Hong Kong Med J 2016 Aug;22(4):320–6 | Epub 3 Jun 2016
DOI: 10.12809/hkmj154748
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Correlation of thermal deficit with clinical parameters and functional status in patients with unilateral lumbosacral radiculopathy
Irena M Dimitrijevic, MSc, MD1;
Mirjana N Kocic, MD, PhD2;
Milica P Lazovic, MD, PhD3;
Dragan D Mancic, PhD4;
Olga K Marinkovic, MD2;
Dragan S Zlatanovic, MSc, MD2
1 Department of Rehabilitation of Neurology, Traumatic, Rheumatic
Patients and After-surgery States, Institute for Treatment and Rehabilitation “Niška Banja”, Niš, Serbia
2 Clinic for Physical Medicine and Rehabilitation, Clinical Center Niš, Niš, Serbia and Faculty of Medicine, University of Niš, Niš, Serbia
3 Institute for Rehabilitation Belgrade, Belgrade, Serbia and Faculty of
Medicine, University of Belgrade, Belgrade, Serbia
4 Department of Electronics, Faculty of Electronic Engineering, University
of Niš, Niš, Serbia
Corresponding author: Dr Irena M Dimitrijevic (irenadimitrije@gmail.com)
Abstract
Introduction: Lumbosacral radiculopathy is a
pathological process that refers to the dysfunction of
one or more spinal nerve roots in the lumbosacral
region of the spine. Some studies have shown that
infrared thermography can estimate the severity of
the clinical manifestation of unilateral lumbosacral
radiculopathy. This study aimed to examine the
correlation of the regional thermal deficit of the
affected lower extremity with pain intensity, mobility
of the lumbar spine, and functional status in patients
with unilateral lumbosacral radiculopathy.
Methods: This cross-sectional study was conducted
at the Clinic for Physical Medicine and Rehabilitation
of the Clinical Center Niš, Serbia. A total of 69
patients with unilateral lumbosacral radiculopathy of
discogenic origin were recruited, with the following
clinical parameters evaluated: (1) pain intensity by
using a visual analogue scale, separately at rest and
during active movement; (2) mobility of the lumbar
spine by Schober test and the fingertip-to-floor test;
and (3) functional status by the Oswestry Disability
Index. Temperature differences between the
symmetrical regions of the lower extremities were
detected by infrared thermography. A quantitative
analysis of thermograms determined the regions of
interest with maximum thermal deficit. Correlation
of maximum thermal deficit with each tested
parameter was then determined.
Results: A significant and strong positive correlation
was found between the regional thermal deficit and
pain intensity at rest, as well as pain during active
movements (rVAS – rest=0.887, rVAS – activity=0.890; P<0.001).
The regional thermal deficit significantly and strongly
correlated with the Oswestry Disability Index score
and limited mobility of the lumbar spine (P<0.001).
Conclusions: In patients with unilateral lumbosacral
radiculopathy, the values of regional thermal deficit
of the affected lower extremity are correlated with
pain intensity, mobility of the lumbar spine, and
functional status of the patient.
New knowledge added by this study
- The values of the regional thermal deficit, especially at the heel and plantar region of the affected foot, significantly and strongly correlated with radicular pain intensity.
- The values of the regional thermal deficit of the affected lower extremity also correlated with limited mobility of the lumbar spine and functional status of patients with unilateral lumbosacral radiculopathy.
- Infrared thermography may be applied for an objective assessment of radicular pain intensity.
Introduction
Lumbosacral radiculopathy is a pathological process
that refers to the dysfunction of one or more spinal
nerve roots in the lumbosacral region of the spine. It
is a frequent consequence of degenerative changes in
the intervertebral discs that cause compression of the
spinal nerve root in the intervertebral foramen.1 The
main clinical characteristic of this disease is pain that
spreads from the lumbar spine to one of the lower
extremities.1 In addition, a typical clinical presentation
is characterised by sensory deficits, muscle weakness,
and impaired deep tendon reflexes.1 2
The initial diagnosis of radiculopathy is
based on a detailed patient history and physical
examination.3 A precise diagnosis requires
information about the function of the spinal nerve
root, as well as structural changes in the spine
so additional diagnostic procedures are used:
electrodiagnostic testing and magnetic resonance
imaging (MRI) or computed tomography.2 3
There is a possibility of using infrared
thermography (IRT) since vasomotor dysfunction
caused by irritation or damage of the spinal nerve
root leads to abnormal changes in skin temperature
of the affected lower extremity.2 4 5 6 7 8 Temperature
differences between the symmetrical parts of
the lower extremities can be detected by IRT. A
quantitative analysis of the recorded temperature
differences provides information that may indicate
unilateral radiculopathy.4 5 7 Considering the ability
of IRT to estimate vasomotor instability, it can be
used to detect unilateral radiculopathy and thus
supplement the findings of clinical, morphological,
and functional examination.7 Some studies have
shown that IRT can estimate the severity of the
clinical manifestation of unilateral lumbosacral
radiculopathy.5 9 10 11
The aim of this study was to examine the
correlation of regional thermal deficit of the affected
lower extremity with pain intensity, mobility of the
lumbar spine, and functional status in patients with
unilateral lumbosacral radiculopathy.
Methods
Patients
This cross-sectional study included out-patients
with lumbosacral radiculopathy who were treated at
the Clinic for Physical Medicine and Rehabilitation
of the Clinical Center Niš, Serbia, between February
2012 and January 2013. Clinical Center Niš is a
tertiary institution that provides health services
for the whole southeast and south Serbia, with a
population of around 3 million. Clinical Center
Niš is also the educational and scientific research
base of the Faculty of Medicine, University of Niš.
During the study period, 97 of 213 patients with
lumbosacral radiculopathy were recruited. All
were aged over 18 years, had symptoms present
for more than 6 weeks, and had unilateral clinical
manifestations. The diagnosis was made by
clinical examination and confirmed by additional
investigations such as needle electromyography
or MRI. Patients were excluded if they had any of
the following: pregnancy, skin changes (lacerations,
inflammation, haemangioma), inflammatory joint
disease, malignant disease, infectious disease,
disorders of peripheral circulation (varicosities,
thrombophlebitis), neurological disorder (various
neuropathies), spinal stenosis, cauda equina
syndrome, bilateral lumbosacral radiculopathy, or
previous injury of the lumbosacral region of the
spine as well as previous surgical interventions in the
same region. Of 97 recruited patients, five refused
to participate and 23 patients were excluded due
to anamnestic or clinical indicators of the diseases
listed in the exclusion criteria. A total of 69
patients with unilateral lumbosacral radiculopathy
of discogenic origin were eligible for the study.
The study was approved by the Ethics
Committee of the Faculty of Medicine, University
of Niš (no. 01-6481-2). All patients gave written
consent to participate in the study.
Clinical and functional evaluation
We measured the following parameters by clinical
examination:
(1) Pain intensity was measured on a visual
analogue scale (VAS). This scale represents a
10-cm horizontal scale, graded 0 to 10, where 0
is a condition without pain and 10 is the worst
possible pain.12 Pain intensity was measured
separately at rest and during active movement
of the lumbar spine. The patients marked their
pain intensity on VAS as an average value of
the pain they had experienced for 7 days before
the test.
(2) The mobility of the lumbar spine was tested
by (a) fingertip-to-floor distance (FFD) that
refers to measuring the flexion of the lumbar
spine as a distance from the tip of the middle
finger to the floor, expressed in centimetres,13 and (b)
the Schober test that assesses the mobility by
measuring changes in the distance between
the two spinal marks. Spinal marks were made
on the skin at the spinous process of L5 and
10 cm above when a patient stood in a neutral
position. The patient then bent forward with
straight knees and the change in distance
between these marks is measured in centimetres.14 The
investigator, who was blinded to the results of
other assessments, tested the mobility of the
lumbar spine.
(3) The functional ability of patients was estimated
by the Oswestry Disability Index (ODI) that
comprises 10 questions. Each question has
six given answers that are graded 0 to 5 points.
After completing the questionnaire, the points
were added and expressed in percentages with
respect to the maximum number of points
(50), where a higher value corresponds to more
severe functional disability.15
The participants filled in the questionnaire in
their native language, without any assistance from
the investigators.
Infrared thermographic imaging
The examined patients were recorded by infrared
(IR) imaging camera and the thermograms were
quantitatively analysed. The operator, who recorded
and analysed the thermograms, did not know
the nature of the patient’s disease. In this study,
only one set of recordings was used, according
to the recommendation of the guidelines for
neuromusculoskeletal thermography that a single
set of thermograms can be adequate in cases where
obvious temperature asymmetry exists.16
The conditions of thermographic recording
were the same for all patients, according to the
guidelines for neuromusculoskeletal thermography
of the American Academy of Thermology.16 Room
temperature, where the recordings were conducted,
was always within the range of 20°C to 25°C. The room
was protected from direct ultraviolet exposure and
air conditioning was turned off. Local application of
analgesics and cosmetic preparations were avoided
before the recording. Corticosteroids, sympathetic
blockers, vasoactive medications, and transdermal
patches were not used for at least 24 hours before the
recording. Physical procedures were not conducted
at least 12 hours before and electrodiagnostic testing
24 hours before the recording.16
The body part marked as the region of interest
(ROI) was without clothes for at least 15 minutes
prior to recording. The ROIs were the front and back
part of the lower extremity, and plantar area of the
foot and the heel. During the recording of the plantar
surface of the foot, patients were seated with legs
in the horizontal plane and feet in a vertical plane
without touching each other. The recording of the
lower extremity was done with patients in a standing
position with lower extremities in slight abduction.
A varioSCAN high-resolution 3021 imaging camera
(Jenoptik, Dresden, Germany) recorded bilateral
ROIs. The analysis of the thermograms was done by
IRBIS Professional 2.2. graphic-oriented software
package (InfraTec GmbH, Dresden, Germany).
Quantitative analysis of the thermograms
determined the average temperature value of
ROIs, expressed in degrees Celsius. For each patient
and for each separate ROI, a difference in average
temperature value was calculated, between ROI of
unaffected and affected lower extremity, according
to the formula:
ΔT = mean value temperature ROI of unaffected
lower extremity – mean value temperature ROI of
the affected extremity
In order to correlate regional thermal deficit
(ΔT) with other examined parameters, ROI with maximum ΔT (max ΔT) value was considered.
In the final stage of the research, a correlation
analysis of max ΔT and each separate tested parameter was performed.
Statistical analysis
Data were analysed using the Statistical Package for
the Social Sciences (Windows version 10.0; SPSS
Inc, Chicago [IL], US). Normal distribution was
tested by Kolmogorov-Smirnov test. The results of
the statistical analysis were represented as mean ± standard deviation for data with normal distribution,
or as median for data without normal distribution.
In order to test the correlation between max ΔT
and other tested parameters, Pearson correlation
coefficient (r) was used for normal distribution
or Spearman correlation coefficient (ρ) for data
without normal distribution. A P value of <0.05
was considered statistically significant.
Results
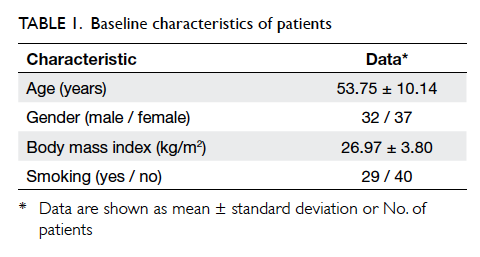
Baseline characteristics of patients are shown in
Table 1. Thermogram of the lower extremities
showed a significant thermal deficit (ΔT >1°C) in the
affected lower extremity in at least one out of four
recorded ROIs. In the majority of patients (n=43;
62.3%), maximum ΔT value was obtained at the heel
or plantar region of the foot. Outcome measures
are shown in Table 2 as mean value for parameters
with normal distribution and median value with
interquartile range for parameters without normal
distribution.
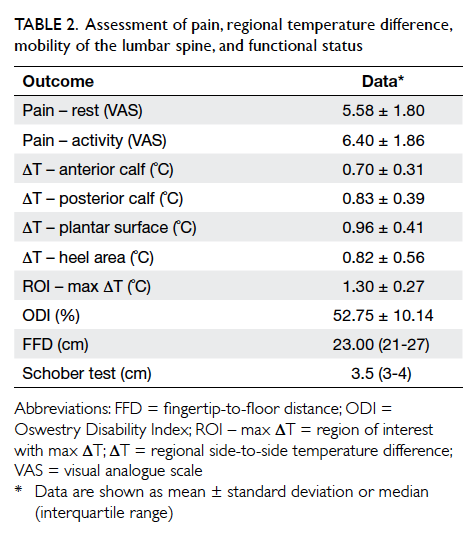
Table 2. Assessment of pain, regional temperature difference, mobility of the lumbar spine, and functional status
A statistically significant and strong positive
correlation was found between max ΔT and pain
intensity at rest (VAS – rest), as well as pain during
active movement (VAS – activity), and showed that
pain intensity (VAS – rest and VAS – activity) increased
along with increased value of max ΔT (rVAS – rest=0.887, rVAS – activity=0.890; P<0.001).
It has also been determined that there was a
significant and strong positive correlation between
max ΔT and ODI score that indicates a relationship
between these two parameters in that the functional
condition of the patient worsened with increased
max ΔT (r=0.744; P<0.001).
Furthermore, a statistically significant and
strong correlation was evident between max ΔT and
limited mobility of the lumbar spine. Nonetheless,
it should be emphasised that the correlation
between max ΔT and FFD was positive (ρ=0.776;
P<0.001) whereas the correlation between max ΔT
and Schober test was negative (ρ= –0.795; P<0.001).
The relationship between these parameters showed
that the mobility of the lumbar spine was reduced
with increased value of max ΔT. Scatter plots show
the results of correlation analyses (Figs 1, 2, 3).
Thermograms of two patients with different values
of thermal deficit are shown in Figure 4.
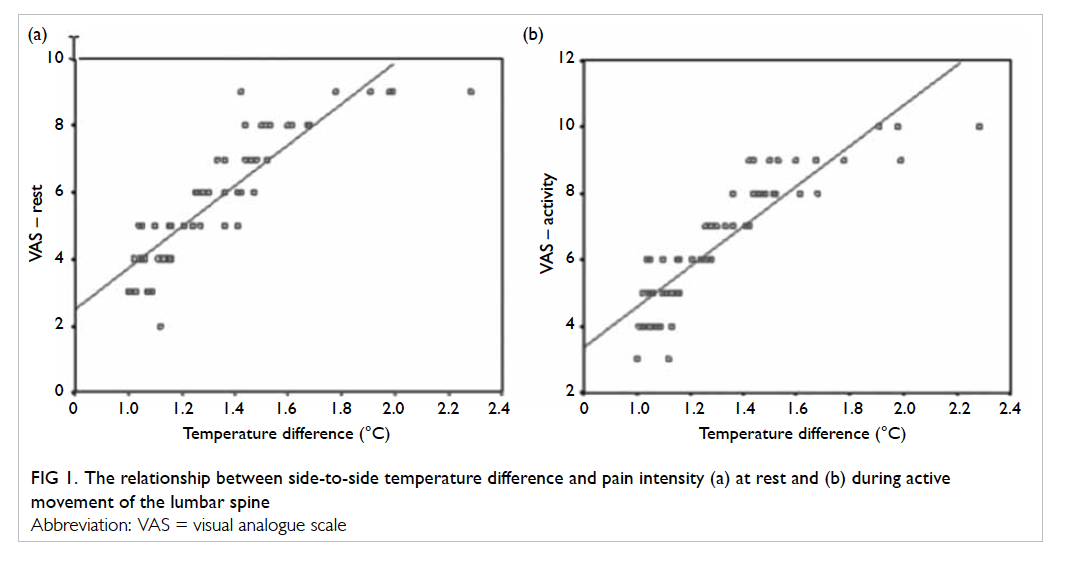
Figure 1. The relationship between side-to-side temperature difference and pain intensity (a) at rest and (b) during active movement of the lumbar spine
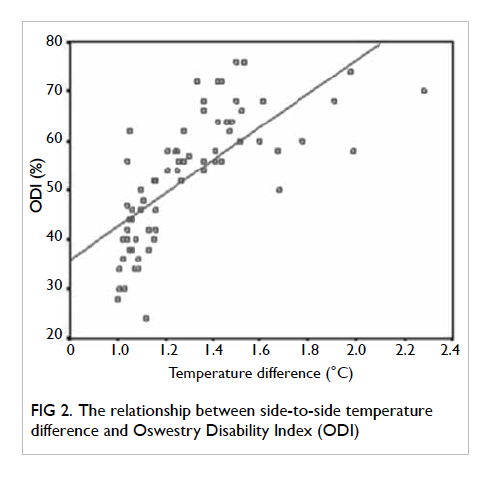
Figure 2. The relationship between side-to-side temperature difference and Oswestry Disability Index (ODI)
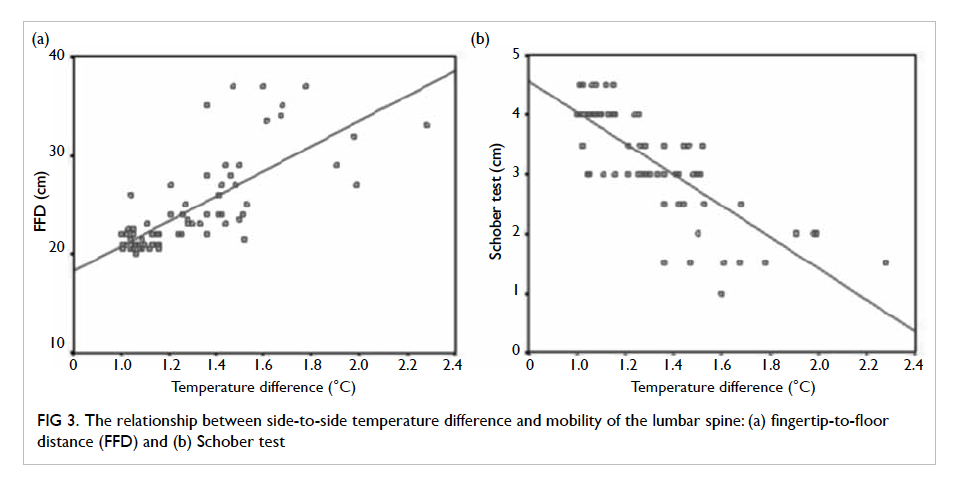
Figure 3. The relationship between side-to-side temperature difference and mobility of the lumbar spine: (a) fingertip-to-floor distance (FFD) and (b) Schober test
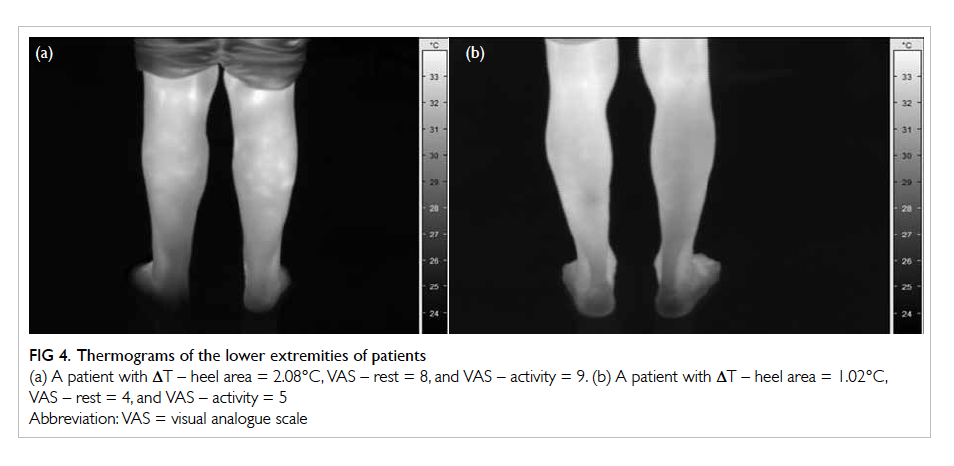
Figure 4. Thermograms of the lower extremities of patients
(a) A patient with ΔT – heel area = 2.08°C, VAS – rest = 8, and VAS – activity = 9. (b) A patient with ΔT – heel area = 1.02°C, VAS – rest = 4, and VAS – activity = 5
Discussion
The results of this study show that regional thermal
deficit, determined by thermography, is correlated
with pain intensity, lumbar spine mobility, and
functional status in patients with unilateral
lumbosacral radiculopathy.
Since the greatest amount of heat from the skin
surface is lost through emission of IR rays, IRT is
the method of choice that enables precise detection
and visualisation of changes in skin temperature.17
By detecting changes in skin temperature, IRT
can contribute to objective assessment of disease
that directly or indirectly affects the vascular
microcirculation tonus that is regulated by the
autonomous nervous system.4 18 Some studies have shown the significance of thermography in the
estimation of some painful conditions, including
radiculopathy.4 8 10 18 19 20
Contrary to the methods that estimate
radiculopathy on the basis of structural changes in
the spine or changes in spinal nerve root function,
IRT assesses radiculopathy based on a vasomotor
dysfunction. Its advantage in comparison with other
methods is its non-invasive, painless nature that
does not expose the patient to ionising radiation
and is also easy to use.4 18 21 In cases of bilateral
radiculopathy, false-negative results can be obtained
because of false temperature symmetry.7 22
Our research focused on the lower extremities,
similar to the majority of research on lumbosacral
radiculopathy within the field of thermography.6 7 10 11
Detection and visualisation of skin temperature
changes in the affected lower extremity was by IRT.
This detects IR rays emitted from the surface of the
body and then focuses and directs them by special
lenses towards a photosensor that transforms the
energy of the detected IR rays into electric impulses
and then into a visible recording—a thermogram. The
temperature emitted from the skin is thus visualised
on the screen in the form of colour spectrum.23
Development of information technology has
reduced the disadvantages of subjective estimation
of the intensity of colouration on the thermogram.
New-generation IR cameras show the temperature
asymmetry as high-quality thermograms and enable
a quantitative analysis.17 24
Qualitative analysis of the thermograms of
patients showed regional hypothermia of the affected
lower extremity, and has also been observed in other
studies.7 10 11 Regional hypothermia is considered
a consequence of the sympathetic vasoconstrictor
reflex that develops due to irritation of the
dorsal root of the spinal nerve.7 22 Some authors describe hypothermia as muscle atrophy caused by
denervation or inactivity.2 25
In our study, the regional thermal deficit of
the affected lower extremity did not follow the
distribution of a dermatome. A possible explanation
for this is that blood supply to the skin of the lower
extremities is quite different to the distribution
of sensory nerves in the same region.2 Therefore,
without additional information, it is not possible to
use IRT to determine the level of disc herniation.
Maximum values of ΔT have mostly been
recorded at the heel or plantar region of the foot. This
shows that vascular changes are more prominent
in the distal regions of the affected extremity. Our
results are similar to those obtained by Zaproudina
et al,22 who found a more significant correlation
between pain intensity and temperature asymmetry
in the plantar area of the foot in patients with low
back pain (LBP).
The present study showed a statistically
significant correlation between regional thermal
deficit values of the affected lower extremity and
radicular pain intensity. Our results are in accordance
with the results obtained by other authors, who
have observed a correlation between temperature
asymmetry and radicular pain, and show that IRT
can be effective in the objective differentiation of
the presence or absence of pain.5 7 9 10 In the present
study, analysis of the correlation between the
stated parameters demonstrated that the values of
thermal deficit increase along with increased pain
intensity (Fig 1). On the basis of this finding, it can
be concluded that thermograms provide not only
information about the existence of pain but also about
pain intensity. This correlation has been explained
as nociceptor excitation, the secondary consequence
of which is vasoconstriction.26 A positive correlation
between pain intensity and temperature asymmetry
of the affected lower extremity was also found in
research on patients with LBP,22 although other
researchers have found no clear correlation between
temperature asymmetry and radicular pain intensity.2
These different results can be partially explained by
the fact that the mentioned study established the
diagnosis of unilateral radiculopathy only on the
basis of clinical findings, while pathological findings
of electrophysiological examination were present
in only 43% of patients. In this study, MRI findings
showed disc herniation in 86% of patients, but in 30%
the herniation was central, and was not characterised
by nerve compression and concomitant muscle
denervation.2
It was also observed that higher values
of thermal deficit are correlated with worse
functional status of patients. The results of the ODI
questionnaire showed that the examined patients
had limited activities of daily living that was thought
to be a result of conditioning by the presence of pain.
The relationship of these parameters was also observed
in the study by Zaproudina et al22 on patients with
LBP.
The relationship between regional thermal deficit
and spine mobility shows that spine mobility is
reduced with increased values of thermal deficit.
The correlation between abnormal changes in skin
surface temperature and limited mobility has been
previously observed in a study that included patients
with pain syndrome in the pelvic-femoral region.27
Considering that the presence of pain can
account for limited mobility of the lumbar region of
the spine, as well as limited activities of daily living,
the most significant of all correlations is the one
between the regional thermal deficit of the affected
lower extremity and radicular pain intensity.
The results of our study should be considered
in light of the following limitations. The main
limitation is the absence of a control group. Future
research should address this. Another limitation
is that circadian rhythm and psychological factors
were not controlled. We believe that it has not
significantly affected our results, because we did not
analyse the absolute value of the temperature, but
only the temperature difference between the two
sides of the lower extremities.
Conclusions
Infrared thermography is a simple, non-invasive,
and painless method that can be used to estimate
neurovascular dysfunction in patients with unilateral
lumbosacral radiculopathy. The correlation between
thermal deficit and pain intensity is highly significant.
Estimation of pain intensity by VAS is a subjective
method, whereas determining the thermal deficit
is objective. The information obtained on the basis
of thermal deficit is significant as it provides an
objective assessment of radicular pain intensity.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Hsu PS, Armon C, Levin K. Lumbosacral radiculopathy:
pathophysiology, clinical features, and diagnosis. Available
from: http://cursoenarm.net/UPTODATE/contents/mobipreview.htm?25/35/26161?source=HISTORY.
Accessed 15 May 2015.
2. Ra JY, An S, Lee GH, Kim TU, Lee SJ, Hyun JK. Skin
temperature changes in patients with unilateral
lumbosacral radiculopathy. Ann Rehabil Med 2013;37:355-63. Crossref
3. Lee JH, Lee SH. Physical examination, magnetic resonance
image, and electrodiagnostic study in patients with
lumbosacral disc herniation or spinal stenosis. J Rehabil
Med 2012;44:845-50. Crossref
4. American Medical Association Council. Thermography in neurological and
musculoskeletal conditions. Thermol 1987;2:600-7.
5. Feng T, Zhao P, Liang G. Diagnostic significance of topical
image of infrared thermograph on the patient with lumbar
intervertebral disc herniation—a comparative study on 45
patients and 65 normal control [in Chinese]. Zhongguo
Zhong Xi Yi Jie He Za Zhi 1998;18:527-30.
6. Thomas D, Cullum D, Siahamis G, Langlois S. Infrared
thermographic imaging, magnetic resonance imaging, CT
scan and myelography in low back pain. Br J Rheumatol
1990;29:268-73. Crossref
7. Uematsu S, Jankel WR, Edwin DH, et al. Quantification of
thermal asymmetry. Part 2: Application in low-back pain
and sciatica. J Neurosurg 1988;69:556-61. Crossref
8. LaBorde TC. Thermography in diagnosis of radiculopathies.
Clin J Pain 1989;5:249-53. Crossref
9. Ping Z, You FT. Correlation study on infrared thermography
and nerve root signs in lumbar intervertebral disk
herniation patient: a short report. J Manipulative Physiol
Ther 1993;16:150-4. Erratum in: J Manipulative Physiol
Ther 1993;16:560.
10. Takahashi Y, Takahashi K, Moriya H. Thermal deficit
in lumbar radiculopathy. Correlations with pain and
neurologic signs and its value for assessing symptomatic
severity. Spine (Phila Pa 1976) 1994;19:2443-9. Crossref
11. Gillström P. Thermography in low back pain and sciatica. Arch Orthop Trauma Surg 1985;104:31-6. Crossref
12. Scott J, Huskisson EC. Graphic representation of pain. Pain
1976;2:175-84. Crossref
13. Perret C, Poiraudeau S, Fermanian J, Colau MM, Benhamou
MA, Revel M. Validity, reliability, and responsiveness
of the fingertip-to-floor test. Arch Phys Med Rehabil
2001;82:1566-70. Crossref
14. Rezvani A, Ergin O, Karacan I, Oncu M. Validity and
reliability of the metric measurements in the assessment
of lumbar spine motion in patients with ankylosing
spondylitis. Spine (Phila Pa 1976) 2012;37:E1189-96. Crossref
15. Fairbank JC, Pynsent PB. The Oswestry Disability Index.
Spine (Phila Pa 1976) 2000;25:2940-52. Crossref
16. Schwartz RG. Guidelines for neuromusculoskeletal
thermography. Thermol Int 2006;16:5-9.
17. Herry CL, Frize M. Quantitative assessment of pain-related
thermal dysfunction through clinical digital
infrared thermal imaging. BioMedical Engineering OnLine
2004. Available from: http://www.biomedical-engineering-online.com/content/3/1/19. Accessed 15 May 2015.
18. Hooshmand H, Hashmi M, Phillips EM. Infrared thermal
imaging as a tool in pain management—an 11 year study.
Part I of II. Thermol Inter 2001;11:53-65.
19. Cojocaru MC, Cojocaru IM, Cojan Carlea NA, Cinteza D,
Berteanu M. Infrared thermography—a tool for computer
assisted research in rehabilitation medicine. Appl Mech
Mater 2015;772:603-7. Crossref
20. Lahiri BB, Subramainam B, Jayakumar T, Philip J. Medical
applications of infrared thermography: a review. Infrared
Phys Technol 2012;55:221-35. Crossref
21. Nahm FS. Infrared thermography in pain medicine. Korean
J Pain 2013;26:219-22. Crossref
22. Zaproudina N, Ming Z, Hänninen OO. Plantar infrared
thermography measurements and low back pain intensity. J Manipulative Physiol Ther 2006;29:219-23. Crossref
23. Tkachenko YA, Golovanova M, Ovechkin AM. Clinical
thermography [in Russian]. Nizhny Novgorod: Union of
Western and Oriental Medicine; 1998.
24. Uematsu S, Edwin DH, Jankel WR, Kozikowski J, Trattner
M. Quantification of thermal asymmetry. Part 1: Normal
values and reproducibility. J Neurosurg 1988;69:552-5. Crossref
25. Hyun JK, Lee JY, Lee SJ, Jeon JY. Asymmetric atrophy of
multifidus muscle in patients with unilateral lumbosacral
radiculopathy. Spine (Phila Pa 1976) 2007;32:E598-602. Crossref
26. Conwell T. Distinct IR signatures result from neuropathic
abnormalities of the limbs. Thermol Int 2013;23:34-5.
27. Gabrhel J, Popracová Z, Tauchmannová H, Chvojka Z.
Thermal findings in pain syndromes of the pelvic-femoral
region. Thermol Int 2013;23:157-63.