DOI: 10.12809/hkmj154790
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Extensive mediastinal aspergillosis presenting
with dyspnoea and cardiac tamponade symptoms
Syed F Mustafa, MD1;
Hamza AR Khan, MD1;
Saulat H Fatimi, MD2
1 Medical College, Aga Khan University, Karachi, Pakistan
2 Division of Cardiothoracic Surgery, Department of Surgery, Aga Khan University, Karachi, Pakistan
Corresponding author: Dr Hamza AR Khan (hamza_saeedahmed@hotmail.com)
Case report
An 18-year-old girl was admitted to the Aga Khan
Hospital, Pakistan in April 2014 with progressively
worsening shortness of breath, orthopnoea, malaise,
and low-grade fever for 3 years, and generalised
body swelling for 6 months. She had no significant
medical history or trauma.
On physical examination she was a medium-built
girl with a heart rate of 120 beats/min, raised
jugular venous pressure, and bilateral pedal pitting
oedema. Chest auscultation revealed muffled heart
sounds with bilateral basilar lung crepitations. The
chest X-ray showed wide mediastinum with clear
lung markings.
The computed tomographic (CT) scan showed
a conglomerate undefined mass in the anterior,
middle, and posterior mediastinum encasing the
entire heart and great vessels with most marked
extension in the retrocardiac area (Fig 1). The
echo showed a large echo-dense mass compressing
the heart with invasion into the left atrium (LA),
obliterating most of the LA cavity.
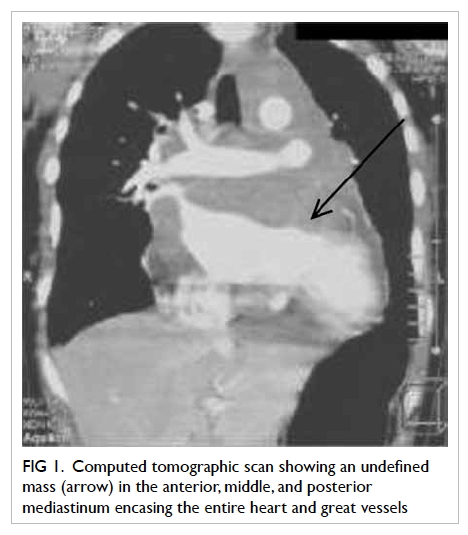
Figure 1. Computed tomographic scan showing an undefined mass (arrow) in the anterior, middle, and posterior mediastinum encasing the entire heart and great vessels
Video-assisted thoracoscopic surgery
was performed and the mass biopsied for
histopathological examination. The histopathology
showed fibrosis and chronic granulomatous
inflammation with fungal hyphae on periodic acid–Schiff staining (Fig 2). The fungal cultures grew
Aspergillus flavus.
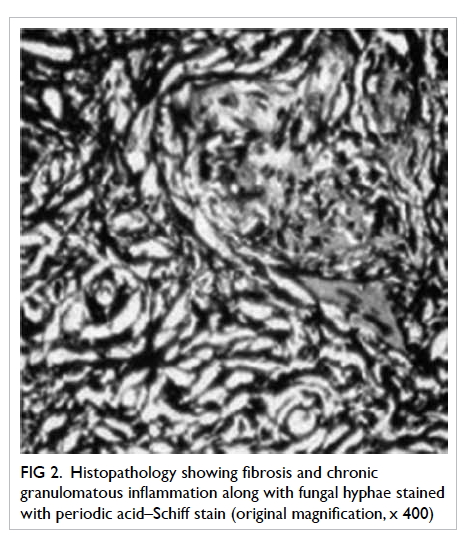
Figure 2. Histopathology showing fibrosis and chronic granulomatous inflammation along with fungal hyphae stained with periodic acid–Schiff stain (original magnification, x 400)
A diagnosis of invasive mediastinal
aspergillosis was made and the patient was started
on oral itraconazole 100 mg twice a day. She showed
a remarkable recovery in her symptomatology in the
first 6 weeks of follow-up.
Discussion
Aspergillosis refers to a variety of diseases caused
by several species of Aspergillus organisms that
are abundant in the environment and recognition
of which has increased over recent years. There
are three main categories in general: saprophytic
aspergilloma, allergic bronchopulmonary
aspergillosis, and invasive aspergillosis. The term
‘invasive aspergillosis’ is generally used to imply a
histopathologically demonstrated invasion of tissues
by these spores. It represents an important cause
of morbidity and mortality, particularly among
immunocompromised patients, occurring mostly
in those with haematological malignancies who are
undergoing chemotherapy and organ transplantation
with concomitant immunosuppressive therapy.
Extension of invasive pulmonary aspergillosis to
the mediastinum has been reported only rarely.1
Our case is an immunocompetent patient with
extensive mediastinal aspergillosis who presented
with dyspnoea and symptoms of cardiac tamponade.
Invasive aspergillosis varies in severity and
clinical course, depending upon the affected organ
and the host. It is caused by many Aspergillus
groups; however the most common is the Aspergillus
fumigatus group. These groups live in soil, and
derive nutrients from dead plants and animal matter.
It has been further subdivided in recent years to
angioinvasive and airway-invasive aspergillosis.
Invasive aspergillosis is a major cause of morbidity
and mortality in immunosuppressed patients.2
The form that Aspergillus lung disease takes
is heavily dependent on the immune response of
the patient.3 Indolent forms of locally invasive
aspergillosis in the form of chronic necrotising
or semi-invasive aspergillosis in apparently
immunocompetent individuals are now recognised.
Invasive aspergillosis is a result of three
factors: (1) suppression of the immune response due
to debilitating disease or therapy; (2) glucocorticoid
therapy with consequent diminished inflammatory
response and disruption of the normal flora by
antimicrobial agents4; and (3) local implantation
of the fungus. The disease is well known in
immunocompromised individuals but has also been
described in healthy individuals. Patients with a
compromised immune system, specifically with
neutropenia, are susceptible to acute airway-invasive
and angioinvasive aspergillosis in the absence of pre-existing
lung pathology.
There have been a few cases described in
which patients were immunocompetent. Orr et al5
documented two patients with normal host defences
in whom postmortem examination revealed death
due to disseminated aspergillosis (one patient had
a history of coronary heart disease, the other acute
renal failure following gangrenous appendicitis).
Our patient was otherwise healthy as confirmed by
the normal haematological studies.
The usual pathogenesis of invasive aspergillosis
is by dissemination from a primary site, such as the
lungs or the paranasal sinuses, or by contiguous
spread.6 In this particular patient, the chest X-ray and
CT scan of the chest were clear without a primary
lesion. It was therefore postulated that inhalation
of the fungal spores with immediate mediastinal
invasion resulted in the implantation of a high
concentration of aspergillus spores around the heart.
This was followed by chronic infiltration around the
pericardium and extension into the heart.
This idea was supported by the histopathology
report of granulomatous tissue fibrosis, indicating
a long-standing process, and in keeping with the
history of worsening shortness of breath for 3 years.
Our case showed an undefined mass in the anterior,
middle, and posterior mediastinum extending into
the LA. The effects of the mass could explain all of
the patient’s symptoms, namely worsening dyspnoea
and cardiac tamponade symptoms.
In conclusion, this case highlights that
there is usually a long dormant period before the
clinical manifestation of aspergillosis, clinically
and radiologically the disease may be suggestive
of a malignant process, and contamination with
aspergillus should be considered from all possible
aspects, particularly in healthy individuals.
References
1. Shakoor MT, Ayub S, Ayub Z, Mahmood F. Fulminant
invasive aspergillosis of the mediastinum in an
immunocompetent host: a case report. J Med Case Rep
2012;6:311. Crossref
2. Al-Alawi A, Ryan CF, Flint JD, Müller NL. Aspergillus-related
lung disease. Can Respir J 2005;12:377-87. Crossref
3. Gefter WB. The spectrum of pulmonary aspergillosis. J
Thorac Imaging 1992;7:56-74. Crossref
4. Mashimoto H, Suyama N, Araki J, et al. A case of
mediastinitis and bilateral pyothorax, following acute
epiglottitis with concurrent Aspergillus infection [in
Japanese]. Kansenshogaku Zasshi 1992;66:648-52. Crossref
5. Orr DP, Myerowitz RL, Dubois PJ. Patho-radiologic
correlation of invasive pulmonary aspergillosis in the
compromised host. Cancer 1978;41:2028-39. Crossref
6. Hendrix WC, Arruda LK, Platts-Mills TA, Haworth CS,
Jabour R, Ward GW Jr. Aspergillus epidural abscess and
cord compression in a patient with aspergilloma and
empyema. Survival and response to high dose systemic
amphotericin therapy. Am Rev Respir Dis 1992;145:1483-6. Crossref

