DOI: 10.12809/hkmj166110
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
The feeding paradox in advanced dementia: a
local perspective
James KH Luk, FHKCP, FHKAM (Medicine)1;
Felix HW Chan, FHKCP, FHKAM (Medicine)1; Elsie Hui,
FHKCP, FHKAM (Medicine)2; CY Tse, FHKCCM, FHKAM
(Medicine)3
1 Department
of Medicine and Geriatrics, Fung Yiu King Hospital, Pokfulam, Hong Kong
2 Department
of Medicine and Geriatrics, Shatin Hospital, Shatin, Hong Kong
3 Hospital Authority Clinical Ethics Committee, Hospital
Authority, Hong Kong
Corresponding author: Dr James KH
Luk (lukkh@ha.org.hk)
Abstract
Feeding problems are common in older people with
advanced dementia. When eating difficulties arise tube feeding is often
initiated, unless there is a valid advance directive that refuses enteral
feeding. Tube feeding has many pitfalls and complications. To date, no
benefits in terms of survival, nutrition, or prevention of aspiration
pneumonia have been demonstrated. Careful hand feeding is an alternative to
tube feeding with advanced dementia. In Hong Kong, the Hospital Authority
has established clear ethical guidelines for careful hand feeding.
Notwithstanding, there are many practical issues locally if tube feeding is
not used in older patients with advanced dementia. Training of doctors,
nurses, and other members of the health care team is vital to the
promulgation of careful hand feeding. Support from the government and
Hospital Authority policy, health care staff training, public education, and
promotion of advance care planning and advance directive are essential to
reduce the reliance on tube feeding in advanced dementia.
Introduction
Hong Kong is facing an unparalleled challenge of rapid
population ageing.1 This demographic change results in an
impending need for end-of-life care among older people with advanced
dementia.2 One of the natural stages of the dementia
disease process is eating problems with poor appetite and swallowing
difficulty, leading to malnutrition, weight loss, and aspiration pneumonia
(AP).3 4 Unless there is a valid advance
directive (AD) refusing enteral feeding, family members and the health care
team often feel compelled to initiate tube feeding. This leads to a very
high prevalence of tube feeding in elderly with advanced dementia,
especially those living in residential care homes for the elderly (RCHEs).5
6
Pitfalls of tube feeding
There are many reasons for placing a feeding tube in
patients with advanced dementia. Medical, social, cultural, economic,
ethical, psychological, and medicolegal factors all play a part in the
decision.7 Many older patients are commenced on tube
feeding when they are dysphagic or are feeding inadequately. Probably due to
inadequate information about the pitfalls of tube feeding, risk of AP and
survival are the most frequently cited reasons by health care teams to
insert a feeding tube.8 To date, however, evidence has
proven that tube feeding does not prevent AP.9 On the
contrary, AP might be increased by the use of enteral feeding.10
Placement of a nasogastric tube weakens the lower oesophageal sphincter and
reduces the efficiency of the valve that prevents gastric reflux into the
upper digestive tract.11 The use of tube feeding without
oral feeding also leads to neglect of oral hygiene, resulting in bacterial
colonisation and an increased risk of AP. Enteral feeding is unable to
improve serum albumin, body weight, or lean muscle mass.12
The use of a feeding tube causes patient discomfort, increased use of
restraints, and consequent greater likelihood of pressure sore development.13
14 Studies showed that RCHE residents with feeding tubes
are frequently transferred to an emergency department for tube complications
such as blockage and dislodgement.15 To date, studies
have not shown survival benefits in older people with tube feeding.16
In a local study of 312 advanced cognitively impaired RCHE residents, 164
(53%) were being tube fed.6 The 1-year mortality rate was
34% and enteral feeding was cited as an important risk factor for 1-year
mortality (odds ratio=2.0; 95% confidence interval, 2.0-3.4; P=0.008).6
Careful hand feeding as an alternative
Careful hand feeding (CHF) has been advocated as an
alternative for older people with advanced dementia and eating problems.17
In CHF, the carer makes use of feeding techniques such as frequent
reminders to swallow, multiple swallows, encouraging gentle coughs after each
swallow, limiting bolus size to less than one teaspoon, and judicious use of
thickeners. The carer observes the patient for choking and pocketing of food
in the mouth. The carer focuses on the older person during the entire
feeding process and avoids distraction. The older person is placed in an
upright position during the meal. Moistening foods with water or sauces, or
alternating food with appropriate liquid consistency may help swallowing,
for example, in patients with a dry mouth.
In the 2014 position statement on feeding
tubes in advanced dementia published by the
American Geriatrics Society, feeding tubes are not
recommended.18 It emphasises that CHF should be
offered as it is at least as good as tube feeding for
the outcomes of death, AP, functional status, and
comfort.19 20 Older patients with dementia can still
form a relationship with their carer. Actions by the
carer can influence food intake of an older person
with dementia and include touching, kissing,
hugging, and responding to non-verbal cues.21
Caregivers can provide patients frequent reminders
to swallow, perform multiple swallows, make
gentle small coughs between feeds, and assume
an appropriate posture to reduce the risk of AP. A
pleasant quiet environment with less distraction is
desirable during the whole feeding process.
Reasons for a high prevalence of
tube feeding in advanced dementia
in Hong Kong
Family factors
Tube feeding is prevalent in Hong Kong among
older patients with advanced dementia for multiple
reasons. Family members may think that they cannot
allow the demented relative to starve. This may be
affected by the Chinese culture that emphasises
eating and avoidance of hunger at all costs. To
achieve this, there seems to be little other choice.
Physicians may be too optimistic and inform family
members that the tube can be removed if the patient
regains the ability to eat normally.22 The chance of
stopping tube feeding, however, is lower than 20%
in all indications for tube feeding.23 Family members
may insist on aggressive measures at all costs, despite
the futility.
Health care team factors
The current medical culture in Hong Kong is
predominantly biomedical, with life preservation
the overwhelming principle.24 Physicians may
recommend tube feeding in older patients with
advanced dementia because they believe clinical
outcomes can be thereby improved.25 Many
physicians are under pressure from family members
when discussing tube feeding.26 The health care team may be unfamiliar with the current literature about
the pitfalls of tube feeding and may not realise that
there is also an option of CHF. The health care team
may also fear legal consequences if patients with
advanced dementia are not fed with a feeding tube.
Lack of an advance directive and
advance care planning
Advance care planning (ACP) is a process of
communication among patients, their family, and
important others about the care they wish to receive
if they are unable to make decisions.27 Often one of
the discussions relates to the decision to start tube
feeding in the presence of severe eating problems.
One outcome of ACP is an expressed wish that is not
legally binding. Another option is for the patient to
sign an AD, a formal tool that respects the autonomy
of patients and in which any decision must be
adhered to by the health care team.28 In Hong Kong,
life-sustaining treatment, including tube feeding, can
be withheld if there is a valid AD when the patient is
in an irreversible coma, persistent vegetative state,
terminal illnesses, or other end-stage irreversible
life-limiting condition.29 Nonetheless until recently
ACP and AD have been seldomly discussed in
Hong Kong.30 When a patient without an AD is
unconscious due to an advanced irreversible illness,
the decision to withhold or withdraw tube feeding
is made by consensus of the health care team and
family members according to the best interests of
the patient, taking into account any prior wish or
treatment preference. Without knowing the exact
wishes of the patient, many health care teams and
family members are compelled to start tube feeding.
Practical issues in not using tube
feeding
In Hong Kong, there are practical issues associated with not using a feeding tube. Hand feeding is time-consuming.
In the hospital environment, because of
staff shortages, it is difficult to provide quality CHF
to all patients with advanced dementia having eating
problems. If an older patient is feeding poorly, it is
difficult to discharge them from hospital, especially
if they are returning to a RCHE. The environment
can also affect feeding.31 Medical wards in Hong
Kong public hospitals are often elderly unfriendly,
crowded, noisy, and without privacy. In addition,
nurses may be reluctant to hand feed the advanced
dementia patient with dysphagia after assessment by
a speech therapist. Without strong hospital policy
support, nurses understandably are concerned about
medicolegal consequences should the dysphagic
elderly patient aspirate following CHF. Hence,
not uncommonly, they will ask relatives who have
‘refused’ tube feeding of an elderly dysphagic older
to feed them. Family members who are unable to
come to the hospital 2 or 3 times a day will have
little choice but to alter their decision and agree to
tube feeding. In RCHEs, manpower issues and the
crowded environment are barriers to quality feeding
of those with dementia. Older RCHE residents who
are offered CHF but are feeding poorly will soon
become dehydrated, especially in summer. Staff in
RCHEs will soon bring their older residents back
to the emergency ward/department if they cannot
eat or are eating poorly, leading to a ‘revolving door’ phenomenon. Alternative ways of hydration,
including hypodermoclysis (subcutaneous fluid
infusion), are not practised in RCHEs in Hong
Kong.32 Not many family doctors are equipped
with the knowledge or have the time to take care of
advanced dementia cases with feeding problems in
RCHEs. Many medications need to be taken orally
and administration via an enteral tube may appear to
be the only alternative in dysphagic patients.
Hospital Authority guidelines on
life-sustaining treatment in the
terminally ill
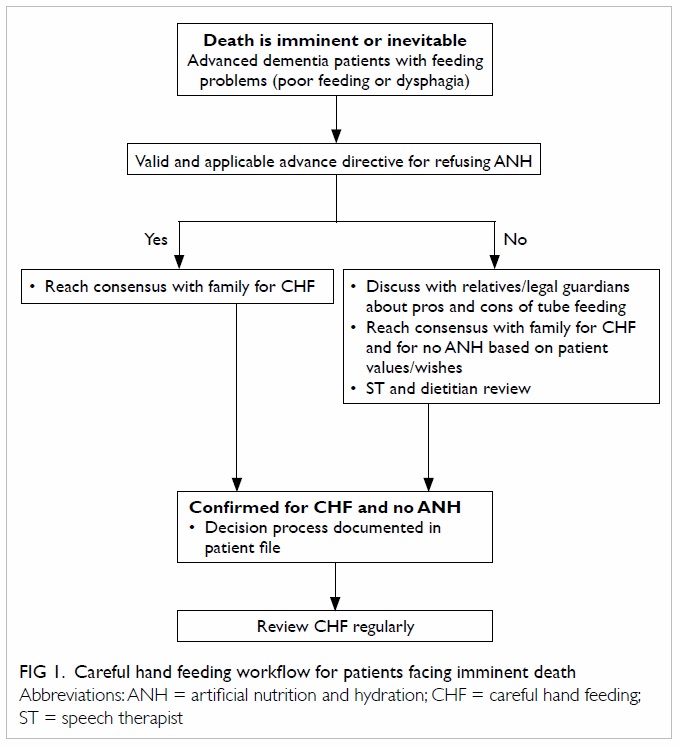
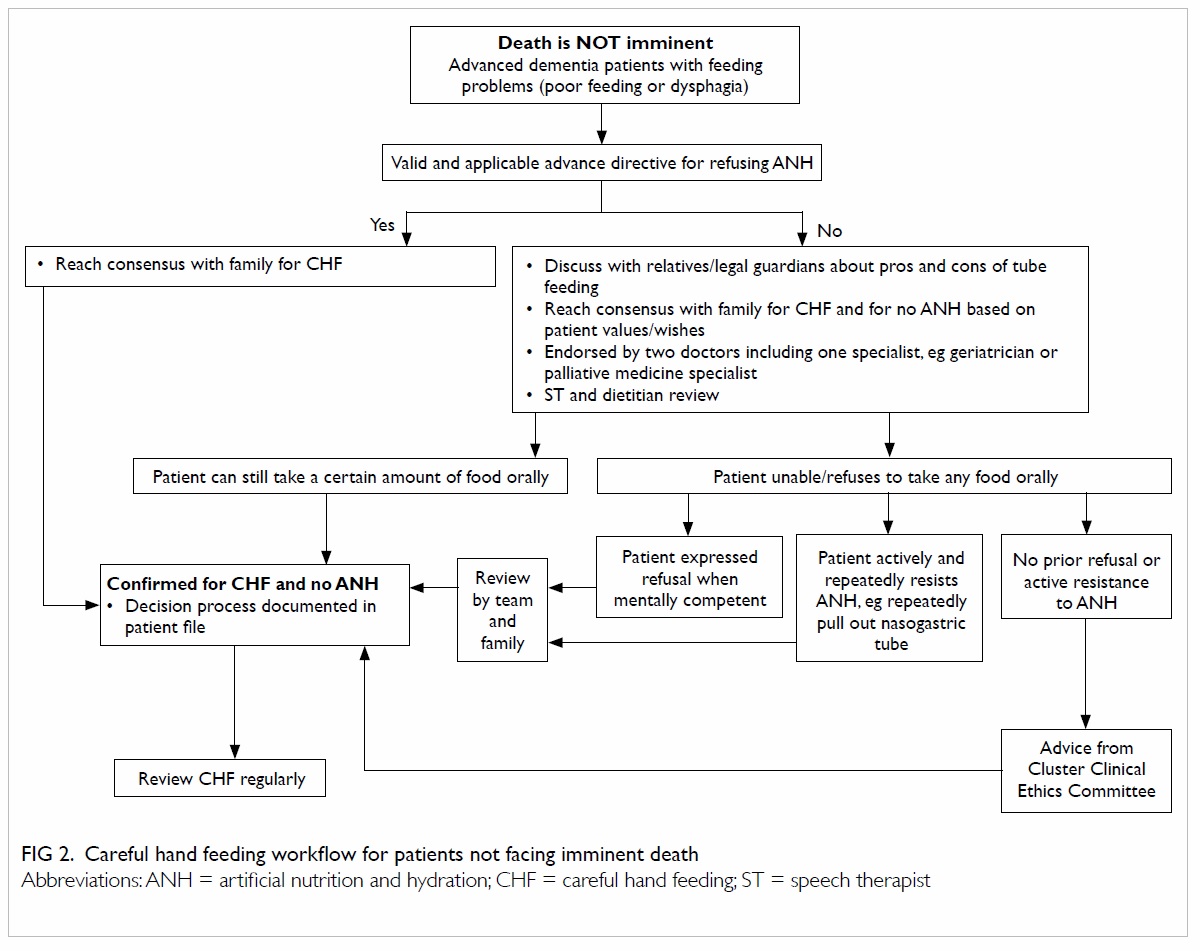
Artificial nutrition and hydration (ANH) refers
specifically to those techniques for providing
nutrition or hydration which are used to bypass
the swallowing process. They include the use
of nasogastric tubes, percutaneous endoscopic
gastrostomy, intravenous or subcutaneous fluid, and
parenteral nutrition. In September 2015, the Hospital
Authority guidelines on life-sustaining treatment
in the terminally ill was updated. Among other
key end-of-life care issues, the guidelines provide
a clear picture of CHF and ANH from the ethical
perspective.33 It states that when death is imminent
(death is expected within a few hours or days) and
inevitable in a mentally incompetent patient without
a valid AD, it is acceptable to withhold or withdraw
ANH. This follows the same principles that apply to
other life-sustaining treatments. Notwithstanding,
if a patient is in or near the end stage of a disease
or condition and is mentally incompetent, and
death is not imminent, the balance of benefits and
burdens of ANH may become unclear. The guideline
states that if the patient does not have a valid AD
refusing ANH, the consideration of withholding or
withdrawing ANH requires additional safeguards.
There must be consensus within the health care
team and with the family (if any) that a decision to
withhold or withdraw ANH is in the best interests
of the patient, taking into account their prior wishes
and values. The health care team must include at
least two doctors, one of whom must be a specialist
in a relevant field, eg geriatrician or palliative care
specialist. In addition, if the patient is unable to
swallow, the health care team should seek advice
from the ‘cluster clinical ethics committee’, before
making a decision to withhold or withdraw ANH,
unless before losing capacity, the patient has clearly
expressed a wish to refuse ANH (as reported clearly
by family members or documented in medical
notes when the patient was still competent) or the
patient actively and repeatedly resists ANH such as
repeatedly pulling out a nasogastric tube. Based on
the principles stipulated in the Hospital Authority
guidelines,33
Figures 1 and
2 were drawn showing
the flowcharts when death is imminent/inevitable
and when death is not imminent, respectively.
The way forward for feeding
patients with advanced dementia
in Hong Kong
There is no definitive solution for feeding problems
in older patients with advanced dementia. In the
absence of a valid AD, patient management should be
individualised, and the decision for tube feeding or
CHF should be shared between the health care team
and family members, based on the patient’s previously
expressed wishes and best interests. The health care
team should accept and respect the family’s choice
of CHF instead of tube feeding. Experienced nurses
and doctors should be responsible for discussing
the pros and cons of tube feeding with the family to
achieve a consensus. Clear hospital guidelines and
protocols should facilitate CHF and effect a cultural
change.34 Staff sentiments and medicolegal concerns
should be addressed. Clear Hospital Authority or
hospital policy to support CHF will help alleviate the
concerns of nursing staff. Training of doctors, nurses,
and other members of the health care team is vital to
the promulgation of CHF. There is an urgent need to
enhance the environment of public hospital wards so
that they are more elderly friendly. Training of RCHE
staff and the staff ratio are important factors that will
determine the success of CHF in the community of
Hong Kong. Without a well-prepared staff, patients
on CHF will soon be put on enteral feeding. The
Social Welfare Department can ensure it is part of
the licensing requirement to have end-of-life care
that includes CHF in most, if not all, RCHEs. More
palliative care training should be given to primary
doctors who look after older people with advanced
dementia.35 Recently, all medical students at the
University of Hong Kong have been seconded to
RCHEs to learn about community geriatrics as part
of their undergraduate training. They have first-hand
experience, under the guidance of geriatricians,
of how the elderly with advanced dementia are
cared for in RCHEs. More education about feeding
issues in dementia should be offered to the public.
Furthermore, ACP and AD should be promoted in
Hong Kong so that patients can elect a particular
mode of feeding while they are mentally capable.36 At
the time of writing this article, the Hong Kong SAR
Government is exploring the realisation of enduring
power of attorney for health care decision, allowing
mentally incapacitated older people to express their
wishes through a chosen advocate.37 It is hoped that
the decision to accept enteral feeding or not can be
included in the scope of the power of attorney.
References
1. Hong Kong population projections 2012-2041. Census
and Statistics Department, Hong Kong SAR Government;
2012.
2. Luk JK, Liu A, Ng WC, Lui B, Beh P, Chan FH. End-of-life
care: towards a more dignified dying process in residential
care homes for the elderly. Hong Kong Med J 2010;16:235-6.
3. Mitchell SL, Teno JM, Keily DK, et al. The clinical course of
advanced dementia. N Engl J Med 2009;361:1529-38.
Crossref
4. Hoffer LJ. Tube feeding in advanced dementia: the
metabolic perspective. BMJ 2006;333:1214-5.
Crossref
5. Luk JK, Chan FH, Pau MM, Yu C. Outreach geriatrics
service to private old age homes in Hong Kong West
Cluster. J Hong Kong Geriatr Soc 2002;11:5-11.
6. Luk JK, Chan WK, Ng WC, et al. Mortality and health
services utilization among older people with advanced
cognitive impairment living in residential care homes.
Hong Kong Med J 2013;19:518-24.
7. Luk JK, Chan DK. Preventing aspiration pneumonia in
older people: do we have the “know-how”? Hong Kong
Med J 2014;20:421-7.
8. Li I. Feeding tubes in patients with severe dementia. Am
Fam Physician 2002;65:1605-10, 1515.
9. Finucane TE, Christmas C, Travis K. Tube feeding in
patients with advanced dementia: a review of the evidence.
JAMA 1999;282:1365-70.
Crossref
10. Vergis EN, Brennen C, Wagener M, Muder RR. Pneumonia
in long-term care: a prospective case-control study of
risk factors and impact on survival. Arch Intern Med
2001;161:2378-81.
Crossref
11. Gomes GF, Pisani JC, Macedo ED, Campos AC. The
nasogastric feeding tube as a risk factor for aspiration and
aspiration pneumonia. Curr Opin Clin Nutr Metab Care
2003;6:327-33.
Crossref
12. Ciocon JO, Silverstone FA, Graver LM, Foley CJ. Tube
feedings in elderly patients. Indications, benefits, and
complications. Arch Intern Med 1988;148:429-33.
Crossref
13. Kuo S, Rhodes RL, Mitchell SL, Mor V, Teno JM. Natural
history of feeding-tube use in nursing home residents with
advanced dementia. J Am Dir Assoc 2009;10:264-70.
Crossref
14. Teno JM, Mitchell SL, Kuo SK, et al. Decision-making and
outcome of feeding tube insertion: a five-state study. J Am
Geriatr Soc 2011;59:881-6.
Crossref
15. Odom SR, Barone JE, Docimo S, Bull SM, Jorgensson D.
Emergency departments visits by demented patients with
malfunctioning feeding tubes. Surg Endosc 2003;17:651-3.
Crossref
16. Mitchell SL, Tetroe JM. Survival after percutaneous
endoscopic gastrostomy placement in older persons. J
Gerontol A Biol Sci Med Sci 2000;55:M735-9.
Crossref
17. DiBartolo MC. Careful hand feeding: a reasonable
alternative to PEG tube placement in individuals with
dementia. J Gerontol Nurs 2006;32:25-33.
18. American Geriatrics Society Ethics Committee and
Clinical Practice and Models of Care Committee. American
Geriatrics Society feeding tubes in advanced dementia
position statement. J Am Geriatr Soc 2014;62:1590-3.
Crossref
19. Hanson LC, Ersek M, Gilliam R, Carey TS. Oral feeding
options for people with dementia: a systematic review. J
Am Geriatr Soc 2011;59:463-72.
Crossref
20. Hanson LC. Tube feeding versus assisted oral feeding
for persons with dementia: using evidence to support
decision-making. Ann Longterm Care 2013;21:36-9.
21. Lange-Alberts ME, Shott S. Nutritional intake. Use of
touch and verbal cuing. J Gerontol Nurs 1994;20:36-40.
Crossref
22. Carey TS, Hanson L, Garrett JM, et al. Expectations and
outcomes of gastric feeding tubes. Am J Med 2006;119:527.e11-6.
23. Wolfsen HC, Kozarek RA, Ball TJ, Patterson DJ, Botoman
VA, Ryan JA. Long-term survival in patients undergoing
percutaneous endoscopic gastrostomy and jejunostomy.
Am J Gastroenterol 1990;85:1120-2.
24. Pang MC, Volicer L, Chung PM, Chung YM, Leung WK,
White P. Comparing the ethical challenges of forgoing
tube feeding in American and Hong Kong patients with
advanced dementia. J Nutr Health Aging 2007;11:495-501.
25. Shega JW, Hougham GW, Stocking CB, Cox-Hayley D,
Sachs GA. Barriers to limiting the practice of feeding tube
placement in advanced dementia. J Palliat Med 2003;6:885-93.
Crossref
26. Solomon MZ, O’Donnell L, Jennings B, et al. Decisions
near the end of life: professional views on life-sustaining
treatments. Am J Public Health 1993;83:14-23.
Crossref
27. Teno JM, Nelson HL, Lynn J. Advance care planning.
Priorities for ethical and empirical research. Hasting Cent
Rep 1994;24:S32-6.
Crossref
28. Chu LW, Luk JK, Hui E, et al. Advance directive and end-of-life care preferences among Chinese nursing home
residents in Hong Kong. J Am Med Dir Assoc 2011;12:143-52.
Crossref
29. Guideline for HA clinicians on advance directives in adults
(2014). Hong Kong: Hospital Authority; 2014.
30. Tse CY. Reflections on the development of advance
directives in Hong Kong. Asian Bioethics Rev 2016;8:211-23. Crossref
31. Amella EJ. Factors influencing the proportion of food
consumed by nursing home residents with dementia. J Am
Geriatr Soc 1999;47:879-85.
Crossref
32. Luk KH, Chan HW, Chu LW. Is hypodermoclysis suitable
for frail Chinese elderly? Asian J Gerontol Geriatr
2008;3:49-50.
33. HA guidelines on life-sustaining treatment in the
terminally ill 2015. Hong Kong: Hospital Authority; 2015.
34. Palecek EJ, Teno JM, Casarett DJ, Hanson LC, Rhodes RL,
Mitchell SL. Comfort feeding only: a proposal to bring
clarity to decision-making regarding difficulty with eating
for persons with advanced dementia. J Am Geriatr Soc
2010;58:580-4.
Crossref
35. Hong TC, Lam TP, Chao VK. Barriers for primary care
physicians in providing palliative care service in Hong
Kong—qualitative study. Hong Kong Pract 2010;32:3-9.
36. Luk JK, Liu A, Ng WC, Beh P, Chan FH. End of life care in
Hong Kong. Asian J Gerontol Geriatr 2011;6:103-6.
37. The Law Reform Commission of Hong Kong Report.
Enduring powers of attorney: personal care. July 2011.
Available from: http://www.hkreform.gov.hk/en/docs/repa2_e.pdf. Accessed 29 Apr 2017.