165005
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Early surgery for Hong Kong Chinese elderly patients with hip fracture reduces short-term and long-term mortality
Stephanie KK Liu, MB, BS1; Angela WH Ho, MB, ChB, FHKAM (Orthopaedic Surgery)2; SH Wong, MB, BS, FHKAM (Orthopaedic Surgery)2
1 Department of Orthopaedics and Traumatology, Princess Margaret Hospital, Laichikok, Hong Kong
2 Department of Orthopaedics and Traumatology, Caritas Medical Centre, Shamshuipo, Hong Kong
An earlier version of this paper was presented at the Young Investigator
Awards, 15th Regional Osteoporosis Conference held in Hong Kong on
24-25 May 2014; and at the International Osteoporosis Foundation (IOF)
Young Investigator Awards, IOF Regionals 5th Asia-Pacific Osteoporosis
Meeting held in Taipei, Taiwan on 15 November 2014.
Corresponding author: Dr Angela WH Ho (angelaho@alumni.cuhk.net)
Abstract
Introduction: Studies have shown that early surgery
reduces hospital and 1-year mortality in elderly
patients with hip fracture, but no major study has
examined such relationship in Hong Kong. This study
aimed to explore the relationship of early surgery
and mortality in a Chinese elderly population with
hip fracture.
Methods: This observational study included
patients attending public hospitals in Hong Kong.
All patients who underwent surgery for geriatric
hip fracture in public hospitals from January 2000
to December 2011 were studied. Data were retrieved
and collected from the Clinical Data Analysis and
Reporting System of the Hospital Authority. Patients
were divided into three groups according to timing of
surgery: early (0-2 days after admission), delayed (3-4
days after admission), and late (≥5 days after admission)
groups. Based on the date of death, we analysed
30-day and 1-year mortality, regardless of cause of
death. Comparison of mortality rates was also made
between the period before and after implementation
of Key Performance Indicator formulated by the
Hospital Authority.
Results: The overall 1-year mortality rate was
16.8%. The relative risks of 1-year mortality were 1.21
and 1.52 when the delayed and late
groups were compared with the early group, respectively. The hazard ratios of long-term mortality were 1.16 (95% confidence interval, 1.13-1.20) and 1.37 (1.33-1.41),
respectively for the same comparison.
Conclusion: Prevalence of geriatric hip fracture will
continue to rise and further increase the burden on
our health care system. After implementation of
Key Performance Indicator, most elderly patients
with hip fracture underwent surgery within 2 days
provided they were medically fit. Early surgery can
reduce both short-term and long-term mortality.
Setting up a fragility fracture registry would be
beneficial for further studies.
New knowledge added by this study
- This study provides evidence that Key Performance Indicator (KPI) can increase the percentage of patients who undergo early surgery and improve their clinical outcome.
- Most medically fit patients were identified for early surgery within 2 days.
- High-risk patients with medical co-morbidities were identified for prompt preoperative optimisation under KPI.
- Early surgery should be considered the standard of care for management of elderly patients with hip fracture.
Introduction
Hip fracture has a high prevalence in an ageing
population and places a major burden on and
challenge to our health care system. In Hong Kong,
the number of geriatric hip fractures managed
in the Hospital Authority increased from 3678
in 2000 to 4579 in 2011.1 International clinical
guidelines recommend surgical treatment within
2 days of admission.2 3 4 Geriatric hip fracture was
selected as the first Key Performance Indicator (KPI)
for orthopaedics in Hong Kong by the Hospital
Authority in 2009 with an aim to limit preoperative
length of stay to no more than 2 days for 70% of
patients with hip fracture.5 Studies have shown
that early surgery reduces hospital and 1-year
mortality in elderly patients with hip fracture,6 7 8 but
no major study has examined such relationship. This
study was conducted to explore the relationship
of early surgery and mortality in a Chinese elderly
population with hip fracture.
Methods
We undertook a retrospective review of data collected from the Clinical Data Analysis and
Reporting System of the Hospital Authority of Hong
Kong for all patients aged 65 years or above who
presented to any public hospital between January
2000 and December 2011 with hip fracture that
was treated surgically. Those patients with a disease
coding of acute hip fracture (ICD-9-CM diagnosis
codes 820.8, 820.09, 820.02, 820.03, 820.20, and
820.22) were retrieved; operations for geriatric hip
fracture were defined as a patient episode with ICD-9-CM procedure codes of 81.52, 51.51, 81.40, 79.15,
79.35, or 78.55. Only elderly patients with a disease
code for acute hip fracture and procedure code for
hip fracture surgery were included in the current
study. Those who had second hip fracture surgery
or surgery for complications arising from a previous
hip fracture were excluded.
Patients were divided into three groups
according to timing of surgery: early (0-2 calendar
days after admission), delayed (3-4 calendar days
after admission), and late (≥5 calendar days after
admission) groups. Dates of death were retrieved
from the Deaths Registries of the Hong Kong SAR.
Based on the date of death, we analysed the 30-day
and 1-year mortality regardless of cause. Mortality
was calculated using Kaplan-Meier survival analysis.
Among the three groups, the 30-day and 1-year
mortality were compared using Chi squared
test. Long-term mortality was compared by Cox
regression models using age, gender, and year as
covariates. Subgroup analysis of mortality before
(year 2000-2008) and after (year 2009-2011) the execution
of KPI for hip fracture was also performed. The
result was considered statistically significant if the P
value was <0.05. All analyses were performed using
SAS version 9.3 (SAS Institute Inc, Cary [NC], US) software. The
principles outlined in the Declaration of Helsinki
have been followed.
Results
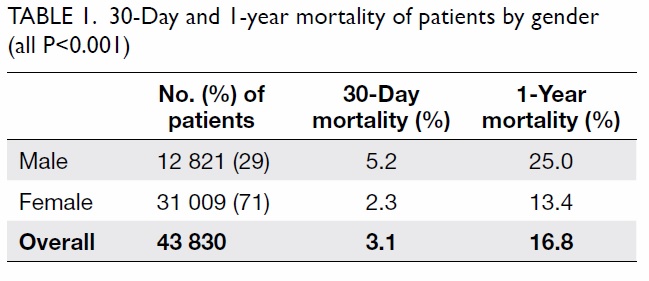
The study identified 43 830 patients (12 821 men
and 31 009 women) with age ranging from 65
to 112 years (mean, 82 years). Early surgery was
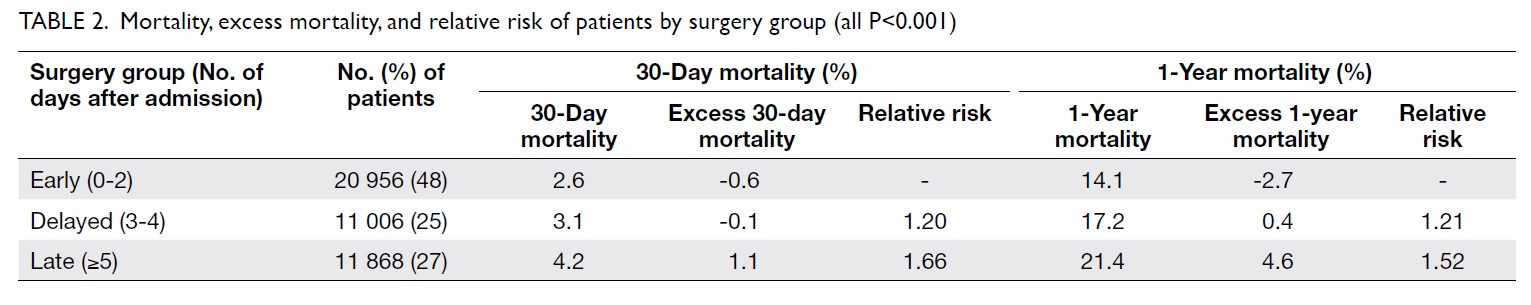
performed in 48%, delayed surgery in 25%, and late
surgery in 27% of all patients. The 30-day and 1-year
mortality of the patients by gender and surgery
group are listed in Tables 1 and 2, respectively.
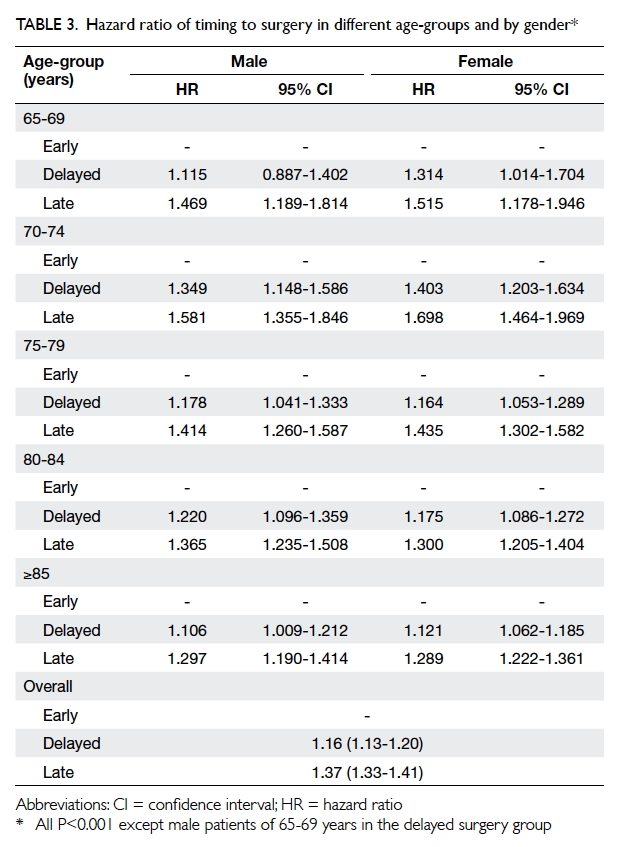
For each age-group (65-69, 70-74, 75-79, 80-84,
≥85 years), the percentage of early, delayed, or late
surgery was similar with a deviation of only 1%
to 2%. Linear regression revealed no correlation
between the timing of surgery and patient age.
The 1-year mortality rate of all hip fractures was
16.8% (25.0% for males and 13.4% for females). The
1-year mortality rates of early, delayed, and late surgery
groups were 14.1%, 17.2%, and 21.4%, respectively.
The relative risks of 1-year mortality were 1.21 (95%
confidence interval [CI], 1.16-1.29) and 1.52 (95%
CI, 1.45-1.59) when the delayed and
late groups were compared with the early group, respectively. All
results were statistically significant.
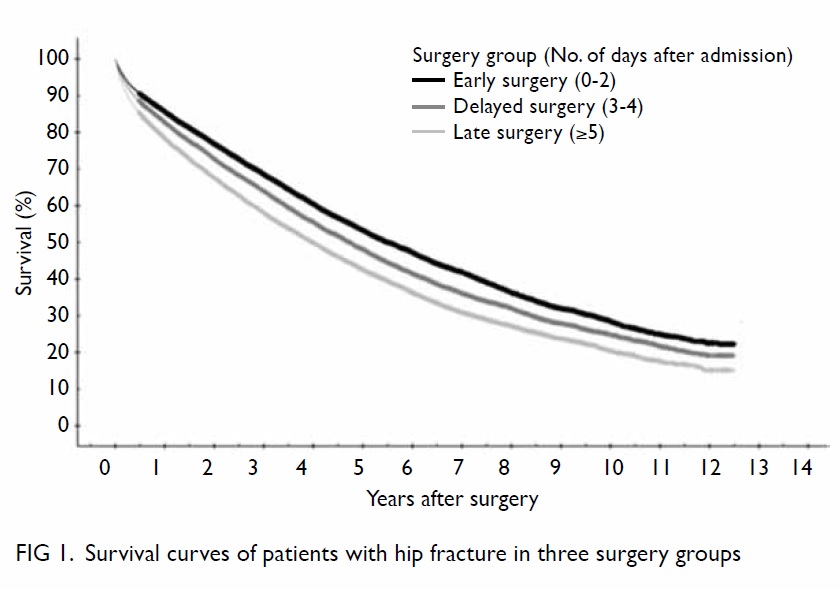
The long-term mortality rate was also
significantly related to the timing of surgery using
log rank test (Fig 1). The hazard ratios (HRs) of long-term
mortality were 1.16 (95% CI, 1.13-1.20) and 1.37
(95% CI, 1.33-1.41) when the delayed
group and late group were compared with the early
group, respectively. Such significant difference was observed
across all age-groups for both genders, except those
male patients of 65-69 years in the delayed surgery
group (Table 3). In men, the respective HR was 1.12-1.35 and 1.30-1.58 when the delayed group and late
group were compared with the early group, with the
highest HR noted in the age-group of 70-74 years.
Similar results were observed in females: the HR
varied with age and ranged from 1.12-1.40 and 1.29-1.70 respectively when the delayed group and late
group were compared with the early group, with the
highest HR in the age-group of 70-74 years (Table 3).
Subgroup analysis of the mortality rate before
(year 2000-2008) and after (year 2009-2011) execution
of KPI for hip fracture was performed. Mortality
rate increased as surgery delay was prolonged. The
respective relative risk of 1-year mortality before
KPI was 1.12 (95% CI, 1.04-1.21) and 1.27 (95% CI,
1.19-1.36) when the delayed group and late group
were compared with the early group; the corresponding figures after KPI were 1.15 (95% CI, 0.99-1.34) and 1.39 (95% CI, 1.20-1.60). The overall 1-year
mortality was lower in the post-KPI group (relative
risk=0.81; P<0.001; 95% CI, 0.76-0.86). All results
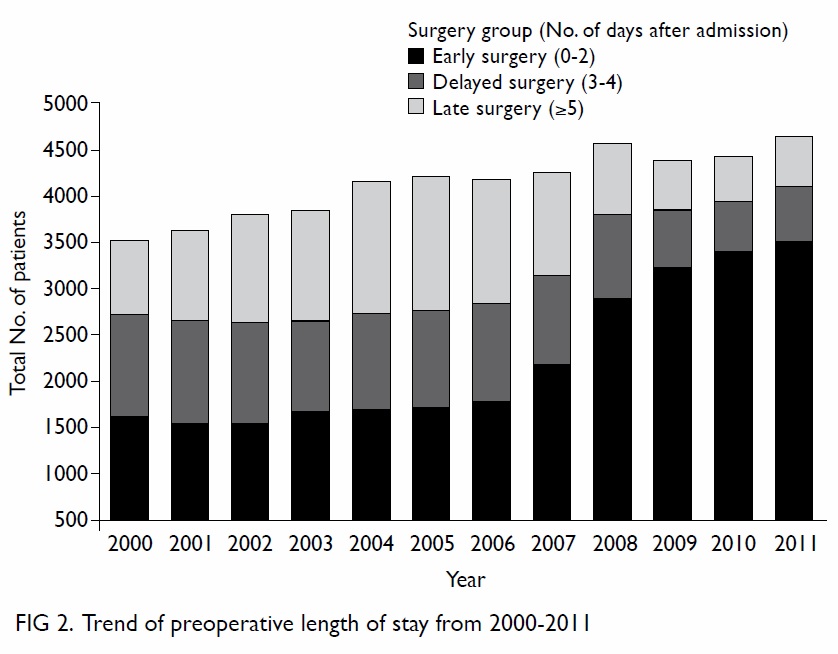
were statistically significant (Table 4). There was also
a gradual reduction in preoperative length of stay of
elderly patients (age range, 65-112 years) with hip
fracture in the post-KPI period (Fig 2).
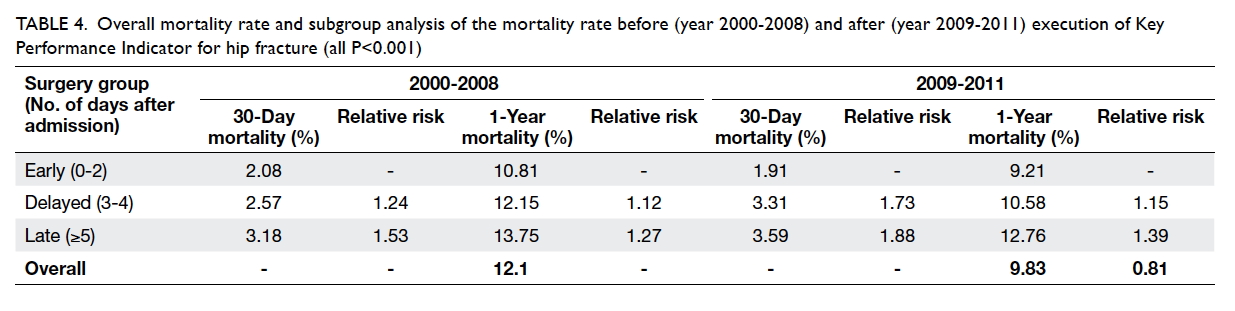
Table 4. Overall mortality rate and subgroup analysis of the mortality rate before (year 2000-2008) and after (year 2009-2011) execution of Key Performance Indicator for hip fracture (all P<0.001)
Discussion
Hip fracture in elderly patients is well known to be
associated with osteoporosis and sarcopenia.9 10 In
an ageing population, it is becoming more important
and places a great burden on our health care system.
Timing of surgery for hip fracture is considered an
important factor in reducing mortality. We therefore
conducted this study to find out their relationship.
To the best of our knowledge, this is the first large
observational study of the association between
timing of surgery and mortality of hip fracture in the
local Chinese elderly population.
Current international guidelines and national model of care for geriatric hip fracture recommend
early surgery to improve the clinical outcome for
elderly patients, including morbidity and mortality.
The Blue Book of the British Orthopaedic Association
in 2007 stated that hip fractures should be operated
on within 48 hours.2 The National Institute for Health
and Care Excellence (NICE) Clinical Guideline (CG 124) from the United Kingdom recommends that
surgery be performed on the day of, or the day after admission, based on the reason that early surgery
within 24 or 48 hours is associated with a lower
mortality risk.3 In Canada, access to surgery should
be no later than 48 hours or 2 days after admission to
the emergency room.4
Hip fracture is associated with high mortality
among the elderly people, with excess mortality compared
with the general population globally.11 Our study
found that longer preoperative stay was associated
with an overall increased 30-day, 1-year, and long-term
mortality in the study population, as shown in
Tables 2 and 3. Other studies have examined short-term
mortality following surgery, with medical co-morbidities
adjusted. Colais et al7 reported that
patients who underwent surgery within 2 days had a
lower 1-year mortality than those in whom surgery
was delayed (HR=0.83; 95% CI, 0.82-0.85). Moja
et al12 performed a meta-analysis of 35 studies and
found that early surgery (<2 days of admission) had
significantly less mortality, with the odds ratio (OR)
being 0.74 (95% CI, 0.67-0.81; P<0.001). In cases
with more than 2 days of delay, the OR for death
in hospital was 1.43 (95% CI, 1.37-1.49) and 30-day
mortality was 1.36 (95% CI, 1.29-1.43).13 Sund and
Liski14 found that delay of more than 2 nights led
to a significant increase in mortality; the HR for
late surgery was 1.18 (95% CI, 1.09-1.28, P<0.0001).
Similar findings were also reported from other
studies. Delay of surgery affected both short-term
and long-term mortality.15 16 17 In our study, the HRs for
delayed surgery and late surgery were 1.16 and 1.37, respectively, similar to other large-scale international
studies.14 16 The longer the delay in surgery, the worse the clinical outcome.
Most studies in the current literature have
focused on short-term mortality following surgery
in patients with hip fracture, but it is known that
mortality in those elderly patients with hip fracture
is high not only in the first year following fracture,
but also remains higher than the general population
during the subsequent 5 years of follow-up in some
studies. Man et al1 reported a 1-year excess mortality
following surgery for geriatric hip fracture of 6.22%
to 23.45%. In our study, the beneficial effects of
early surgery on mortality were not only limited to
the first year after initial fracture, but extended to
later years after the injury based on the calculation
using survival analysis (Fig 1). Our results showed
that the HRs of long-term mortality were 1.16 (95%
CI, 1.13-1.20) and 1.37 (95% CI, 1.33-1.41) when the
delayed group and late group were compared with
the early group, respectively. This significant result
was observed across all age-groups for both genders
(Table 3), despite advancing age and male gender
being associated with increased mortality and
higher excess mortality following hip surgery.1 Thus,
early surgery for hip fracture among elderly patients
is justified to relieve pain, reduce complications,
and improve survival; this echoes our current local
guidelines from the Hospital Authority.4 16 18 19
Key Performance Indicator was a framework
formulated by the Hospital Authority in 2008 and
covered three areas, including Clinical Services,
Human Resources, and Finance. For each area, it
covers a collection of selected indicators. Annual
reviews are conducted by a working group to ensure
the KPIs are in line with the service directions
and priorities of the Hospital Authority. Through
comments and feedback collected from different
sources, the working group reviews the results
and offers suggestions and recommendations for
subsequent service development and resource
allocation, in order to provide the best service
and practices for the general public. With the
implementation of the KPI, hospitals gradually
operated on hip fractures as an emergency or
earlier under the supervision of more experienced
orthopaedic surgeons. In the past, it was not
uncommon for hip fracture surgery to be performed
by junior orthopaedic surgeons in an emergency
setting after office hours. According to the Blue Book
of the British Orthopaedic Association, “all patients
with hip fracture who are medically fit should have
surgery within 48 hours of admission, and during
normal working hours”.2 To correctly interpret
the best practice guideline, timing of surgery is an
important consideration that can improve outcome.
Therefore, emergency daytime surgery under
supervision is preferable. Prior to 2007 the KPI was
approximately 30%, but it had improved to 71.6%
by 2015.20 As a result, length of hospital stay, and
postoperative mortality and morbidity were reduced
in our population.18
Figure 2 shows the gradual reduction in
preoperative length of stay of elderly patients
(age range, 65-112 years) with hip fracture after
implementation of KPI. Lau et al21 identified
preoperative length of stay as one of the most
important factors to affect clinical outcomes of elderly
patients with hip fracture. This was confirmed by our
study. After the introduction of KPI for geriatric hip
fracture, there was a reduced preoperative stay, and
improved survival with reduced 1-year mortality (Table 4). This was likely because patients were able
to mobilise sooner with consequent faster recovery
and rehabilitation. Advances in surgical techniques,
improved perioperative care, and a multidisciplinary
approach allowed high-risk elderly patients to
undergo early surgery.
Since the execution of KPI, the percentage of
medically fit patients operated on early has increased
by approximately 30% to over 70%.5 18 As a result,
the overall 1-year mortality was significantly lower
in the post-KPI group. Our current data reveal that
the KPI was successful in allowing more patients
to have earlier surgery with a consequent better
clinical outcome. Unnecessary delay for surgery was
avoided.
One of the reasons for a delay in surgery was
medical fitness. It is not uncommon for geriatric
patients to be admitted with an acute medical co-morbidity,
such as chest infection. This group
of patients has complex care needs and a higher
risk of morbidity and mortality.11 Surgery is often
delayed due to the need for a medical condition to
be stabilised. We therefore performed a subgroup
analysis of 1-year mortality in patients before
and after KPI. Our results showed that after the
implementation of KPI, the increased relative risk of mortality for
delayed surgery was even more pronounced (Table 4).
A recent retrospective analysis of prospectively
collected data published by Nyholm et al22 revealed
that patients who underwent delayed surgery had
more co-morbidities, and those with a higher
American Society of Anesthesiologists (ASA)
score often waited longer for surgery. One of the
postulated reasons was preoperative optimisation
of their medical condition. Nonetheless they were
able to show an association between surgical delay
and risk of mortality even after adjustment for ASA
score, indicating that there was an increased risk
of mortality with increasing surgical delay, but not
due to decreasing medical fitness of patients with
longer delay times only.23 A systematic review and
meta-analysis by Moja et al12 of 35 retrospective
and prospective studies examined the association
between mortality and delayed surgery in hip
fracture among elderly patients. Meta-analysis of the
primary outcome of overall mortality showed that
early surgery (<2 days of admission) had significantly
less mortality with an OR of 0.74 (95% CI, 0.67-0.81; P<0.001). Meta-analysis of only prospective
studies gave similar results (OR=0.69; 95% CI, 0.57-0.83), and further analysis did not show any effect
of potential confounders such as age or gender.
Despite some intra-study heterogeneity, these
authors concluded that early surgery was associated
with overall lower mortality risk, consistent with the
current recommendation in national guidelines.2 3 4
In order to achieve early preoperative
optimisation, collaboration with orthogeriatricians
is important. The National Hip Fracture Database
annual report in 2015 revealed that 85.3% of people
with hip fracture received orthogeriatric assessment
in the perioperative period. Such service, however,
was not available in all orthopaedic units.23 The NICE
Clinical Guideline (CG 124) recommends early
input from orthogeriatricians in the management of
patients with hip fracture.3 They play a key role in the
integration of initial assessment and perioperative
care as most elderly patients with hip fracture have
co-morbidities. Leung et al24 found that input from
geriatricians in the pre- and post-operative periods
resulted in reduced 1-year mortality (11.5% for
orthogeriatric group vs 20.4% for conventional group;
P=0.02) and improved functional outcome in elderly
patients with hip fracture. In the study of Vidán et
al,25 patients assigned to the geriatric intervention
showed a lower hospital mortality (0.6% vs 5.8%;
P=0.03) and major medical complication rate (45.2%
vs 61.7%; P=0.003) compared with the usual care
group. Similar findings are evident in many other
reports.26 27 28
Orosz et al29 classified reasons of delay in
surgery into patient-related or system-related. Delay
related to stabilisation of medical co-morbidities
may sometimes be inevitable, but operative delay
would undoubtedly have a significant impact on
survival. Based on this observational study, we were
able to conclude that KPI was successful in allowing
more medically fit patients to undergo surgery
without delay and therefore lead to improved
clinical outcomes. Surgery may be delayed in high-risk
patients to enable optimisation of medical
conditions, and involves close collaboration with
orthogeriatricians.
In future studies, further subgroup analysis of
patients with different ASA grade and number of
co-morbidities is warranted so that causes of excess
mortality and high-risk patients can be recognised
and early interventions performed to reduce their
risk. Potential confounding factors should also be
identified as far as possible so they can be controlled
and matched in future studies. The setting up of a
fragility fracture registry would be beneficial for
further studies and analysis.
Limitations
This study has several limitations. First, factors
affecting mortality—for example, pre-injury
mobility status, medical co-morbidities, ASA
grade, functional status, and fracture type—were
not adjusted. It is known that patients with active
medical co-morbidities have higher morbidity
and mortality.15 Medical fitness is one of the major
confounding factors in delayed surgery. Patients
who are medically fit generally undergo surgery
earlier, and those with medical co-morbidities
may be delayed for preoperative assessment and
stabilisation.
Second, a small percentage of geriatric hip
fracture patients who were treated in the private
sector was not included. This, however, would not
have had a large impact on the overall results as
approximately 98% of elderly patients with hip
fracture are managed in public hospitals under
the Hospital Authority. We believe our data are an
accurate reflection of hip fracture cases in Hong
Kong.30
Third, like many database systems for hospital data, deaths out of Hong Kong were not captured, leading to underreported hospital mortality.
Fourth, the current observed association
between early operation and reduced mortality
rate might have been substantially confounded
by improved operative techniques and choice of
implant (eg use of cemented hemiarthroplasties for
relatively younger and medically fit elderly patients
with femoral neck fractures), early involvement
from orthogeriatricians, and improved general
medical care. Undoubtedly all these factors within
the current improved clinical pathway have played
an important role in the improved clinical outcomes
in the later (post-KPI) period of this study.
Lastly, reasons for delay in operation were not
determined in this study.
Conclusion
The present observational study found that KPI
has successfully increased the percentage of
patients undergoing early surgery within 2 days
so as to improve clinical outcome, with one of the
parameters being mortality. Collaboration with
orthogeriatricians will allow early preoperative
optimisation of high-risk patients with medical
co-morbidities. With an expected increase in the
incidence of geriatric hip fracture, good practice of
KPI with early surgery should be offered to these
patients. Guidelines, clinical pathways, and the
setting up of a fragility fracture registry can all play a
significant role in improving our health care system.
Acknowledgements
The authors would like to thank Dr CP Chan for
the statistical analysis, and Mr Tony Kwok and the
Clinical Data Analysis and Reporting System team
of Hospital Authority for their help in data retrieval.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Man LP, Ho AW, Wong SH. Excess mortality for operated
geriatric hip fracture in Hong Kong. Hong Kong Med J
2016;22:6-10. Crossref
2. The care of patients with fragility fracture. British
Orthopaedic Association. September 2007. Available from:
http://www.fractures.com/pdf/BOA-BGS-Blue-Book.pdf.
Accessed Jun 2016.
3. Hip fracture: management. Clinical guideline. National
Institute for Health and Care Excellence (NICE). 22 June 2011. Available from: https://www.nice.org.uk/guidance/cg124. Accessed Jun 2016.
4. Bone and Joint Decade
Canada. National hip fracture toolkit. June 30 2011. Available from: http://boneandjointcanada.com/wp-content/uploads/2014/05/National-hip-fracture-toolkit-June-2011.pdf. Accessed Jun
2016.
5. Report of the chairman. COC in orthopaedics and
traumatology. Hong Kong: Hospital Authority; 2009.
6. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with
increased mortality of hip fracture patients? Systematic
review, meta-analysis, and meta-regression. Can J Anaesth
2008;55:146-54. Crossref
7. Colais P, Di Martino M, Fusco D, Perucci CA, Davoli M.
The effect of early surgery after hip fracture on 1-year
mortality. BMC Geriatr 2015;15:141. Crossref
8. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G,
Frankel VH. Postoperative complications and mortality
associated with operative delay in older patients who have
a fracture of the hip. J Bone Joint Surg Am 1995;77:1551-6. Crossref
9. Tsang SW, Kung AW, Kanis JA, Johansson H, Oden A.
Ten-year fracture probability in Hong Kong Southern
Chinese according to age and BMD femoral neck T-scores.
Osteoporos Int 2009;20:1939-45. Crossref
10. Ho AW, Lee MM, Chan EW, et al. Prevalence of pre-sarcopenia
and sarcopenia in Hong Kong Chinese geriatric
patients with hip fracture and its correlation with different
factors. Hong Kong Med J 2016;22:23-9.
11. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality
after hip fracture: is delay before surgery important? J Bone
Joint Surg Am 2005;87:483-9. Crossref
12. Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip
fracture surgery: patients operated within 48 hours have
better outcomes. A meta-analysis and meta-regression of
over 190,000 patients. PLoS One 2012;7:e46175. Crossref
13. Bottle A, Aylin P. Mortality associated with delay in
operation after hip fracture: observational study. BMJ
2006;332:947-51. Crossref
14. Sund R, Liski A. Quality effects of operative delay on
mortality in hip fracture treatment. Qual Saf Health Care
2005;14:371-7. Crossref
15. Casaletto JA, Gatt R. Post-operative mortality related to
waiting time for hip fracture surgery. Injury 2004;35:114-20. Crossref
16. Novack V, Jotkowitz A, Etzion O, Porath A. Does delay
in surgery after hip fracture lead to worse outcomes? A
multicenter survey. Int J Qual Health Care 2007;19:170-6. Crossref
17. Zuckerman JD. Hip fracture. N Engl J Med 1996;334:1519-25. Crossref
18. Lau PY. To improve the quality of life in elderly people with
fragility fractures. Hong Kong Med J 2016;22:4-5.
19. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early
surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 2010;182:1609-16. Crossref
20. Chief Executive’s Progress Report on Key Performance
Indicators (KPI Report No. 29, December 2015). Available from: https://www.ha.org.hk/haho/ho/cad_bnc/AOM-P1169.pdf. Accessed
Sep 2016.
21. Lau TW, Fang C, Leung F. The effectiveness of a geriatric
hip fracture clinical pathway in reducing hospital and
rehabilitation length of stay and improving short-term
mortality rates. Geriatr Orthop Surg Rehabil 2013;4:3-9. Crossref
22. Nyholm AM, Gromov K, Palm H, et al. Time to surgery is
associated with thirty-day and ninety-day mortality after
proximal femoral fracture: a retrospective observational
study on prospectively collected data from the Danish
fracture database collaborators. J Bone Joint Surg Am
2015;97:1333-9. Crossref
23. Royal
College of Physicians. National Hip Fracture Database annual report 2015. Available from:
http://www.nhfd.co.uk/nhfd/nhfd2015reportPR1.pdf.
Accessed Jun 2016.
24. Leung AH, Lam TP, Cheung WH, et al. An orthogeriatric
collaborative intervention program for fragility fractures: a
retrospective cohort study. J Trauma 2011;71:1390-4. Crossref
25. Vidán M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy
of a comprehensive geriatric intervention in older patients
hospitalized for hip fracture: a randomized, controlled
trial. J Am Geriatr Soc 2005;53:1476-82. Crossref
26. Friedman SM, Mendelson DA, Kates SL, McCann RM.
Geriatric co-management of proximal femur fractures:
total quality management and protocol-driven care result
in better outcomes for a frail patient population. J Am
Geriatr Soc 2008;56:1349-56. Crossref
27. Thwaites JH, Mann F, Gilchrist N, Frampton C, Rothwell
A, Sainsbury R. Shared care between geriatricians and
orthopaedic surgeons as a model of care for older patients
with hip fractures. N Z Med J 2005;118:U1438.
28. Ho AW, Wong SH. Orthogeriatric collaborative intervention
program for hip fracture surgery: A review on southern
Chinese population. Osteoporos Int 2016;27(Supp 1):P400.
29. Orosz GM, Hannan EL, Magaziner J, et al. Hip fracture in
the older patient: reasons for delay in hospitalization and
timing of surgical repair. J Am Geriatr Soc 2002;50:1336-40. Crossref
30. Chau PH, Wong M, Lee A, Ling M, Woo J. Trends in hip
fracture incidence and mortality in Chinese population
from Hong Kong 2001-09. Age Ageing 2013;42:229-33. Crossref