DOI: 10.12809/hkmj144416
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Three cases of early-stage localised Lyme disease
Mahizer Yaldiz, MD1;
Teoman Erdem, MD1;
Fatma H Dilek, MD2
1 Department of Dermatology, Sakarya University Training and Research Hospital, Sakarya 54010, Turkey
2 Department of Pathology, Sakarya University Training and Research Hospital, Sakarya 54010, Turkey
Corresponding author: Dr Mahizer Yaldiz (drmahizer@gmail.com)
Case reports
Case 1
A 6-year-old girl was referred to our hospital in July
2010 with a red patch on one leg. The red patch
had appeared 15 days after a tick-bite and become
increasingly large within the last 1.5 months.
Dermatological examination revealed an irregular
annular erythema of 10 x 15 cm, with ecchymotic
centre and pale outer edge on the anteromedial part
of her left thigh (Fig a). Systemic examination as well as complete blood picture and liver and renal
function tests were normal. In view of the history of
tick-bite and prediagnosis of erythema chronicum
migrans (ECM), Borrelia burgdorferi serology was
requested and confirmed positive immunoglobulin
(Ig) M to B burgdorferi. A diagnosis of Lyme disease
was considered and treatment was started with
amoxicillin and clavulanic acid at a paediatric dose
of 50 mg/kg/day. After 15 days, the patient showed
clinical improvement and at 6-month follow-up
there were no systemic findings.
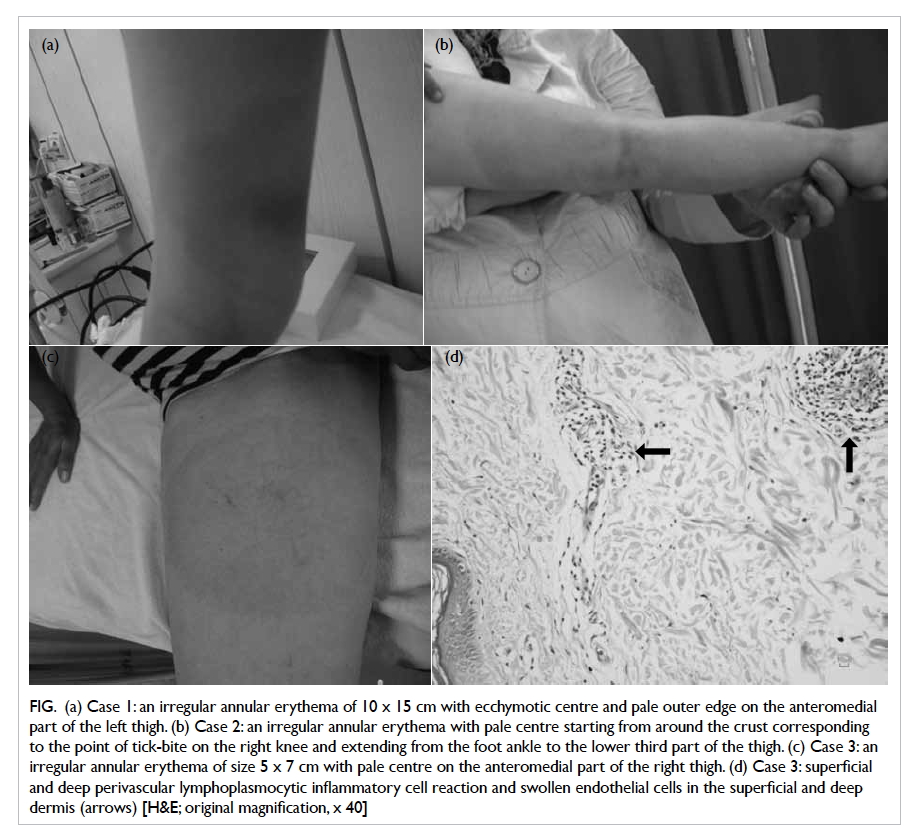
Figure. (a) Case 1: an irregular annular erythema of 10 x 15 cm with ecchymotic centre and pale outer edge on the anteromedial part of the left thigh. (b) Case 2: an irregular annular erythema with pale centre starting from around the crust corresponding to the point of tick-bite on the right knee and extending from the foot ankle to the lower third part of the thigh. (c) Case 3: an irregular annular erythema of size 5 x 7 cm with pale centre on the anteromedial part of the right thigh. (d) Case 3: superficial and deep perivascular lymphoplasmocytic inflammatory cell reaction and swollen endothelial cells in the superficial and deep dermis (arrows) [H&E; original magnification, x 40]
Case 2
A 2-year-old girl was referred to our hospital in May
2010 with a red patch on one leg that developed 10
days after a tick-bite and became increasingly large.
Dermatological examination revealed an irregular
annular erythema with pale centre starting from
around the crust corresponding to the tick-bite
on her right knee and encompassing an area from
the ankle to the lower third of the femur (Fig b).
Systemic examination was normal as were complete
blood picture and liver and renal function tests.
Borrelia burgdorferi serology was not performed.
Lyme disease was considered and treatment
was started with amoxicillin-clavulanic acid at a
paediatric dose of 50 mg/kg/day. The patient showed
clinical improvement after 15 days and there were no
systemic findings at 6-month follow-up.
Case 3
A 53-year-old female patient was referred to our
hospital in June 2010 with a red patch on her right
leg that developed about 1 month previously and had
steadily enlarged over the preceding 10 days. She had
been bitten by a tick in the same region approximately
1.5 months earlier. Dermatological examination
revealed an irregular annular erythema of about 5
x 7 cm with pale centre on the anteromedial part
of her right thigh (Fig c). Systemic questioning and
examination was normal and B burgdorferi serology,
IgM, and IgG were negative. Histopathological
examination of a skin biopsy revealed a perivascular
lymphoplasmocytic inflammatory cell reaction and
swelling of the endothelial cells in the superficial and
deep dermis. The findings were consistent with ECM
(Fig d). In view of the anamnesis and clinical and
histopathological findings, the case was diagnosed
as Lyme disease. Treatment was started with oral
doxycycline (100 mg twice daily for 2 weeks). Follow-up
at 15 days showed clinical improvement and the
patient had no systemic findings after 6 months.
Discussion
Lyme disease is a systemic disorder that can affect
many organs and is caused by some Borrelia species
transmitted by the Ixodes genus of ticks. There are
three genotypes of Borrelia that cause Lyme disease
in humans: Borrelia burgdorferi sensu strico, Borrelia
afzelii, and Borrelia garinii, collectively known as
Borrelia burgdorferi sensu lato. Vector-transmitted
Lyme infection is frequently seen in the United
States and Europe.1 2 3 4 5 6 7
In Turkey, the disease was first reported in
1990 in the Black Sea and Aegean Regions of the
country. To date, 25 types in the family Ixodidae
have been reported in Turkey.1 2 3 4 5 6 7 8 9 Ixodes ricinus may
be seen in all geographical areas of the country
but is particularly widespread in humid forest
areas (Black Sea, Marmara, and Mediterranean
regions). The definitive prevalence of B burgdorferi
infection in Turkey is unknown because of limited
investigations. Seropositivity in the general
population has been reported as 2% to 6% and in
risk groups in endemic region as 6% to 44%, but
values change with different country regions.10 11 12 13 14 Lyme disease is seen in both genders and in all
age-groups, but is more prevalent in adults aged
between 30 and 59 years and in children under 15
years of age.13 Approximately 60 cases have been
reported in Turkey since 1990. When children were
analysed, approximately 48% had a history of tick
retention and most of the skin lesions were identified
(approximately 46% in early stage). Neuroborreliosis
is the second common clinical form to be reported.
The Lyme disease is more common in women (70%)
and the age distribution is 4 to 72 years (mean, 29.1
years); cases are mostly seen between March and
July when vectors (nymphs) are active.15
Erythema chronicum migrans is the most
frequently seen and most important diagnostic skin
lesion in Lyme disease.3 6 7 It occurs on any part of
the body and appears at the site of a tick-bite after an
incubation period of 3 to 32 days, depending on the
migration of spirochaetes in the skin. The incubation
period can extend to 6 months, however.3 7 9 The
lesion that starts as a red macule or papule rapidly
expands outwards. It will then turn pale in the
centre and develop into an annular rash, giving the
appearance of a target board or bull’s eye.7 13 The diameter of the lesion varies between 4 cm and
60 cm. The lesion should have a minimal diameter of
5 cm in order to be defined as ECM. Local symptoms
such as a burning sensation, itching, or pain may be
reported.7 11
Following primary infection, the acute
disseminated stage starts with dissemination of the
causative agent to other tissues via blood and lymph
vessels. The skin findings at this stage of infection
include secondary ECM, borrelial lymphocytoma,
urticarial plaques, erythema nodosum, and a malar
rash.3 14 Secondary ECM lesions occur at sites distant from the tick-bite and will range in number from 2
to 30. The initial ECM may be followed by similar
but generally smaller and often non-migrating
lesions. More than 10 lesions are uncommon, but
may occur.3 4 7 Borrelial lymphocytoma presents
as a solitary bluish-red soft nodule with a slightly
atrophic surface that varies from 1 to 5 cm in
diameter, and occurs most frequently on the earlobe,
nipple, scrotum, or axillary region. In this stage
of dissemination, cardiac, neurological, and joint
findings predominate.1 4 7 8
After several months or years, untreated
patients may go on to develop late-stage Lyme
disease. Acrodermatitis chronica atrophicans is
the characteristic skin lesion in this stage. Other
findings are of mono- or oligo-arthritis, meningoencephalitis,
and uveitis. This stage may be the result
of an immunopathological process in the absence of
clinical regression with antibiotic therapy, a chronic
inflammatory response, and no isolation of the
causative bacterium from the lesions.2 3 4 7 12 The three cases reported here showed only an ECM lesion and
no systemic findings at 6-month follow-up. This was
consequent to adequate therapy commenced at an
early stage of the disease.
The diagnosis of Lyme disease is based on
symptoms, objective physical findings (ECM,
facial paralysis, arthritis, etc), and a history of
tick contact.1 4 9 The results of enzyme-linked
immunosorbent assay and Western blot analysis can
be used to support the diagnosis.4 9 The diagnosis of early-stage Lyme disease is based on the presence
of ECM and history of tick-bite.3 6 7 Since the rate of
false-negative results is high in the acute stage of the
disease, serological tests are not recommended, but
are used to support the clinical findings of early- and
late-disseminated stages of Lyme disease.8 9 10 11 12 Our case 1 confirmed positive IgM to B burgdorferi. Case
2 underwent no serological tests. In case 3, both IgM
and IgG were negative to B burgdorferi.
Skin biopsy is used for the differential
diagnosis of ECM. In ECM cases, there is a patch-like
perivascular mononuclear infiltration of the
superficial and deep dermis. This infiltration consists
of predominantly lymphocytes and histiocytes as
well as plasma cells in varying quantities.3 7 11 In
our case 3, histopathological examination of her
skin biopsy for differential diagnosis demonstrated
perivascular lymphoplasmocytic inflammatory cell
infiltration in the superficial and deep dermis. This
histopathological picture supported our diagnosis of
ECM.
Doxycycline, amoxicillin, and cefuroxime
axetil are the antibiotics of choice. The recommended
duration of therapy for early-stage disease is 14 to
21 days and for late stage at least 4 weeks.4 7 12 Since
our first two cases were children, they received
amoxicillin and clavulanic acid 50 mg/kg/day for
15 days. Our case 3 was an adult and received oral
doxycycline (100 mg twice daily for 2 weeks). At 15
days, all lesions were completely cured in all patients,
and there was no relapse or systemic involvement at
6-month follow-up.
In conclusion, ECM is an important clinical
sign of early-stage Lyme disease. The diagnosis and
therapy of Lyme disease at an early stage is vital
as it prevents progression to late-stage disease.
In endemic regions and in patients with a history
of tick-bite, the clinician should stay alert to the
presence of ECM. If a patient is considered to have
ECM, specific investigations for Lyme disease should
be ordered.
References
1. Winn WJ, Allen S, Janda W. Spirochetal infections.
Koneman’s color atlas and textbook of diagnostic
microbiology. 6th ed. Philadelphia: Lippincott Williams
and Wilkins; 2006: 1135-43.
2. Mullegger RR. Dermatological manifestations of lyme
borreliosis. Eur J Dermatol 2004;14:296-309.
3. Topcu AW, Soyletir G, Doğanay M, Doğanci L. Lyme
disease: infectious diseases and microbiology. 3. Istabul:
Nobel Tip Kitapevleri; 2008: 973-88.
4. Borriello SP, Murray PR, Funke G. Postic D. Borrelia. Topley
and Wilson’s microbiology and microbial infections. 10th
ed. London: Hodder Arnold; 2005: 1818-37.
5. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS,
Leffel DJ. In: Mahalingam M, Bhawan J, Chomat AM, Hu
L. Lyme borreliosis. Fitzpatrick’s dermatology in general
medicine. 7th ed. New York: McGraw Hill; 2008: 1797-806.
6. Tepe B, Sayiner HS, Karincaoğlu Y. Early stage localized
Lyme disease: case report [in Turkish]. İnönü Üniversitesi
Tip Fakültesi Dergisi 2011;18:122-5.
7. Bolognia JL, Jorizzo JL, Rapini RP, Espana A. Figurate
erythemas. Dermatology. St Louis: Mosby; 2003:
277-86.
8. Evans SE, Karaduman A. Eritemli dermatozlar [in Turkish]. Turk J Dermatol 2009;3:55-62.
9. UtaŞ S, Kardag Y, Doganay M. The evaluation of Lyme
serology in patients with symptoms which may be related
with Borrelia burgdorferi [in Turkish]. Mikrobiyoloji
Bulteni 1994;28:106-12.
10. Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser
GP. Diagnosis of lyme borreliosis. Clin Microbiol Rev
2005;18:484-509. Crossref
11. DePietropaolo DL, Powers JH, Gill JM, Foy AJ. Diagnosis of
lyme disease. Am Fam Physician 2005;72:297-304.
12. Anlar FY, Durlu Y, Aktan G, et al. Clinical characteristics
of Lyme disease in 12 cases [in Turkish]. Mikrobiyol Bul
2003;37:255-9.
13. Koksak I, Saltoğlu N, Bingul T, Ozturk H. A case of Lyme
disease [in Turkish]. Ankem Dergisi 1990;4:284.
14. Gargili A. Lyme disease: factors and epidemiology. II.
Proceedings of Turkey Zoonotic Diseases Symposium;
2008 Nov 27-28. Ankara: Program ve Bildiri Kitabi; s:89-92.
15. Kiliç S. Lyme disease: the pathogen and epidemiology [in
Turkish]. Turkiye Klinikleri J Infect Dis Spec Top 2014;7:29-41.

