Hong Kong Med J 2016 Oct;22(5):445–53 | Epub 19 Aug 2016
DOI: 10.12809/hkmj154747
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Clinical transition for adolescents with developmental disabilities in Hong Kong: a pilot study
Tamis W Pin, PhD;
Wayne LS Chan, PhD;
CL Chan, BSc (Hons) Physiotherapy;
KH Foo, BSc (Hons) Physiotherapy;
Kevin HW Fung, BSc (Hons) Physiotherapy;
LK Li, BSc (Hons) Physiotherapy;
Tina CL Tsang, BSc (Hons) Physiotherapy
Department of Rehabilitation Sciences, Hong Kong Polytechnic University, Hunghom, Hong Kong
Corresponding author: Dr Tamis W Pin (tamis.pin@polyu.edu.hk)
This paper was presented as a poster at the Hong Kong Physiotherapy Association Conference 2015, Hong Kong on 3-4 November 2015.
Abstract
Introduction: Children with developmental
disabilities usually move from the paediatric to adult
health service after the age of 18 years. This clinical
transition is fragmented in Hong Kong. There are
no local data for adolescents with developmental
disabilities and their families about the issues they
face during the clinical transition. This pilot study
aimed to explore and collect information from
adolescents with developmental disabilities and their
caregivers about their transition from paediatric to
adult health care services in Hong Kong.
Methods: This exploratory survey was carried out
in two special schools in Hong Kong. Convenient
samples of adolescents with developmental
disabilities and their parents were taken. The
questionnaire was administered by interviewers in
Cantonese. Descriptive statistics were used to analyse
the answers to closed-ended questions. Responses to
open-ended questions were summarised.
Results: In this study, 22 parents (mean age ±
standard deviation: 49.9 ± 10.0 years) and 13
adolescents (19.6 ± 1.0 years) completed the face-to-face questionnaire. The main diagnoses of the
adolescents were cerebral palsy (59%) and cognitive
impairment (55%). Of the study parents, 77% were
reluctant to transition. For the 10 families who did
move to adult care, 60% of the parents were not
satisfied with the services. The main reasons were
reluctant to change and dissatisfaction with the adult
medical service. The participants emphasised their
need for a structured clinical transition service to
support them during this challenging time.
Conclusions: This study is the first in Hong Kong
to present preliminary data on adolescents with
developmental disabilities and their families during
transition from paediatric to adult medical care.
Further studies are required to understand the needs
of this population group during clinical transition.
New knowledge added by this study
- These results are the first published findings on clinical transition for adolescents with developmental disabilities in Hong Kong.
- Dissatisfaction with the adult health services and reluctance to change were the main barriers to clinical transition.
- The concerns and needs of the families were similar regardless of whether adolescents had physical or cognitive disabilities.
- A structured clinical transition service is required for adolescents with developmental disabilities and their parents.
- Further in-depth studies are required to examine the needs for and concerns about clinical transition for all those involved. This should include adolescents with developmental disabilities, their parents or caregivers, and service providers in both paediatric and adult health services.
Introduction
Advances in medical management now enable
children with developmental disabilities (DD)
who may previously have died to live well into
adulthood.1 Such disabilities are defined as any
condition that is present before the age of 22 years
and due to physical or cognitive impairment or a
combination of both that significantly affects self-care,
receptive and expressive language, mobility,
learning, independent living, or the economic
independence of the individual.2 The transition
from adolescence to adulthood is a critical period
for all young people.3 In a clinical context, adult
transition is “the purposeful, planned movement of
adolescents and young adults with chronic physical
and medical conditions from child-centered to adult-oriented
health-care systems”.4 In 2001, a consensus
statement with guidelines was endorsed to ensure
adolescents with DD, who depend on coordinated
health care services, make a smooth transition to
the adult health care system in order to receive the
services that they need in developed countries such
as the United States.5
Researchers have identified needs and factors
necessary for the successful transition of adolescents
with DD.6 7 From the adolescent’s perspective,
barriers to success include their dependence on
others, reduced treatment time and access to
specialists in the adult health service, lack of information
about transition, and lack of involvement in the
decision-making process. Parents of adolescents
with DD were reluctant or confused about changing
responsibilities during the transition period. The
majority of challenges came from the service
systems and included unclear eligibility criteria
and procedures, limited time and lack of carer
training, fragmented adult health service provision, lack
of communication between service providers, and
inaccessibility to resources including information.6 7
Based on the 2015 census of ‘Persons with
disabilities and chronic diseases in Hong Kong’ from
the Hong Kong Census and Statistics Department,
there were 22 100 (3.8%) people with disability
(excluding cognitive impairment) aged between
15 and 29 years, ie who were transitioning from
the paediatric to adult health service.8 According
to the Hospital Authority, Hong Kong, all public
hospitals, and specialist and general out-patient
clinics are organised into seven hospital clusters
based on geographical location.9 The Duchess of
Kent Children’s Hospital (DKCH) is a tertiary centre
that provides specialised services for children with
orthopaedic problems, spinal deformities, cerebral
palsy and neurodevelopmental disorders, and
neurological and degenerative diseases. Unlike
overseas health care, there is no children’s hospital in
Hong Kong that provides an acute health service. All
paediatric patients go to the same hospital as adult
patients but are triaged into the paediatric section
for management by both in-patient and out-patient
services. The specialised out-patient clinic list under
each hospital cluster varies. Children with DD might
receive services from general paediatrics clinic,
a cerebral palsy clinic, Down’s clinic, behavioural
clinic, or paediatric neurology out-patient clinic.
Once a child reaches the age of 18 years, they are
referred to the adult section of the same hospital
for continued care. They will be followed up in
neurology or movement disorder clinics, where other
patients with adult-onset neurological conditions
or movement disorders, such as stroke, Parkinson’s
disease, multiple sclerosis are followed up. There
is no separate specialised clinic for complex child-onset
DD.10
Although adult transition for adolescents with
DD has been recognised as a crucial area in health
care overseas, it is an under-developed service in
Hong Kong.11 A local study found that there is a
service gap in adult transition for young people
with chronic medical conditions, such as asthma,
diabetes, and epilepsy. Training and education
are urgently required for both service providers
and young people with chronic health conditions
and their families.11 It is unclear if the challenges
and barriers identified in overseas literature6 7 are
applicable to Hong Kong, where the paediatric and
adult health services, especially the medical services,
are located in the same building. At present, no
study has been conducted with adolescents with DD
and their families in Hong Kong about the issues
they face during clinical transition. As a start, in this
pilot study, we aimed to explore the acceptance of
clinical transition and identify the main barriers to
successful clinical transition for adolescents with
DD and their caregivers in Hong Kong.
Methods
Participants
A survey study was conducted on a convenience
sample of adolescents and/or their caregivers, who
were recruited from two special high schools (Hong Kong Red Cross John F Kennedy Centre [JFK] and Haven of
Hope Sunnyside School [HOH]) in Hong Kong. Students from
JFK have primarily physical and multiple disabilities
including cerebral palsy or muscular dystrophy and
those from HOH have severe cognitive impairment.
Both schools provide rehabilitation services on
site including physiotherapy, occupational therapy,
speech therapy, nursing support, and family support
via the school social workers. The medical out-patient
services for the students fall under different
hospital clusters, depending on where the students’
families live. The parents are responsible for taking
their adolescent children for medical review. As there
was no previous study on which basis to calculate
the required sample size and as a pilot study, we
aimed to recruit 10 adolescents and their parents/caregivers in each school.
The inclusion criteria of the adolescents were: (1) aged 16 to 19 years and (2) a diagnosis of DD.
All participating adolescents and/or their parents or
legal guardians gave written informed consent before
the survey. For adolescents with severe cognitive
impairment, consent was sought from their parents
as proxy and only their parents participated in the
survey. This pilot study was approved by the Human
Subjects Ethics Sub-committee of the Hong Kong
Polytechnic University.
Survey
A specific questionnaire was developed for this
pilot study to collect information relative to: (1)
demographic characteristics of the participants; (2)
whether or not the study participants were aware of
the transition and the information source(s); (3) if
the study participants were willing to transition to
the adult health service and the underlying reasons;
(4) for those who had transitioned, if they were
satisfied with the adult health service and the underlying
reasons; and (5) the opinion of the study participants
of the clinical transition service. As a pioneer pilot
study, health service included both medical and
rehabilitation services and the study aimed to explore
the general issues faced by this group of adolescents
and their families during clinical transition. Lastly,
as we predicted that the competency level of the
adolescents and their caregivers in managing their
disabilities might influence their perception of
clinical transition, information about their self-rated
competency level was also collected. Questions in
the latter part were based on information from the
Adolescent Transition Care Assessment Tool and
were designed to assist health care professionals
to provide a better transition for adolescents with
chronic illness.12 The whole survey was administered
by interviewers for the study adolescents and/or their
caregivers separately in Cantonese. All interviews
were recorded for data analyses.
The survey comprised closed- and open-ended
questions. The closed-ended questions were designed
to require a dichotomous answer, ie ‘yes’ or ‘no’, or
an answer from a set of choices. For example, when
asked about the sources of information about clinical
transition, the study participants could choose
their answers from a list of professionals such as
paediatricians, social workers, physiotherapists, and
school teachers. The open-ended questions focused
on the reasons for an earlier response. For example,
when asked if they wished to move to the adult health service, the individual would first answer ‘yes’ or ‘no’, then give their reasons. For the questions about
self-perceived competency level, study participants
read a number of statements (8 for the adolescents
and 14 for parents) and indicated how much they
agreed with the statement using a Likert-scale from
‘strongly disagree’ to ‘strongly agree’.
Data analyses
Descriptive statistics—including mean, median,
standard deviation, or quartiles—were used
to analyse the responses to the closed-ended
questions. Discussion of the open-ended questions
was transcribed and summarised by five team
members (CLC, KHF, KHWF, LKL, and TCLT). The
content was analysed and themes were identified
independently by two other team members (TWP
and WLSC). These themes were discussed and a
consensus reached by all team members.
Results
Thirteen potential families were approached at the
JFK via the physiotherapist of the school anticipating
possible refusal by some. All the students and their
parents agreed to participate, so all were included.
Ten families were approached at the HOH via the
social worker at the school but one parent declined
the offer and no other family was interested in
participating in the study. Since the students from
HOH, who were cognitively impaired, were not able
to be interviewed, only their parents/caregivers
were interviewed. As a result, 22 parents (13 from
the JFK and 9 from the HOH) and 13 adolescents
(all from the JFK) were asked to complete the
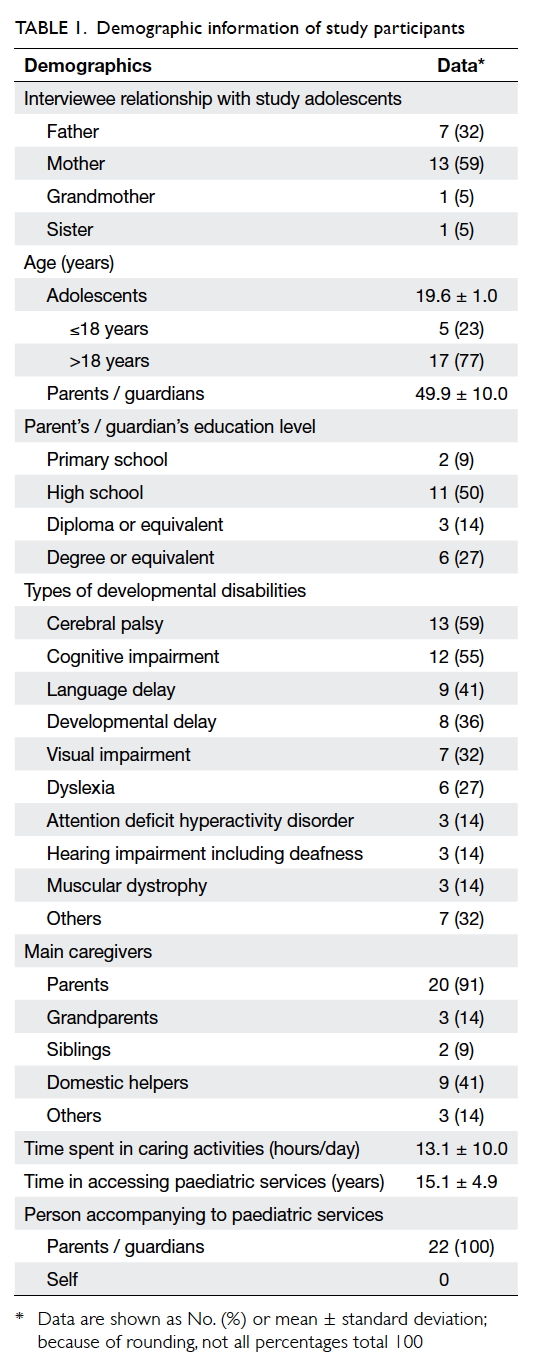
face-to-face survey. The demographic data of the
participants are listed in Table 1. Cerebral palsy and
cognitive impairment were the principal types of
DD. All adolescents received rehabilitation from the
Hospital Authority and/or from their special school.
All the adolescents accessed between four and seven
paediatric medical specialists (eg paediatrician,
neurologist, orthopaedic surgeon) and rehabilitation
services (eg physiotherapy, occupational therapy,
speech therapy) indicating their complex needs.
Over 90% of the JFK students were followed up at the
DKCH that is within walking distance of the school
(personal communication, Senior Physiotherapist at
JFK).
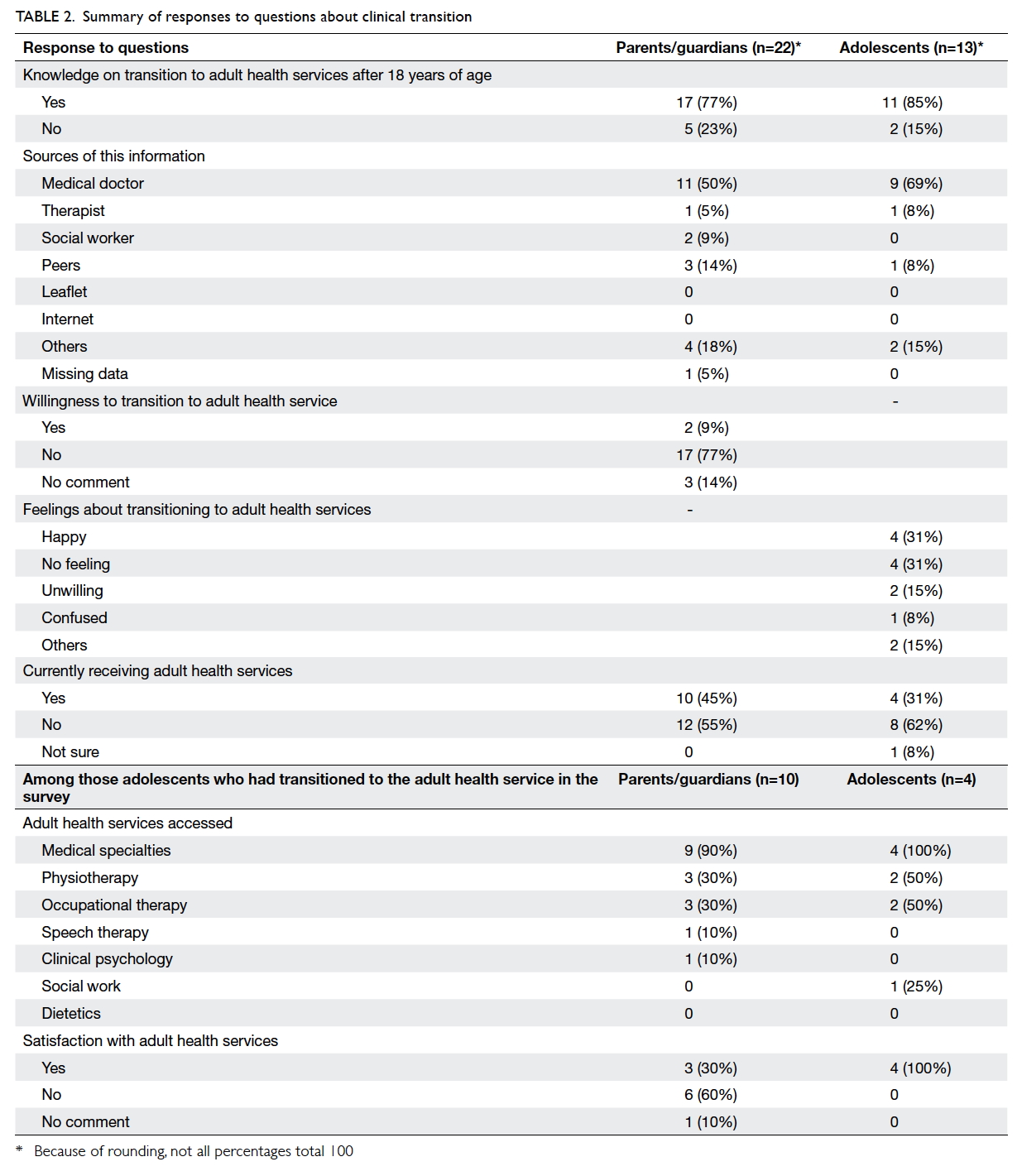
Table 2 summarises the participant responses
about clinical transition. The majority of the parents
(77%) and adolescents (85%) knew that clinical
transition to adult care would occur at 18 years of age.
They were mainly informed by their paediatrician
(50% of parents and 69% of adolescents). Most
parents (77%) were reluctant to make this move.
Ten parents stated that their adolescent child was
already receiving care from the adult sector and over
half of them (60%) were dissatisfied with the service.
Four of the 13 adolescents clearly stated that they
had transitioned to the adult health service during
the survey and all of them were happy with the
transition. Among those 17 families who knew that clinical transition to adult care would occur at 18 years of age, 10 adolescents were all over 18 years old, whereas those in another seven (41%) families were also over 18 years old and still receiving services from the paediatric sector at the time of the study.
When asked why they were not willing to the
transition or why they were dissatisfied after the
transition, the parent responses could be summed up
as two main areas of concern: reluctance to change
and dissatisfaction with the adult health services. Most
parents (16/22, 73%) did not want to change their
existing care circumstances. When asked why, some
parents cited dissatisfaction with the adult health service or
health system (for the latter, 13/22, 59% of parents).
For example, parents found it difficult to attend the
follow-up appointments using public transport.
Although there was a free shuttle bus service for
families who needed it, parents were frustrated by
the limited service.
Some parents also wanted more flexible
visiting hours in the adult hospital so that they could
look after their adolescent children, especially those
who were cognitively impaired. The parents worried
about the quality of care for their children who
were entirely dependent for their daily activities.
They were also unhappy about the waiting time for
medical appointments and stated that their children
with DD had a short attention span and were unable
to control their behaviour. Long waiting times in a
crowded waiting area, which is commonly observed
in the adult setting, could easily trigger their
behavioural problems.
There was also dissatisfaction with the adult
health service providers (13/22, 59% of parents). Parents
often found that the adult medical staff demonstrated
limited understanding and knowledge of their child’s
clinical presentation and abilities, especially for those
with severe cognitive impairment. The adult health
service providers did not know how to communicate
with the cognitively impaired adolescents and
treated them as other normal adults.
There is no formal clinical transition service in
Hong Kong but when asked, the majority of parents
(21/22, 95%) and adolescents (11/13, 85%) stated
that they would welcome such a service. About two
thirds of the study parents and adolescents (23/35,
66%) would like the clinical transition service to
support them during the clinical transition. About
one third of the parents (7/22, 32%) believed that the
service could act as a bridge linking the paediatric
and adult health services, providing information about
available services in the adult sector.
The Figure summarises the responses of
adolescents for self-perceived competency in
managing their disability, and Table 3 summarises
the study parents’ responses. Most adolescents
demonstrated understanding of instructions (11/13,
85%), confidence in communicating with the service
providers about their condition (10/13, 77%), and
understanding the importance of treatments for
their condition (12/13, 92%) [Fig]. About half were
confident in seeking help from different specialties
according to their condition (6/13, 46%) and making
medical decisions (7/13, 54%) [Fig]. Over half of the adolescents, however, lacked the confidence to
attend routine medical visits on their own (8/13,
62%) and worried about the unfamiliar adult medical
service (6/13, 46%) [Fig]. Most parents stated that
they were familiar with their children’s medical
conditions and treatments (20/22, 91%) and able to
seek help from different medical specialties based on
their child’s condition (14/22, 64%) [Table 3]. Only
a minority of parents (1/22, 5%), however, believed
that their children were capable of attending medical
appointments on their own. Less than half of the
parents believed that their children would be able to
explain their medical condition (9/22, 41%) or make
independent clinical decisions in the future (7/22,
32%). None of the parents of an adolescent with
cognitive impairment believed that the child would
ever be able to manage their own health.
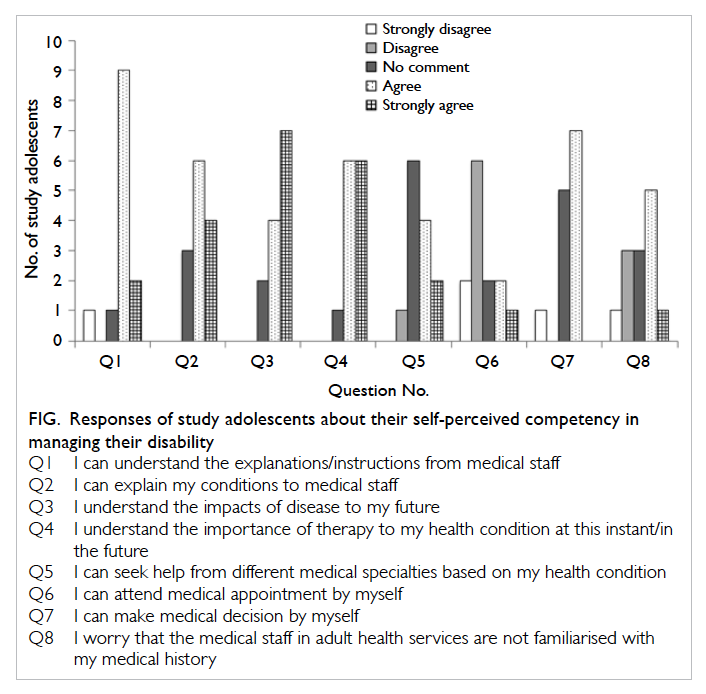
Figure. Responses of study adolescents about their self-perceived competency in managing their disability
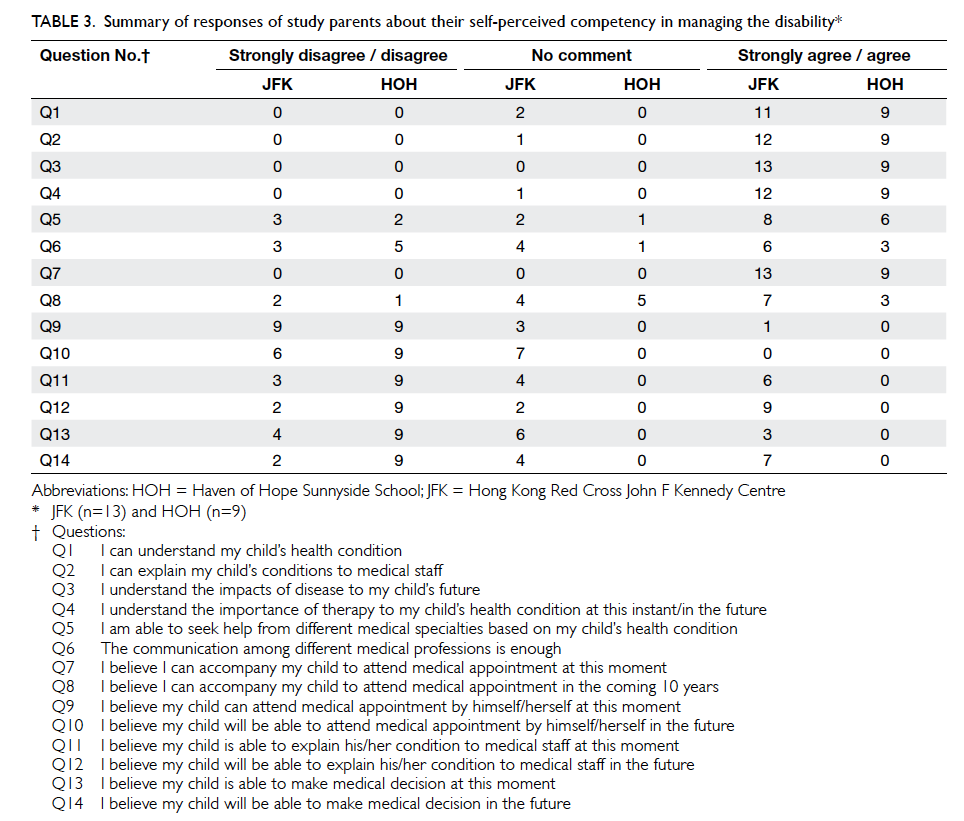
Table 3. Summary of responses of study parents about their self-perceived competency in managing the disability
Discussion
The present pilot study aimed to determine how
adolescents with DD and their parents in Hong
Kong accept the clinical transition and identify
the main barriers to successful transition. This was
the first step to understanding the issues of this
population group during clinical transition and to
enable planning for the future. As far as we know,
this study is the first to be conducted in Hong Kong
for this population group. Overall, 22 parents and 13
adolescents were recruited from two special schools
(one for primarily physically disabled children and
the other for severe physically and/or cognitively
impaired individuals), aiming to understand what
was the acceptance level and barriers faced by these
two vastly different groups with DD. The results
were very similar between these two subgroups,
indicating that the study parents had similar issues
during clinical transition, regardless of the type of
DD of their child. Hence, the results from these two
subgroups were discussed as one group.
Most of the study participants were aware of
the clinical transition necessary at the age of 18 years.
Only 10 (45%) of the 22 families shifted to the adult health service, despite the fact that their adolescent child
was close to or over 18 years old (Tables 1 and 2). The
reasons for this delay were not thoroughly explored
but it has been suggested that medical practitioners
in the paediatric service felt that the adolescents were
not ready for the transition so they continued to see
them well into adulthood while the parents and the
adolescents were reluctant to make the move.11 The
latter appeared to be true because when asked, most
study participants did not want to change and move
to the adult health service. This contradicts the results of
a previous local study of adolescents with chronic
medical conditions, in which over 80% of the study
participants (adolescents and parents) were willing
to move to the adult health service.11 The difference is likely
due to the complexity of the health conditions of
the present cohort. Adolescents with DD usually
have varying degrees of physical and/or cognitive
impairment and so depend more on others for
managing their health condition, making them and
their carers more anxious about any change.6 7 For
those with chronic medical conditions, the physical
and cognitive abilities of the adolescent were
unlikely affected and hence the adolescents could
manage their condition more independently and
more readily after the transition.13 This speculation
was supported by the findings about self-perceived
competency level. Most study adolescents, who
had mainly physical disabilities, were not confident
about attending a medical appointment alone
because of their limited physical abilities (Fig). The
reluctance for change may also be due to fear of
the unknown and of not being well prepared.11 In
Hong Kong, clinical transition is non-structured and
unplanned.11 Parents are often informed just before
the transition, leading to poor preparation and
confusion. Early and continuous clinical transition
from early adolescence can enable parents and
adolescents with DD to be prepared and actively
participate in the transition planning.7 14 Although
the clinical transition service is not well-known in
Hong Kong, the study participants had a positive
attitude towards a clinical transition service to help
them navigate the process by bridging the paediatric
and adult health services. In addition, the study parents
wished to have more information about available
adult health services, eg rehabilitation services, wheelchair
maintenance services, etc. More information
about the unknown has been shown to reduce the
reluctance of parents and adolescents to change and
to further improve their confidence about moving to
adult care.5 6 15 16
Another barrier was dissatisfaction with the
health care system and service providers in the
adult setting (Table 2), and is in line with present
literature.7 Some parents found it difficult to arrange
transport to the adult hospital for follow-up while
most of the appointments were currently at the
special school. More accessible public transport
might help, especially in Hong Kong, where private
vehicles are not a common option. Flexible visiting
hours in the adult hospital that would enable parents
to care for their dependent adolescent child may also
reduce their dissatisfaction. Longer waiting times
for medical appointments in the adult setting was
frequently mentioned by the study parents. In the
adult sector, patients with all kinds of neurological
conditions, both child-onset and adult-onset, are
reviewed in the same clinic. The number of patients
attending the clinic is vastly increased compared
with the paediatric setting. In addition, patients
with adult-onset neurological conditions and their
family may not understand the characteristics of DD.
Stressed behaviour of an adolescent child with DD
may be perceived by other families as impatience.
In the paediatric clinic, where all clinic attendees
were children or adolescents with DD and their
parents, the waiting time was shorter. Families as
well as clinic staff had a full understanding of DD
and would be more tolerant. It is likely that this lack
of support in the adult setting further discouraged
the study parents to make the transition willingly.
Changes to the existing health care system, such
as a separate clinic for child-onset DD conditions,
may be a possible small step to assist this group
in making a smooth transition. Education about
clinical transition for staff in both the paediatric and
adult settings allows them to prepare the families in
advance. Education about paediatric conditions and
communication with adolescents with DD can also
equip adult staff with confidence so they develop a
strong rapport with the families.16
Interestingly, from the perspective of
the adolescents, the four adolescents who had
transitioned stated that they were happy with the
adult health service. Two (50%) adolescents indicated that
because the ‘new’ doctors did not know them well,
they paid more attention to them and one adolescent
did not give any reason to support his statement. It is
likely that in the paediatric sector, these adolescents
had been followed up from early childhood by the
same medical staff who virtually watched them grow
up. A change of scene and people in the adult sector
is welcomed by these adolescents. In addition, they
might welcome the idea that they have started to
actively participate in the consultation as a ‘patient’,
unlike in the paediatric sector, where the consultation
was directed at their parents, not them.14
Parents of adolescents who had physical and/or cognitive impairment had a similar perception of
their adolescent child, that they would never be able
to attend a medical appointment alone, presumably
because of their disability (responses to questions 9
to 10 in Table 3). None of the parents of a cognitively
impaired adolescent child believed their child to
be capable of explaining their medical condition
to others or making an independent medical
decision. On the contrary, parents of a physically
disabled child thought that while it may not apply at
present, their child would be able to make their own
decisions in future (responses to questions 11 to 14
in Table 3). Nonetheless, there was a discrepancy in
this perception between the study adolescents and
parents (Fig and Table 3). Most adolescents believed
they could explain their condition to others (question
2 in the Fig) and over half believed that they could
make an independent medical decision at the time
of the study (question 7 in the Fig). Further studies
are needed to determine whether this discrepancy is
due to confusion on the part of the parents because
of changing responsibilities during the transition.13
While western literature emphasises the importance
of active participation by adolescents during clinical
transition,14 it would be interesting to see if this can
be endorsed in a parent-dominant Chinese society
such as Hong Kong, where cultural differences may
influence attitudes towards clinical transition.17
We were unable to analyse other challenges
identified in overseas literature, such as unclear
eligibility criteria and procedures and limited time
for clinical transition, because comparable data were
not available for Hong Kong. In other developed
countries, adolescents are shifted with the assistance
of a clinical transition service based in the children’s
hospital (if any) or by applying clinical guidelines for
best service.18 In Hong Kong, adolescents are referred
from the paediatric section to the adult section
within the same hospital. Each hospital cluster may
have different procedures for this ‘transition’ and
there is no defined department within the hospital
structure to assist adolescents and their families
through this process. Nor do the families receive any
advice about how to negotiate this process. A future
in-depth study is recommended to understand the
existing situation of clinical transition in different
hospital clusters and determine how to establish a
more formal approach among all the hospital clusters
in Hong Kong to support this group of adolescents
and their families during this confusing time.
Limitations of the present study
There may have been a selection bias in the
study sample as the families were approached
by convenience through the school staff. Due to
the small sample size, no statistical analysis was
conducted to compare the subgroups of adolescents
with physical and cognitive impairments. Although
the sample size was small, the purpose of the present
pilot study was not to generalise the findings to all
adolescents with DD but to begin to understand
the acceptance of clinical transition and the main
barriers to success for adolescents with DD and
their family in Hong Kong. The present results are
also in line with the literature in this area.4 7 11 14 17
Future studies with a larger sample size and more
in-depth qualitative data are required to verify the
present results. The potential subjective bias of the
results, especially for the open-ended questions, was
another limitation but we attempted to minimise
this through consensus agreement among the team.
Conclusions
In the present explorative study, close to half of the
study families had a delayed clinical transition to the
adult health service. Most study parents were reluctant for
their adolescent children to shift to the adult health service
due to unwillingness to change and dissatisfaction
with the adult medical service. A structured and
well-planned clinical transition was urged by the
study participants to bridge the paediatric and
adult health services and to provide support to the family.
Further studies are required to analyse the needs and
concerns of adolescents with DD and their families
as well as the service providers in the adult medical
setting to facilitate the future development of a
clinical transition service in Hong Kong.
Acknowledgements
The authors would like to thank all the participating
families from the Hong Kong Red Cross John F Kennedy Centre
and Haven of Hope Sunnyside School.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Westbom L, Bergstrand L, Wagner P, Nordmark E. Survival
at 19 years of age in a total population of children and
young people with cerebral palsy. Dev Med Child Neurol
2011;53:808-14. Crossref
2. Public Law 98-527, Developmental Disabilities Act of 1984.
3. Staff J, Mortimer JT. Diverse transitions from school to
work. Work Occup 2003;30:361-9. Crossref
4. Blum RW, Garell D, Hodgman CH, et al. Transition from
child-centered to adult health-care systems for adolescents
with chronic conditions. A position paper of the Society
for Adolescent Medicine. J Adolesc Health 1993;14:570-6. Crossref
5. American Academy of Pediatrics, American Academy
of Family Physicians, American College of Physicians-American Society of Internal Medicine. A consensus
statement on health care transitions for young adults with
special health care needs. Pediatrics 2002;110(6 Pt 2):1304-6.
6. Bindels-de Heus KG, van Staa A, van Vliet I, Ewals FV,
Hilberink SR. Transferring young people with profound
intellectual and multiple disabilities from pediatric to adult
medical care: parents’ experiences and recommendations.
Intellect Dev Disabil 2013;51:176-89. Crossref
7. Stewart D, Stavness C, King G, Antle B, Law M. A critical
appraisal of literature reviews about the transition to
adulthood for youth with disabilities. Phys Occup Ther
Pediatr 2006;26:5-24. Crossref
8. Persons with disabilities and chronic diseases in Hong
Kong. Hong Kong: Hong Kong Census and Statistics
Department; 2016. Available from: http://www.statistics.gov.hk/pub/B71501FB2015XXXXB0100.pdf. Accessed Jul
2016.
9. Clusters, hospitals & institutions. Hospital Authority.
2016. Available from: http://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=10036&Lang=ENG&Dimension=100&Parent_ID=10004. Accessed Jul 2016.
10. Hospital Authority Statistical Report 2012-2013. Hong
Kong: Hospital Authority; 2013.
11. Wong LH, Chan FW, Wong FY, et al. Transition care for
adolescents and families with chronic illnesses. J Adolesc
Health 2010;47:540-6. Crossref
12. Hong Kong Society for Adolescent Health. Adolescent
Transition Care Assessment Tool, Public Education Series
No. 12 (2013). Available from: http://hksah.blogspot.hk/2013/11/adolescent-transition-care-assessment.html.
Accessed 6 Feb 2016.
13. Stewart DA, Law MC, Rosenbaum P, Willms DG. A
qualitative study of the transition to adulthood for youth
with physical disabilities. Phys Occup Ther Pediatr
2002;21:3-21. Crossref
14. Viner RM. Transition of care from paediatric to adult
services: one part of improved health services for
adolescents. Arch Dis Child 2008;93:160-3. Crossref
15. Blum RW. Introduction. Improving transition for
adolescents with special health care needs from pediatric
to adult-centered health care. Pediatrics 2002;110(6 Pt
2):1301-3.
16. Stewart D. Transition to adult services for young people
with disabilities: current evidence to guide future research.
Dev Med Child Neurol 2009;51 Suppl 4:169-73. Crossref
17. Barnhart RC. Aging adult children with developmental
disabilities and their families: challenges for occupational
therapists and physical therapists. Phys Occup Ther Pediatr
2001;21:69-81. Crossref
18. Department of Health. National Service Framework for
Children, Young People and Maternity Services. Transition:
getting it right for young people. Improving the transition
of young people with long term conditions from children’s
to adult health services. 2006. Available from: http://dera.ioe.ac.uk/8742/1/DH_4132145%3FIdcService%3DGET_FILE%26dID%3D23915%26Rendition%3DWeb. Accessed Jul
2016.