Hong Kong Med J 2017 Aug;23(4):326–32 | Epub 23 Jun 2017
DOI: 10.12809/hkmj176267
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Triplet pregnancy with fetal reduction:
experience in Hong Kong
WT Tse, MB, ChB, MRCOG; LW Law, MB, ChB, MRCOG; Daljit S Sahota, PhD; TY Leung, MD, FRCOG; Yvonne KY Cheng, MB, ChB, MRCOG
Department of Obstetrics and Gynaecology, The Chinese University of
Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr Yvonne KY Cheng (yvonnecheng@cuhk.edu.hk)
 A video clip showing triplet pregnancy with fetal reduction skills
A video clip showing triplet pregnancy with fetal reduction skillsAbstract
Introduction: Triplet and higher-order multiple
pregnancies are well known to be associated with
increased adverse outcomes. This study reviewed
the perinatal outcomes in women with a triplet
pregnancy who underwent fetal reduction versus
expectant management at a university hospital in
Hong Kong.
Methods: This was a retrospective review of triplet
pregnancies at Prince of Wales Hospital in Hong
Kong from 1 January 2008 to 30 September 2014.
Women carrying a triplet pregnancy were classified
as having had expectant management, fetal reduction
to twins, or fetal reduction to a singleton. Maternal
and pregnancy characteristics were compared.
Outcome measures included fetal loss, gestational
age at delivery, birth weight, neonatal survival rate,
neonatal death, neonatal complications, and need
for and length of neonatal intensive care unit stay.
Results: A total of 52 triplet pregnancies were
identified. One pregnancy that was lost to follow-up
and one that was terminated were excluded. The
majority of pregnancies (84%) were the result of
assisted reproductive technology. Fetal reduction
was performed in 26 (52%) pregnancies, of which 22
were reduced to twins and four to a singleton. The
mean gestations at delivery were 32.6, 35.2, and 39.6
weeks in the expectant management, fetal reduction to twins, and fetal reduction to a singleton groups,
respectively. Significantly more pregnancies with
expectant management resulted in a preterm birth.
All pregnancies with fetal reduction to a singleton
resulted in a term birth. A higher mean birth weight,
lower neonatal death rate, and reduced need for
admission to and length of stay in the neonatal
intensive care unit were observed in the fetal
reduction groups.
Conclusions: Approximately 50% of women
with a triplet pregnancy in Hong Kong elected to
undergo fetal reduction. This was associated with
a significant reduction in extreme preterm delivery
and associated morbidity and mortality.
New knowledge added by this study
- This is the first study of fetal reduction in triplet pregnancy in Hong Kong.
- About half of women with a triplet pregnancy in Hong Kong would elect to undergo fetal reduction.
- Fetal reduction can significantly prolong the gestation at delivery and significantly reduce preterm delivery to <32 weeks.
- Women with a triplet pregnancy should be adequately counselled on the benefits and risks of fetal reduction to allow them to make an informed decision.
Introduction
The recent increasing availability and popularity
of assisted reproductive technology (ART) has
resulted in an increase in the incidence of multiple
pregnancies.1 In the United States, the incidence of
triplet pregnancies has increased two- to three-fold
since the early 1980s.2 In Hong Kong, there was a
2.3-fold increase in ART procedures from 2009 to
2015, reaching over 11 000 procedures per year.3
The Council on Human Reproductive Technology of Hong Kong issued the Code of Practice on
Reproductive Technology & Embryo Research in
2013 and limited the number of embryos transferred
per cycle to three. Despite this recommendation,
there has been no drop in the number of multiple
pregnancies following ART, and the rate has
remained at 6% since 2010.3 Thus multiple pregnancy
is still a major obstetric concern in Hong Kong.
Triplet and higher-order multiple pregnancies
are well known to be associated with increased adverse outcomes including maternal medical
complications, pregnancy loss, intrauterine
growth restriction, and preterm delivery. Triplet
pregnancies have a four-fold increased risk of birth of
<29 weeks compared with twin pregnancies.4 This is
of particular concern as it significantly increases the
perinatal morbidity and mortality due to prematurity.
The risk of infant death in triplets is 3 times higher
than that in twins.4
Reduction of triplets or higher-order multiple
pregnancies has been performed since the 1980s.
A meta-analysis of the early prospective non-randomised
studies suggested that reduction of
triplet pregnancies was associated with a reduction
in maternal and fetal adverse outcomes.5 More
importantly, the rate of early premature delivery
(<32 weeks) can significantly be reduced following
fetal reduction (FR), from 26%-33% to 5.5% for
FR to a singleton and 10%-17% for FR to twins.6 7 8
Nonetheless, it is associated with procedure-related
pregnancy loss in 4.5%-9.6% of cases when performed
by fetal intracardiac injection of potassium chloride
(KCl), and 8.8%-15% for cord coagulation.8 9
10 11
The objective of this study was to compare the
perinatal outcomes for triplet pregnancy with and
without FR at a university hospital in Hong Kong.
Methods
This was a retrospective cohort study conducted
at Prince of Wales Hospital, Hong Kong. Triplet pregnancies with an expected date of confinement
from 1 January 2008 to 30 September 2014 were retrieved
from the prenatal diagnostic unit database and the
Specialty Clinical Information System database.
Demographics, and pregnancy and perinatal
outcomes were reviewed. The data retrieval and
review were performed by the first author, a medical
officer from the department, who was not blinded
to the study hypothesis. Women who carried a
triplet pregnancy were classified into three groups: expectant management, FR to twins, or FR to a
singleton.
Chorionicity and amnionicity were assessed
during the first trimester by ultrasound. Women with
a triplet pregnancy were offered counselling about
the benefits and risks of expectant management
versus FR to twins or a singleton. Specifically, women
were counselled that approximately one third of
triplet pregnancies resulted in preterm birth before
32 weeks of gestation. The aim of FR was primarily
to reduce the risk of early preterm birth. Such risk
can be reduced to 10%-18% following FR to twins
and to 5%-8% if reduced to a singleton, although
the procedure associated with a miscarriage rate
of 5%-15%, depending on the method used.6 7 8 9
10 11 Ultimately, the decision for FR to twins or a
singleton was dictated first by the mother’s wishes
and second by whether FR was technically feasible.
All procedures were performed in accordance with
the Offences Against the Person Ordinance. The
FR procedures carried out at the Prince of Wales
Hospital were performed under real-time ultrasound
guidance by Maternal and Fetal Medicine (MFM)
specialists or supervised trainees. Some procedures
were performed in the private sector. Choice of
fetus(es) to be reduced depended on the presence
of fetal abnormalities, placental location, and
technical feasibility. Fetal gender was not revealed
to the parents to avoid gender selection. Fetal
intracardiac KCl injection was performed in fetuses
with a separate placenta, that is, in trichorionic
triamniotic (TCTA) triplets or when feticide was
performed in both monochorionic fetuses of a
dichorionic triamniotic (DCTA) pregnancy. A 20G
needle was inserted transabdominally into the fetal
heart and 1-5 mL of 14.9% KCl injected until fetal
asystole was observed. Bipolar cord coagulation
(BPC) or radiofrequency ablation (RFA) of the
umbilical cord was performed in monochorionic
fetuses in DCTA or monochorionic triamniotic
(MCTA) triplets. In BPC, a 2-mm or 3-mm bipolar
forceps was inserted transabdominally through a
3.9-mm trocar (Karl Storz, Tuttlingen, Germany)
and the umbilical cord was grasped. Electrocautery
was performed at a power setting of 20-60 W for a
duration of 30-60 seconds. Two to three adjacent
sites on the cord were cauterised. Cessation of blood
flow through the umbilical cord was confirmed by
colour and/or pulsed wave Doppler. In RFA, the
radiofrequency needle (LaVeen SuperSlim Needle
Electrode radiofrequency probe, 17G, 15 cm long;
Massachusetts, United States) was inserted percutaneously
into the fetal abdomen at the site of cord insertion.
The prongs of the device were deployed and
radiofrequency energy was applied in a stepwise
fashion starting from 30 W and progressing to a
maximum of 100 W; each energy level lasted no
more than 2 minutes. Energy was applied until no
blood flow was observed in the umbilical cord by
colour and pulsed wave Doppler and a terminal fetal
bradycardia was detected.
Women were discharged within 24 hours of
the procedure, and were followed up 1 week later
to confirm viability of the remaining fetus(es).
Women who carried triplets and elected expectant
management underwent elective caesarean delivery
at 34 weeks. Monochorionic twins were delivered
at 37 weeks and dichorionic twins at 38 weeks.
Earlier delivery was indicated if there were maternal
or fetal complications. The pregnancy outcomes
studied included any pregnancy loss, gestational
age at delivery, birth weight, neonatal survival
rate, neonatal death, and neonatal complications:
respiratory distress syndrome, chronic lung
disease, intraventricular haemorrhage, necrotising
enterocolitis, retinopathy of prematurity, neonatal
sepsis, need for neonatal intensive care unit (NICU)
care, and median length of NICU stay.
Ethics approval was obtained from the
Institutional Review Board (CREC Ref No: 2016.697)
with informed consent waived. The SPSS (Windows
version 21.0; IBM Corp, Armonk [NY], US) was used
for statistical analysis. Fisher’s exact test was used for
categorical data, and Student’s t test for comparing
the means between the expectant management
and FR groups. A P value of <0.05 was taken as
statistically significant.
Results
There were 52 triplet pregnancies during the study
period. Two cases were excluded from analysis as
one was lost to follow-up after 13 weeks of gestation,
and the other had a termination of pregnancy
(TOP) at 8 weeks for social reasons. Of the included
pregnancies, 84% (42/50) were the result of an ART
procedure, of which 14 resulted from ovulation
induction and 28 from in-vitro fertilisation. Among
those conceived by ovulation induction, seven also
included intrauterine insemination. In these 42
pregnancies conceived by ART, 33 (78.6%) were
TCTA, eight (19.0%) were DCTA, and one (2.4%) was
MCTA.
In the 50 cases included in the analysis,
26 (52.0%) pregnancies underwent FR and the
remaining 24 (48.0%) had expectant management.
Of the 26 cases of FR, 22 (84.6%) were reduced
from triplets to twins and four (15.4%) from triplets
to a singleton. Two of the pregnant women in the
expectant management group elected FR, however,
this could not be done due to technical difficulties
and so they were managed conservatively. All except
three FR procedures were performed at the Prince
of Wales Hospital between 10 and 13 weeks of
gestation. The three cases of FR performed in the
private sector had fetal intracardiac KCl injection
between 7 and 9 weeks of gestation.
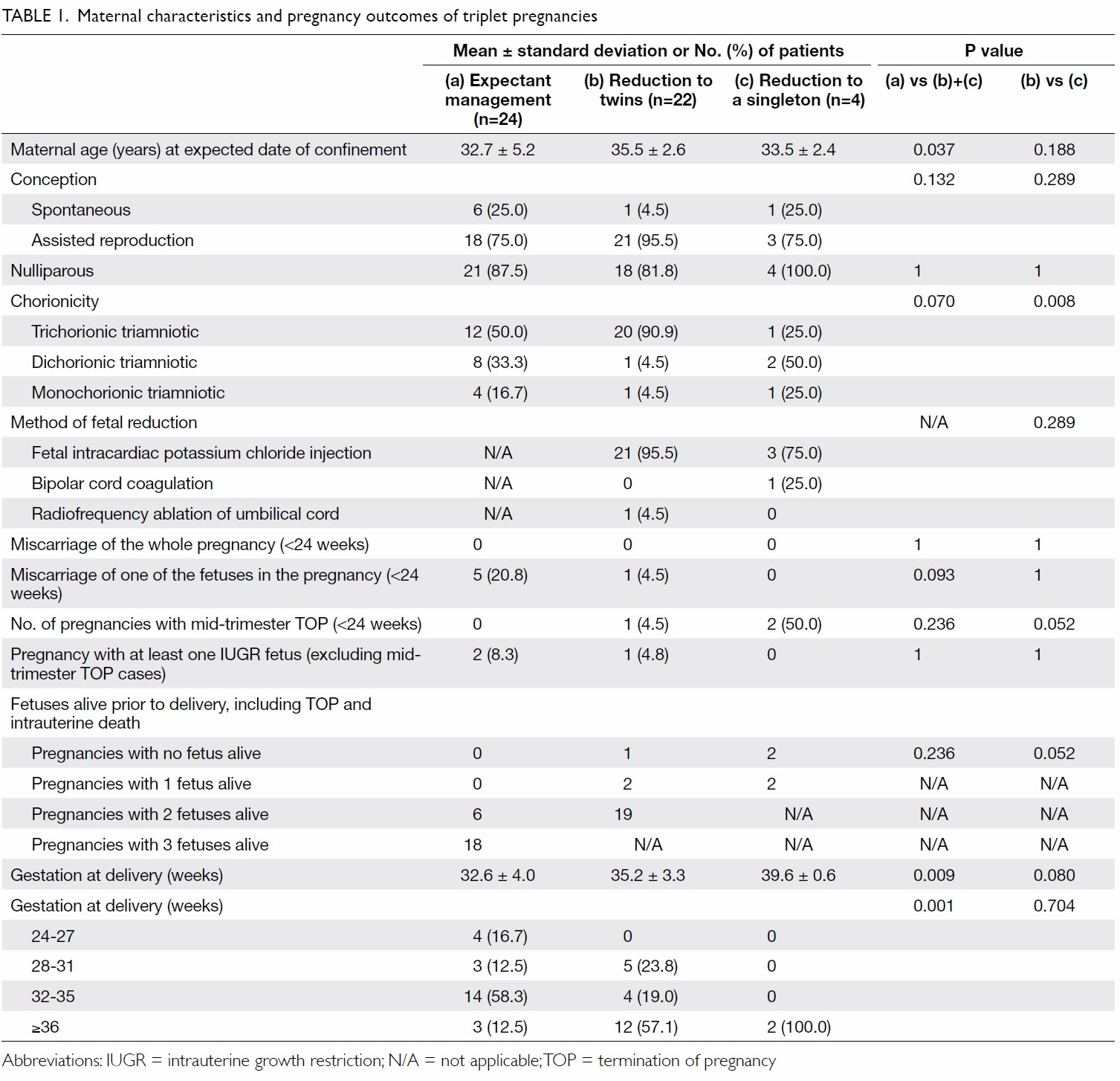
Maternal characteristics and pregnancy
outcomes are shown in Table 1. Women who
underwent FR were 1 to 2 years older than those
who elected expectant management. Parity, method
of conception, chorionicity, and method of feticide
between the three groups were similar. There was
no miscarriage of the whole pregnancy in any of
the three groups although five pregnancies that
were managed expectantly had spontaneous fetal
loss of one of the fetuses, and one pregnancy with
FR to twins miscarried one twin following FR. The
numbers of spontaneous fetal losses before 24 weeks
(ie miscarriage rate) were 6.9% (5/72) and 2.1% (1/48)
in the expectant management group and FR group,
respectively, and there was no statistical significance
between the two groups. There were three cases of
preterm rupture of membranes (ROM) following FR
and in all three cases the parents elected TOP. One
woman had fetal intracardiac KCl injection to reduce
a TCTA triplet pregnancy to twins at 11 weeks, but
ROM occurred at 15 weeks of gestation. In the other
two cases where feticide was performed to reduce the
triplets to a singleton, one was a case of MCTA triplets
reduced to a singleton with BPC of two fetuses at 13
weeks, and the other was TCTA triplets reduced
to a singleton by fetal intracardiac KCl injection in
two fetuses at 11 weeks of gestation. For these two
cases, ROM occurred at 1 day and 11 weeks after
FR, respectively. There were only two cases of cord
coagulation in this study. Apart from the case of BPC
in MCTA triplets that resulted in ROM, the other
case was also MCTA triplets with RFA performed at
12 weeks for FR to twin pregnancy. The procedure
was uncomplicated and the twins were subsequently
delivered at 35 weeks of gestation. The gestational age
at delivery was significantly higher in the FR groups.
The mean gestation at delivery was 32.6 weeks in
the expectant management group versus 35.2 and
39.6 weeks in the FR to two fetuses and one fetus,
respectively. The risk of extreme preterm delivery was
also significantly lower in those with FR (P=0.001).
In women with expectant management, 16.7% had
extreme preterm delivery of <28 weeks, and 29.2%
delivered before 32 weeks. In women with FR to two
fetuses, there was no case of extreme preterm delivery
of <28 weeks, and 23.8% delivered before 32 weeks.
All pregnancies with FR to a singleton had term
birth. None of the pregnancies was complicated by
twin-to-twin transfusion syndrome and intrauterine
growth restriction occurred in only two and one
pregnancies in the expectant management and FR to
twins groups, respectively.
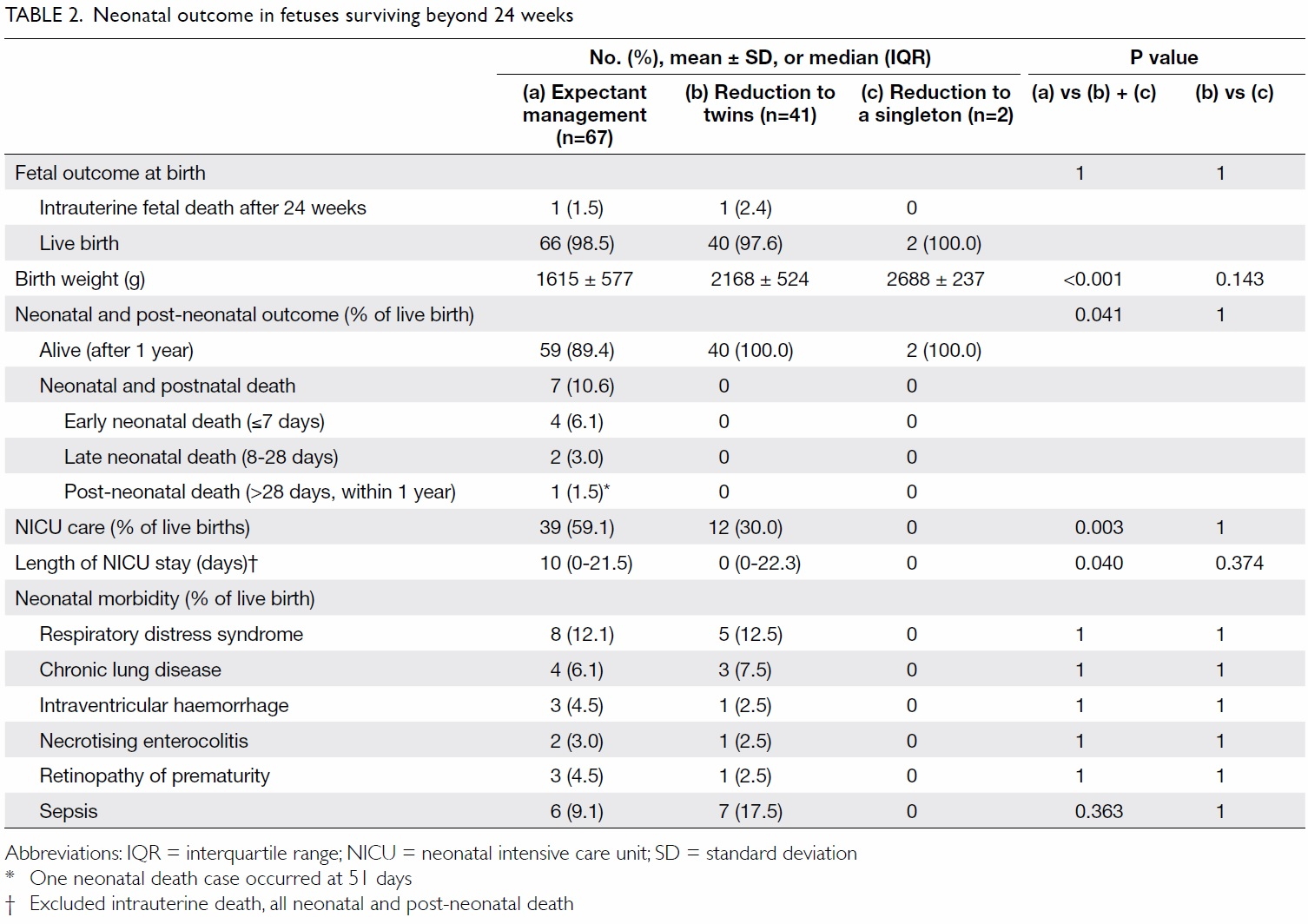
The neonatal outcome of the fetuses who
survived beyond 24 weeks are reported in Table 2.
There were two intrauterine fetal deaths, one in the
expectant management group and one in the FR to
twins group. All seven neonatal and post-neonatal
deaths occurred in the expectant management
group. These infants were all delivered <25 weeks and died of complications of prematurity. The
mean birth weights in the FR groups to twins and
a singleton were 553 g and 1073 g higher than that
in the expectant management group, respectively.
The need for NICU care (P=0.003) and length of
NICU stay (P=0.040) were significantly higher in the
expectant management group with no FR. Neonatal
morbidities including respiratory distress syndrome,
chronic lung disease, intraventricular haemorrhage,
necrotising enterocolitis, retinopathy of prematurity,
and neonatal sepsis were not statistically significant
between the groups.
Discussion
Multiple pregnancy is an increasingly important
problem in obstetric practice as a result of the
success of fertility procedures. Their incidence is
expected to continue to rise as fertility services both
in Hong Kong and in other nearby countries such as
Taiwan, Thailand, and Mainland China become more
accessible and affordable. As shown in our cohort,
over 80% of triplet pregnancies were conceived by
ART. This is the first study of the outcomes of triplet
pregnancies following FR in Hong Kong. Of note, FR
may not be acceptable to all parents, and parental
choice has a strong influence on decisions about
intervention. To make the best informed choice,
parents should be counselled adequately on the
benefits and risks of expectant management versus
FR. The provision of local data on perinatal outcomes
following FR is an essential part of that counselling.
The primary aim of FR is to reduce neonatal
morbidity consequent to prematurity. Our results
show that FR in a triplet pregnancy has the benefit
of increasing the gestation at delivery and reducing
the risk of extreme preterm delivery earlier than 32 and 28 weeks. The mean gestation at delivery was
32.6 weeks in the expectant management group
versus 35.2 and 39.6 weeks in the FR to two fetuses
and one fetus, respectively. This indicates that the
performance of FR in Hong Kong is comparable with
that reported in the literature and our results reaffirm
previously reported data in which FR in triplet
pregnancies to twins can prolong the pregnancy by
approximately 3 weeks.12 In women with expectant
management, 16.7% and 29.2% had extreme preterm
delivery before 28 weeks and 32 weeks, respectively.
In women with FR to two fetuses, there was no
extreme preterm delivery of <28 weeks, and 23.8%
delivered before 32 weeks. The risk of preterm
delivery earlier than 32-33 weeks following FR has
been reported to be between 24% and 37%,7 13 14 15 which are comparable to our results. All women
with FR to one fetus had term deliveries. Despite
the prolongation of pregnancy, however, the overall
survival following FR was not significantly different
to that following expectant management (Table 1).
In fact, studies of FR in triplet pregnancies have not
shown an increase in perinatal survival.12 13
Prolongation of pregnancy in the FR group
leads to improvement in a number of outcomes. The
FR group had a significantly higher birth weight. The
need for NICU care and length of NICU stay were
significantly lower. The seven neonatal deaths in
our cohort were all of neonates from the expectant
management group who were delivered <25 weeks
and died of complications of prematurity. We were,
however, unable to show a difference in neonatal
morbidity due to the small numbers in each group.
The rates of spontaneous loss of the whole
pregnancy in reduced versus non-reduced triplets
have previously been reported to be 8.1% and 4.4%,
respectively,7 although such loss rate can be reduced
with increasing experience so that it is comparable
with that in non-reduced triplets.6 10 11 In our study,
there was no spontaneous total pregnancy loss.
This may be because all procedures were carried
out by MFM specialists or trainees with expertise in
invasive fetal procedures. There were fetal losses in
both the expectant management and FR groups, but
it was not statistically significant. Three cases had
prelabour ROM after FR, and these parents elected
TOP due to poor prognosis. Most studies of FR report
a procedure-related pregnancy loss or miscarriage
rate,6 7 8 10 11 but there are no data for the rate of
prelabour ROM after FR in triplet pregnancies. In
complicated monochorionic pregnancies, the rate of
prelabour ROM following cord coagulation has been
reported to be 20% to 30%.9 16 17 On the contrary, the
prelabour ROM rate was 12% after fetal intracardiac
KCl injection in multichorionic pregnancies.18
This study found that only maternal age
influenced a decision to undergo FR but this is
contrary to the findings of other studies.7 13 19 A
possible explanation is that in women with advanced
age, multiple pregnancy will add additional maternal
risks during the pregnancy and may influence a
decision to undergo FR. When choosing FR to
twins or a singleton, our results showed that the
chorionicity of the triplet pregnancies most likely
affected their choice: 64% (21/33) of those with TCTA
triplets chose to have FR although 95% (20/21) opted
for reduction to twins. In DCTA and MCTA triplets,
only 27% and 33% proceeded to FR, respectively.
As our study only had two cases of RFA or BPC
performed in MCTA triplets, we cannot conclude
any reason for a low rate of FR by cord coagulation. It
is, however, possible that women believed there was
a higher risk of miscarriage associated with RFA or
BPC.
It must be emphasised that in women who
choose to reduce one fetus in a DCTA pregnancy,
the best option is to reduce one fetus in the
monochorionic pair, not the fetus with a separate
placenta, by fetal intracardiac KCl injection.
Although the latter is technically easier, there would
be continued risks of twin-to-twin transfusion syndrome or twin anaemia polycythaemia sequence
when the singleton fetus is reduced to keep the
monochorionic twins, and this poses significant
risks to the pregnancy. The miscarriage risk before
24 weeks following FR of the fetus with a separate
placenta has been reported to be as high as 23.5%.8
Therefore, women who elect to have FR of DCTA
triplets to twins should be referred to a tertiary
unit with expertise in FR and where more advanced
techniques are readily available. Nevertheless, the
best perinatal outcome in any type of triplets will
be achieved by reducing two fetuses resulting in
a singleton pregnancy.8 Women along with their
partner should be aware of this and be adequately
counselled so that they may make an informed
decision.
This is the first study of FR in triplet pregnancy
in Hong Kong. It provides valuable data on the local
experience in FR that is useful in parental counselling.
The strength of this study is that comprehensive
perinatal outcomes were obtained in all pregnancies
except two.
This study has limitations. First, the number of
cases included was small, although we believe this is
the largest cohort possible to be reported in Hong
Kong as our hospital has the highest number of
deliveries and receives referrals for FR from private
obstetricians and other obstetric units in Hong Kong.
Second, the number of cord coagulation procedures
was limited, and no further analysis was possible
to determine which cord coagulation procedure is
superior.
Conclusions
Approximately 50% of women with a triplet
pregnancy in Hong Kong elected to undergo FR,
which can significantly prolong the gestation at
delivery and significantly reduce preterm delivery
of <32 weeks, although it is associated with risk
of miscarriage and complications such as ROM.
Women carrying a triplet pregnancy should be
adequately counselled about the benefits and risks
of FR so that they can make an informed decision.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Pison G, Monden C, Smits J. Twinning rates in developed
countries: trends and explanations. Popul Dev Rev
2015;41:629-49. Crossref
2. Martin JA, Osterman MJ, Thoma ME. Declines in triplet
and higher-order multiple births in the United States,
1998-2014. NCHS Data Brief 2016;(243):1-8.
3. Council on Human Reproductive Technology, Hong Kong.
Code of practice on reproductive technology & embryo
research. Available from: http://www.chrt.org.hk/english/service/service_cod.html. Accessed 26 Jan 2017.
4. Luke B, Brown MB. Maternal morbidity and infant death
in twin vs triplet and quadruplet pregnancies. Am J Obstet
Gynecol 2008;198:401.e1-10. Crossref
5. Dodd J, Crowther C. Multifetal pregnancy reduction of
triplet and higher-order multiple pregnancies to twins.
Fertil Steril 2004;81:1420-2. Crossref
6. Evans MI, Berkowitz RL, Wapner RJ, et al. Improvement in
outcomes of multifetal pregnancy reduction with increased
experience. Am J Obstet Gynecol 2001;184:97-103. Crossref
7. Papageorghiou AT, Avgidou K, Bakoulas V, Sebire NJ,
Nicolaides KH. Risks of miscarriage and early preterm
birth in trichorionic triplet pregnancies with embryo
reduction versus expectant management: new data and
systematic review. Hum Reprod 2006;21:1912-7. Crossref
8. Morlando M, Ferrara L, D’Antonio F, et al. Dichorionic
triplet pregnancies: risk of miscarriage and severe
preterm delivery with fetal reduction versus expectant
management. Outcomes of a cohort study and systematic
review. BJOG 2015;122:1053-60. Crossref
9. Rossi AC, D’Addario V. Umbilical cord occlusion for
selective feticide in complicated monochorionic twins:
a systematic review of literature. Am J Obstet Gynecol
2009;200:123-9. Crossref
10. Stone J, Eddleman K, Lynch L, Berkowitz RL. A single
center experience with 1000 consecutive cases of multifetal
pregnancy reduction. Am J Obstet Gynecol 2002;187:1163-7. Crossref
11. Stone J, Ferrara L, Kamrath J, et al. Contemporary
outcomes with the latest 1000 cases of multifetal pregnancy
reduction (MPR). Am J Obstet Gynecol 2008;199:406.e1-4. Crossref
12. van de Mheen L, Everwijn SM, Knapen MF, et al. The
effectiveness of multifetal pregnancy reduction in trichorionic triplet gestation. Am J Obstet Gynecol
2014;211:536.e1-6. Crossref
13. Chaveeva P, Kosinski P, Puglia D, Poon LC, Nicolaides KH.
Trichorionic and dichorionic triplet pregnancies at 10-14
weeks: outcome after embryo reduction compared to
expectant management. Fetal Diagn Ther 2013;34:199-205. Crossref
14. Wimalasundera RC. Selective reduction and termination
of multiple pregnancies. Semin Fetal Neonatal Med
2010;15:327-35. Crossref
15. Antsaklis A, Souka AP, Daskalakis G, et al. Embryo
reduction versus expectant management in triplet
pregnancies. J Matern Fetal Neonatal Med 2004;16:219-22. Crossref
16. Bebbington MW, Danzer E, Moldenhauer J, Khalek
N, Johnson MP. Radiofrequency ablation vs bipolar
umbilical cord coagulation in the management of complicated
monochorionic pregnancies. Ultrasound Obstet Gynecol
2012;40:319-24. Crossref
17. van den Bos EM, van Klink JM, Middeldorp JM, Klumper
FJ, Oepkes D, Lopriore E. Perinatal outcome after selective
feticide in monochorionic twin pregnancies. Ultrasound
Obstet Gynecol 2013;41:653-8. Crossref
18. Mohammed AB, Farid I, Ahmed B, Ghany EA. Obstetric
and neonatal outcome of multifetal pregnancy reduction.
Middle East Fertil Soc J 2015;20:176-81. Crossref
19. Boulot P, Vignal J, Vergnes C, Dechaud H, Faure JM, Hedon
B. Multifetal reduction of triplets to twins: a prospective
comparison of pregnancy outcome. Hum Reprod
2000;15:1619-23. Crossref