Hong Kong Med J 2016 Apr;22(2):116–23 | Epub 29 Jan 2016
DOI: 10.12809/hkmj154566
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Haemodynamic changes in emergency
department patients with poorly controlled
hypertension
Stewart SW Chan, MSc, FHKAM (Emergency Medicine);
Mandy M Tse, BSc, MPhil;
Cangel PY Chan, PhD;
Marcus CK Tai, MB ChB, FHKAM (Emergency Medicine);
Colin A Graham, FRCPEd, FHKAM (Emergency Medicine);
Timothy H Rainer, FHKAM (Emergency Medicine), FIFEM
Accident and Emergency Medicine Academic Unit, Prince of Wales
Hospital, The Chinese University of Hong Kong, Shatin, Hong Kong
 Full
paper in PDF
Full
paper in PDF
Figure 1. Collection of haemodynamic data in the emergency department using the Ultrasonic Cardiac Output Monitor
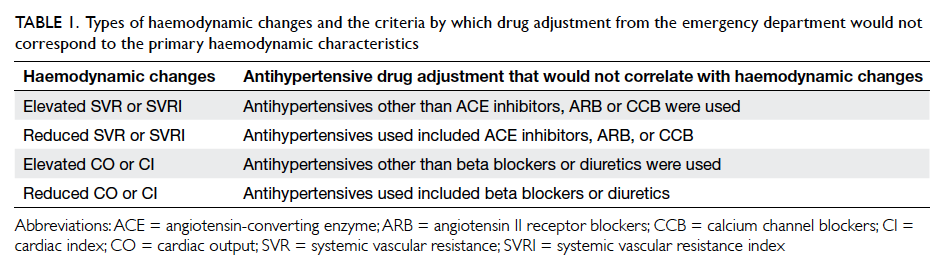
Table 1. Types of haemodynamic changes and the criteria by which drug adjustment from the emergency department would not correspond to the primary haemodynamic characteristics
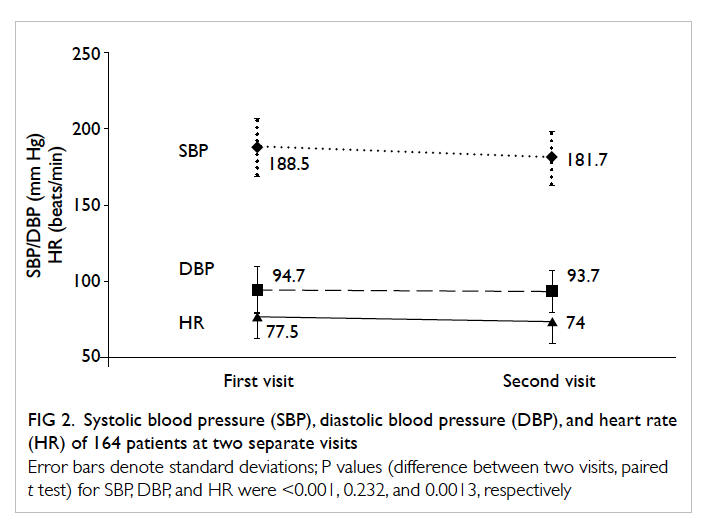
Figure 2. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) of 164 patients at two separate visits
Error bars denote standard deviations; P values (difference between two visits, paired t test) for SBP, DBP, and HR were <0.001, 0.232, and 0.0013, respectively
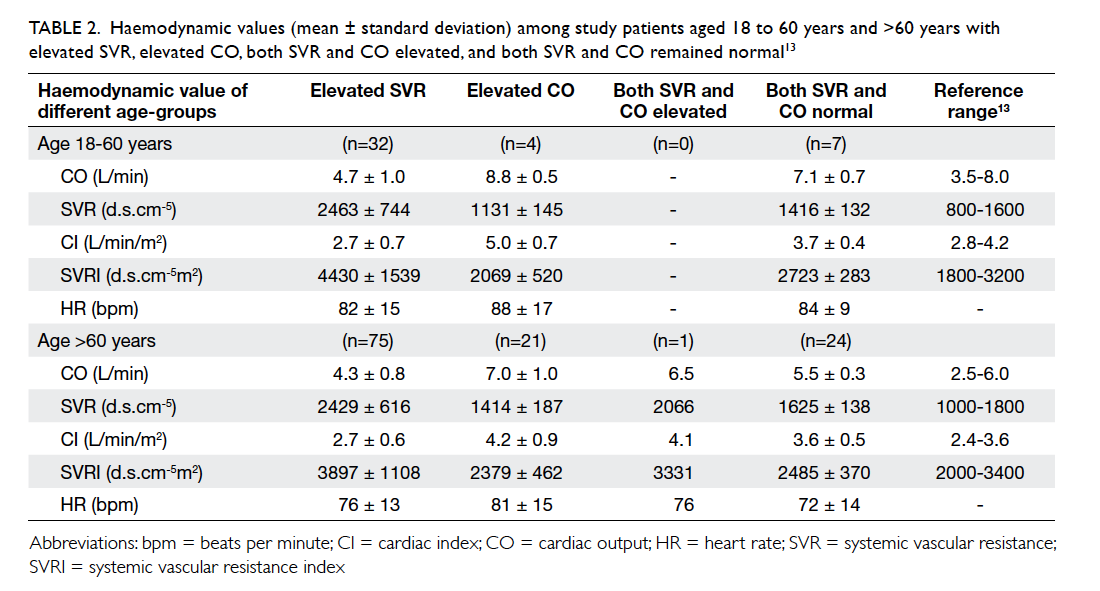
Table 2. Haemodynamic values (mean ± standard deviation) among study patients aged (a) 18 to 60 years and (b) >60 years with elevated SVR, elevated CO, both SVR and CO elevated, and both SVR and CO remained normal13
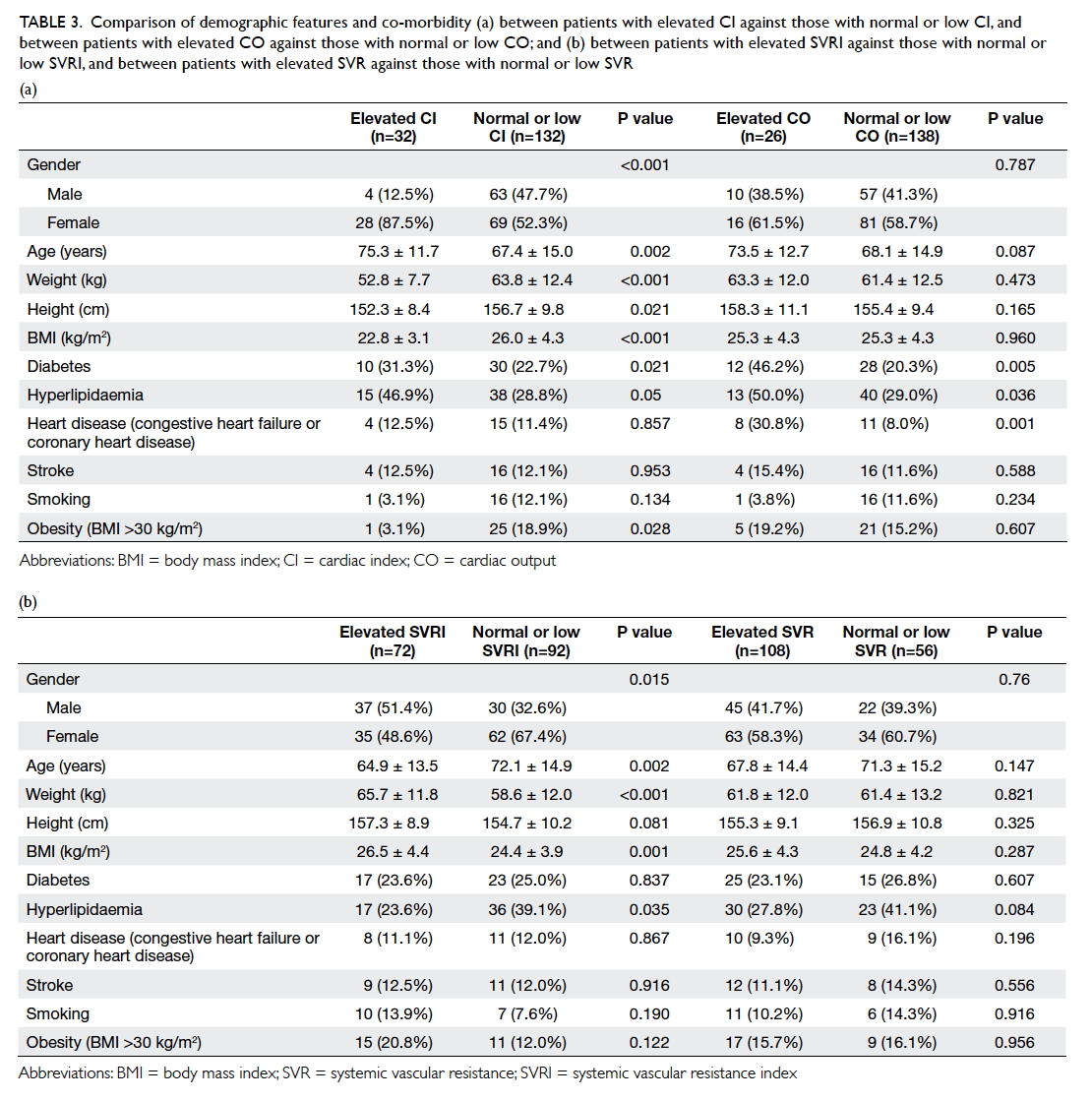
Table 3. Comparison of demographic features and co-morbidity (a) between patients with elevated CI against those with normal or low CI, and between patients with elevated CO against those with normal or low CO; and (b) between patients with elevated SVRI against those with normal or low SVRI, and between patients with elevated SVR against those with normal or low SVR
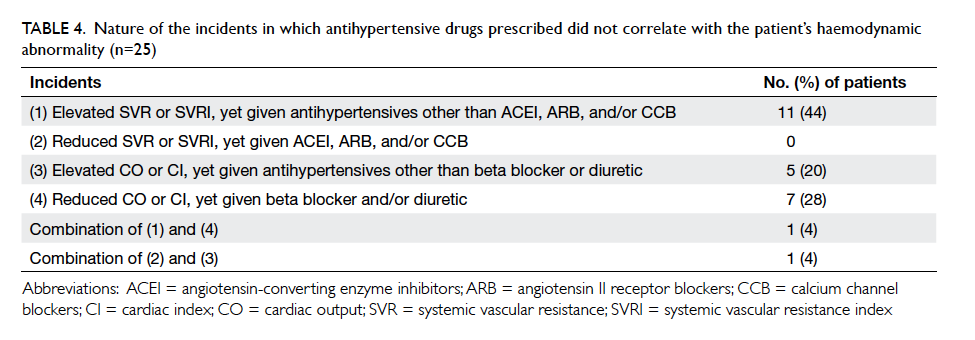
Table 4. Nature of the incidents in which antihypertensive drugs prescribed did not correlate with the patient’s haemodynamic abnormality (n=25)
Corresponding author: Dr Stewart SW Chan (stewart_chan@hotmail.com)
Abstract
Objectives: This study aimed to measure cardiac
output, systemic vascular resistance, cardiac index,
and systemic vascular resistance index in emergency
department patients with poorly controlled
hypertension; and to determine the frequency
in which antihypertensive drugs prescribed do not address the predominant haemodynamic
abnormality.
Methods: This cross-sectional observational study was conducted in an emergency department of a 1400-bed tertiary hospital in Hong Kong. Patients aged 18 years or above, with systolic blood pressure of ≥160 mm Hg or diastolic blood pressure of ≥100 mm Hg based on two or more measurements and on two separate occasions within 2 to 14 days, were included. Haemodynamic measurements were obtained using a non-invasive Doppler ultrasound monitor. Doctors were blinded to the haemodynamic data. Any antihypertensive medication adjustment was evaluated for correlation with haemodynamic changes.
Results: Overall, 164 patients were included. Their
mean age was 69.0 years and 97 (59.1%) were
females. Systemic vascular resistance and cardiac
output were elevated in 65.8% (95% confidence
interval, 57.9-72.9%) and 15.8% (10.8-22.5%) of patients,
respectively. Systemic vascular resistance index
and cardiac index were elevated in 43.9% (95%
confidence interval, 36.2-51.8%) and 19.5% (13.9-26.5%)
of patients, respectively. Of 71 patients in whom
antihypertensive medications were adjusted, 25
(35.2%; 95% confidence interval, 24.5-47.5%) were
prescribed agents that did not correlate with the
primary haemodynamic abnormality.
Conclusions: The profile of haemodynamic changes
in emergency department patients with poorly
controlled hypertension is characterised. The antihypertensive drugs prescribed did not correspond to the
patient’s primary haemodynamic derangement in
35% of cases.
New knowledge added by this study
- This is the first study to delineate the haemodynamic characteristics of Hong Kong emergency department (ED) patients with poorly controlled hypertension.
- Antihypertensive drugs prescribed in the ED did not correlate with the patient’s primary haemodynamic derangement in 35% of cases.
- A haemodynamically guided approach to drug therapy should be further investigated as it may lower blood pressure more effectively in a large proportion of patients.
Introduction
Hypertension is an important risk factor for
cardiovascular disease, cardiovascular events, and
death. It was estimated that in the year 2000, 972
million adults in the world had hypertension, and
that by 2025, this number will increase by 60%.1
Within the US, from 2009 to 2010, 29.5% of adults
were affected by hypertension, of whom only 45.1%
had blood pressure (BP) under control, which is
below 140/90 mm Hg.2 Uncontrolled hypertension is
present in about 69%, 77%, and 74% of patients with
a first myocardial infarction, patients with a first
stroke, and patients with congestive heart failure,
respectively.3 Blood pressure control is an important
factor in preventing or delaying the development
of end-stage renal disease and congestive heart
failure and also relieves symptoms associated with
congestive heart failure.4 5 Control of hypertension is
also essential in stroke prevention.6
Hypertension is associated with increased
cardiac output (CO) and/or increased systemic
vascular resistance (SVR), according to the
relationship: BP = CO x SVR.7 Clarification of the
associated haemodynamic pathophysiology of
hypertensive patients may allow a more tailored
choice of antihypertensive drugs, resulting in more
effective BP control. Patients with elevated CO may
benefit more from primary treatment with agents
that lower CO, while patients with elevated SVR may
benefit more from primary treatment with agents
that reduce SVR. This haemodynamically guided
approach is feasible in the clinical setting, provided
there is a simple and accurate method of measuring
CO and SVR. These parameters are readily obtained
non-invasively at the point-of-care by the Ultrasonic
Cardiac Output Monitor (USCOM; USCOM Ltd,
Sydney, Australia) that uses continuous-wave
Doppler ultrasound transcutaneously to detect the
velocity of blood flowing through the aortic valve or
pulmonary valve.8 9 The time to read out is less than
3 minutes.
In current practice, doctors who encounter
patients with poorly controlled hypertension are
often unable to choose an antihypertensive agent
with respect to the pattern of haemodynamic
derangement. This is particularly relevant in the
emergency department (ED) because, according to
a report from the US Centers for Disease Control
and Prevention and National Center for Health
Statistics, BP is severely elevated (with systolic
BP of ≥160 mm Hg or diastolic BP of ≥100 mm Hg)
in 16.3% of ED visits.10 We therefore aimed to
investigate the haemodynamic changes in this
group of ED patients with severely elevated, poorly
controlled hypertension, and to determine whether
antihypertensive drugs prescribed to them correlate
with these changes.
This study aimed to measure the CO, SVR,
cardiac index (CI), and SVR index (SVRI) in ED
patients with poorly controlled hypertension. It
also aimed to determine the frequency with which
antihypertensive medications prescribed in the
ED setting did not correspond to the predominant
haemodynamic abnormality for such patients.
Methods
Our setting was an academic ED of a 1400-bed
tertiary hospital in Hong Kong, with an annual ED
attendance of over 150 000 cases. Patients aged 18
years or above, with systolic BP of ≥160 mm Hg or
diastolic BP of ≥100 mm Hg based on two or more
BP measurements at least 20 minutes apart and on
two separate occasions within 2 to 14 days, were
included in the study. Patients were excluded if they
were pregnant or lactating, and if they presented
with a hypertensive emergency such as stroke.
Patients’ haemodynamic profile was obtained
by using USCOM. A transducer was placed
transcutaneously in either the left parasternal
position to measure blood flow through the
pulmonary valve, or the suprasternal position to
measure blood flow through the aortic valve. The
approach giving a tracing that better fulfilled the
optimal Doppler flow profile characteristics was
chosen. Measures of CO, CI, SVR, and SVRI were
obtained by trained operators as shown in Figure 1, with patients examined supine and after 5 minutes’ resting. Stroke volume (SV) and heart rate (HR)
were measured by USCOM, with CO calculated as
the product of SV and HR; SVR was then obtained
according to the relationship: SVR = mean arterial
pressure/CO. The SVRI and CI are SVR and CO
respectively normalised for body surface area.
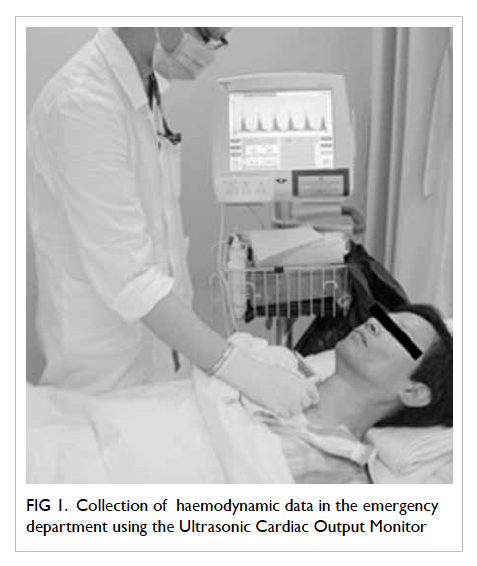
Figure 1. Collection of haemodynamic data in the emergency department using the Ultrasonic Cardiac Output Monitor
For the purpose of recruiting patients, BP was
measured with an appropriately sized cuff using
a standard oscillometric device with the patient
in a sitting position, unless precluded by physical
condition, according to the US National Heart,
Lung, and Blood Institute recommendation.11 After
prospective patients had been recruited, for the
purpose of haemodynamic calculations, the supine
position was used for BP measurement just before
the acquisition of haemodynamic data, according to
standard operating instructions and specifications of
the machine. This supine BP reading was manually
entered into the USCOM device for subsequent
computations. Demographic, anthropometric,
and clinical data such as co-morbidity and current
medications were also collected and entered
into a database. The ED physicians were blinded
to the haemodynamic profile of patients and
all antihypertensive medication changes were
documented. These ED doctors did not follow any
particular set of practice guidelines or study protocol
when they made medication changes, but managed
each individual case according to their own clinical
judgement, as they would in their everyday practice.
All patients were recruited from 9:00 am to 5:00
pm, Monday to Friday, over a consecutive 9-month
period. They were followed up as clinically indicated
within 2 to 14 days. This was essentially a single-centre
cross-sectional study as far as the first objective was
concerned. The prospective observational follow-up
assessments ensured that patients with elevated BP
who fulfilled the inclusion criteria at the first visit, but
whose elevated BP was not sustained at the follow-up
visit, could be excluded from the study. Approval
from the Clinical Research Ethics Committee of
the authors’ institution was obtained prior to study
commencement. All patients gave written consent to
participate with full knowledge of the nature of this
research.
Statistical analyses
The primary outcome measure was the CO estimated
by USCOM. Although our literature search failed to
identify any USCOM-derived range for CO values
in hypertensive patients, the reference range for
healthy subjects aged 16 to 60 years is reported
to be 3.5 to 8.0 L/min. Assuming that this follows
a normal distribution, with the upper and lower
values defining the 95% confidence interval, the
standard deviation (SD) was calculated to be 1.13.
The total width of the confidence interval desired
was 0.4 L/min. For a confidence level of 95%, the
required sample size was thus estimated to be 126.12
Continuous variables were analysed using unpaired
2-tailed t test or paired t test where appropriate, and
categorical data were analysed using the Chi squared
test or Fisher’s exact test. Stepwise logistic regression
analysis was used to identify independent predictors
of patients with elevated CO, CI, SVR, and SVRI.
Variables were entered into the model if P<0.05. All
data were analysed using the Statistical Package for
the Social Sciences (Windows version 18.0; SPSS
Inc, Chicago [IL], US), and MedCalc version 11.5.1
(MedCalc Software; Mariakerke, Belgium).
Evaluation of the correlation between
haemodynamic profile and antihypertensive
drug
The second part of the study was a retrospective
review of prospectively collected data. We
investigated five different classes of antihypertensive
drugs: angiotensin-converting enzyme (ACE)
inhibitors, angiotensin II receptor blockers (ARBs),
calcium channel blockers (CCBs), beta blockers,
and diuretics. Each patient’s antihypertensive
medication was assessed against a theoretical model
of guidance based on measured haemodynamic
abnormality of the patient. The protocol is illustrated
in Table 1, and shows the types of haemodynamic change, the corresponding optimal antihypertensive
drug selection, and the criteria by which the actual
drug selected would not correspond to the primary
haemodynamic characteristics. For each case in
which antihypertensive drugs were identified as
not correlating with the primary haemodynamic
abnormality, the case notes were reviewed to ensure
that the choice of medication was not influenced
or limited by known drug allergies or a history of
adverse drug reactions to the more appropriate drug
class.
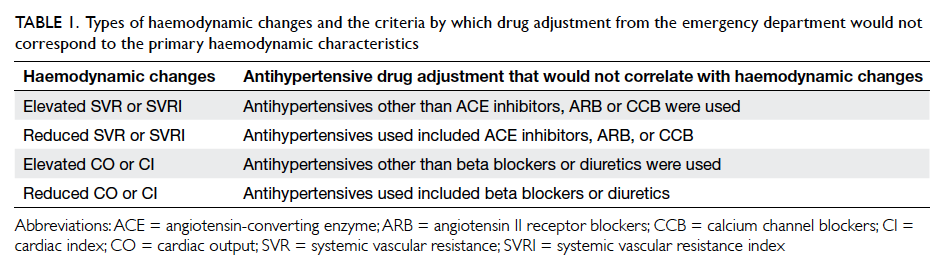
Table 1. Types of haemodynamic changes and the criteria by which drug adjustment from the emergency department would not correspond to the primary haemodynamic characteristics
Results
Of 232 patients who were assessed for the study, 68
patients were excluded (9 defaulted follow-up, 54
with BP <160/100 mm Hg at follow-up, and 5 with
unsuccessful USCOM measurements), leaving a total
of 164 patients. The mean age was 69.0 (SD, 14.7)
years, with a median of 72 years and interquartile
range of 21.3 years. Of the patients, 97 (59.1%) were
females. The mean body mass index (BMI) was 25.3
kg/m2 (SD, 4.3; range, 16.1-42.3 kg/m2). The mean
body weight was 67.7 kg (SD, 10.8; range, 42.6-92.9
kg) for males, and 57.5 kg (SD, 11.8; range, 34.4-116.2 kg) for females. The mean height was 164.1 cm
(SD, 7.2; range, 149-186 cm) for males, and 150.2 cm
(SD, 6.7; range, 136.2-172.3 cm) for females. Systolic
and diastolic BP values together with HR from
two separate visits are shown in Figure 2. Of the 164 patients included, with regard to confounding
factors that might increase BP, 67 (40.9%) had
complained of pain, 13 (7.9%) had an injury, two (1.2%)
had symptoms of anxiety, 14 (8.5%) had an infection,
and seven (4.3%) presented with fever. For the 14 cases
with infection, the sources of infection were soft
tissue (n=5), gastrointestinal tract (n=4), upper
respiratory tract (n=3), lower respiratory tract (n=1),
and urinary tract (n=1). With regard to co-morbidity,
40 (24.4%) patients also had diabetes, 53 (32.3%) had
hyperlipidaemia, 19 (11.6%) had heart disease, and
20 (12.2%) had a history of stroke. Of the patients, 46
(28.0%) were never diagnosed to have hypertension.
In addition, 20 (12.2%) patients were smokers and 26
(15.9%) were obese (BMI >30 kg/m2).
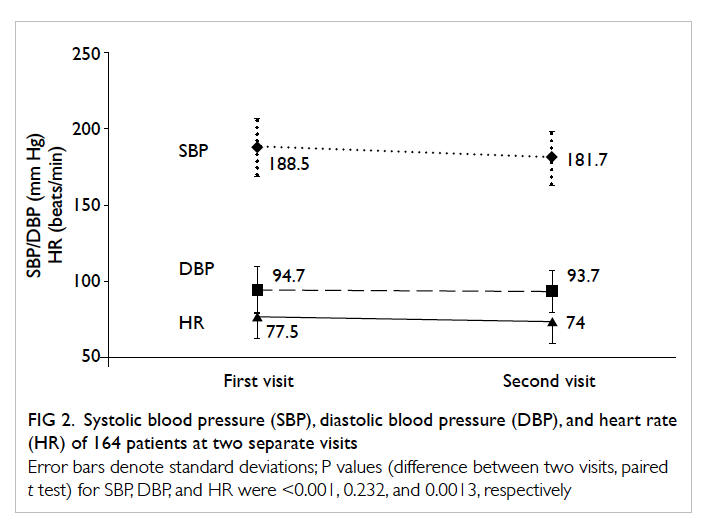
Figure 2. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) of 164 patients at two separate visits
Error bars denote standard deviations; P values (difference between two visits, paired t test) for SBP, DBP, and HR were <0.001, 0.232, and 0.0013, respectively
The SVR was elevated above reference range
in 65.8% (95% confidence interval, 57.9-72.9%) of
patients, while CO was elevated above reference
range in 15.8% (10.8-22.5%) of patients. Similarly,
SVRI was elevated above reference range in 43.9%
(95% confidence interval, 36.2-51.8%) of patients,
while CI was elevated above reference range in 19.5%
(13.9-26.5%) of patients. Only one patient had both
SVR and CO elevated, while none of the patients had
both SVRI and CI elevated.
Table 213 shows the haemodynamic values
(mean ± SD) of study patients grouped according to
associated pathophysiology.
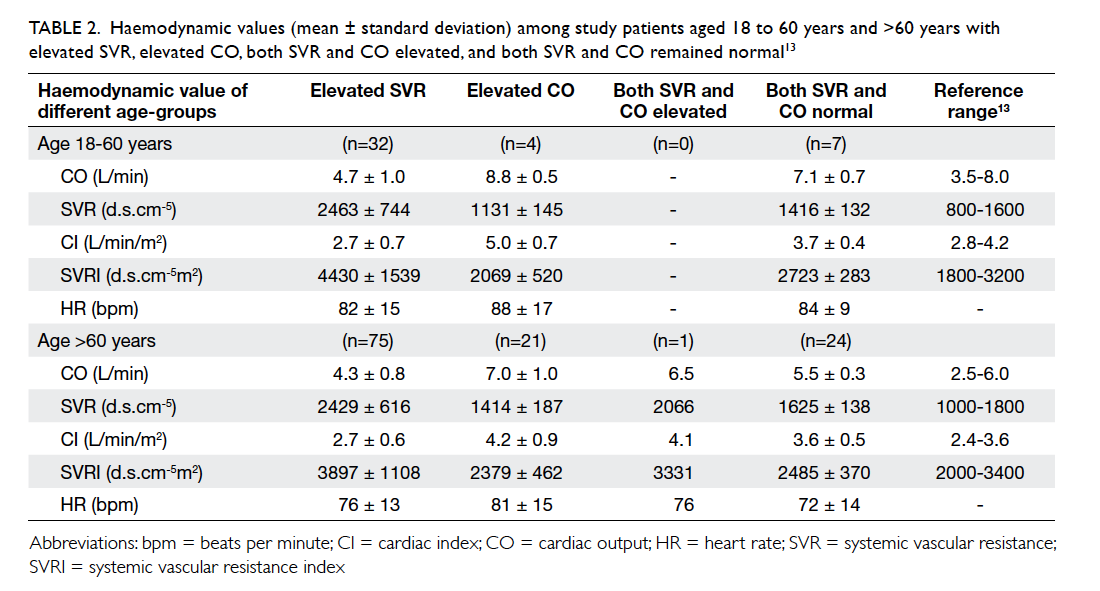
Table 2. Haemodynamic values (mean ± standard deviation) among study patients aged (a) 18 to 60 years and (b) >60 years with elevated SVR, elevated CO, both SVR and CO elevated, and both SVR and CO remained normal13
Patients with elevated CI (n=32) compared
with those with normal or low CI (n=132) were
more likely to be female (87.5% vs 52.3%; P<0.001),
older (mean age ± SD, 75.3 ± 11.7 years vs 67.4 ±
15.0 years; P=0.002), have lower body weight (52.8
± 7.7 kg vs 63.8 ± 12.4 kg; P<0.001), shorter stature
(152.3 ± 8.4 cm vs 156.7 ± 9.8 cm; P=0.021), and have
significantly lower BMI (22.8 ± 3.1 kg/m2 vs 26.0 ±
4.3 kg/m2; P<0.001) [Table 3a].
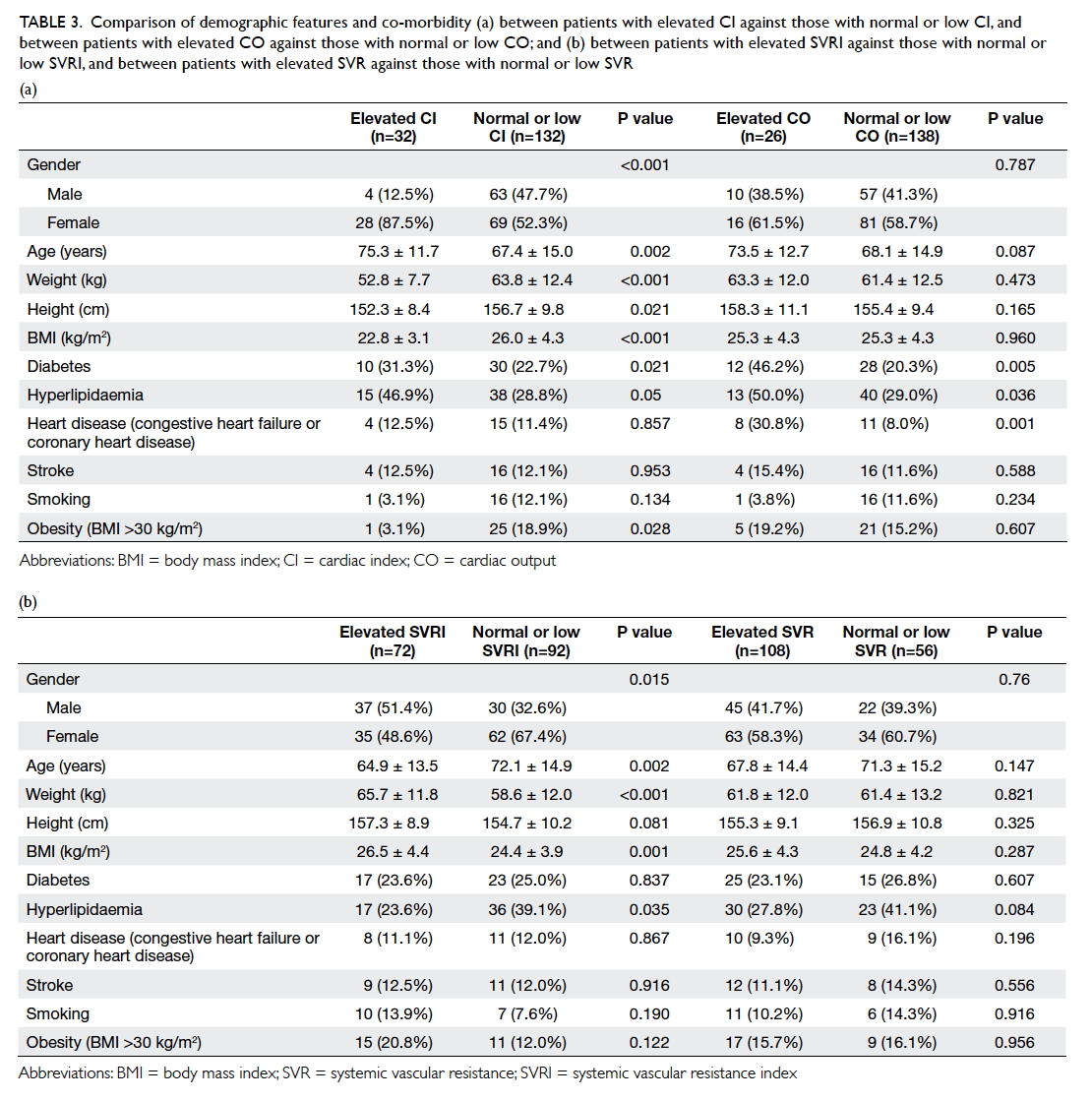
Table 3. Comparison of demographic features and co-morbidity (a) between patients with elevated CI against those with normal or low CI, and between patients with elevated CO against those with normal or low CO; and (b) between patients with elevated SVRI against those with normal or low SVRI, and between patients with elevated SVR against those with normal or low SVR
Patients with elevated SVRI (n=72) compared
with those with normal or low SVRI (n=92) were
more likely to be male (51.4% vs 32.6%; P=0.015),
younger (mean age ± SD, 64.9 ± 13.5 years vs 72.1 ±
14.9 years; P=0.002), have higher body weight (65.7 ±
11.8 kg vs 58.6 ± 12.0 kg; P<0.001), and significantly
higher BMI (26.5 ± 4.4 kg/m2 vs 24.4 ± 3.9 kg/m2;
P=0.001) [Table 3b].
Using stepwise logistic regression analysis,
independent predictors of elevated CI were: age >70
years (odds ratio [OR]=2.80; 95% confidence interval,
1.11-7.05) and female gender (5.64; 1.81-17.5) after
the model was adjusted for current smoker, diabetes,
heart disease, hypertension, and stroke. Age above
70 years was an independent negative predictor
of elevated SVRI with an OR of 0.32 (95% confidence
interval, 0.16-0.61) after the model was adjusted
for sex, current smoker, diabetes, heart disease,
hypertension, and stroke.
Doctors in ED initiated or added
antihypertensive medications in 71 (43.3%) of the
164 cases. These were given as a new prescription in
20 cases, as adjustment of usual medication regimen
in 48 cases, and as resumption of omitted treatment
in three cases. The added drugs were given as
monotherapy in 22 cases, and as combination therapy
in 31 cases. In 22 cases, the dosage of existing drugs
was increased. The drugs were all prescribed until
follow-up.
Of these 71 cases, 25 (35.2%; 95% confidence
interval, 24.5-47.5%) were prescribed agents that
did not correspond to the primary haemodynamic
derangement. Chart review for each of these cases
showed that the choice of medication was not
influenced or limited by known drug allergies or a
history of adverse drug reactions to the appropriate
drug class. Table 4 shows how the choice of medication did not correlate with haemodynamic
abnormalities in these 25 patients. The most frequent
cause or scenario occurred in patients with elevated
SVR or SVRI who were given antihypertensive
drugs other than ACE inhibitors, ARBs, or CCBs.
There were 11 such cases, representing 15.5% (95%
confidence interval, 8.9%-25.7%) of the 71 cases in
which medications were adjusted.
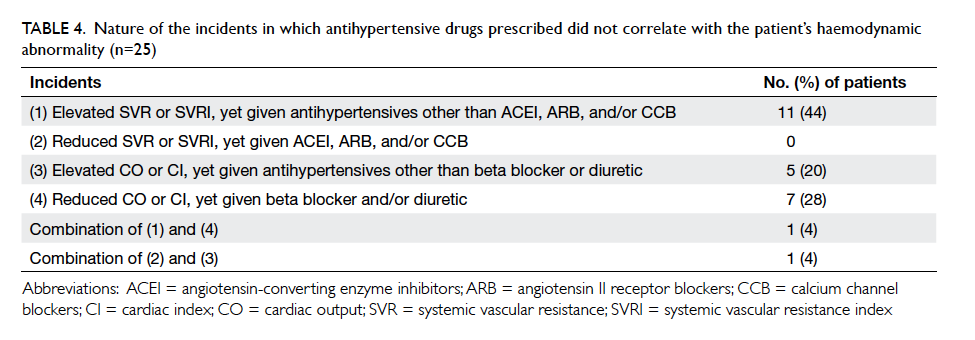
Table 4. Nature of the incidents in which antihypertensive drugs prescribed did not correlate with the patient’s haemodynamic abnormality (n=25)
Discussion
Blood pressure control is an important and
cost-effective means of reducing cardiovascular
events, with their associated work absenteeism,
loss of productivity, and hospitalisations.4 5 6 14
According to the relationship that BP = CO x SVR,
the pharmacotherapy of hypertension may be
much improved by delineating and targeting the
associated primary haemodynamic derangements
that can be a relative elevation of CO or SVR or
both. Just as the latest US and UK national guidelines
for the management of hypertension have both
recommended selection of antihypertensive agent
based on associated factors such as age, ethnicity
(black population) and co-morbid illnesses (chronic
kidney disease and heart failure); selection based
on haemodynamic pattern may also be considered
in order to optimise BP control.15 16 It has been
shown that guiding antihypertensive therapy using
haemodynamic parameters measured by impedance
cardiography results in improved BP control in the
primary care setting.17 18 This same approach also
improved BP control for patients with resistant
hypertension in a hypertension specialty clinic.19
Although these studies were promising, their results
might not be extrapolated to the ED setting. To
the best of our knowledge, our study is the first in
indexed literature to delineate the pathophysiologic
haemodynamic patterns of hypertensive patients in
the ED setting upon which future research can be
based.
In our study, there were approximately 4 times
as many patients with elevated SVR as elevated CO,
and slightly more than twice as many patients with
elevated SVRI than with elevated CI. Approximately
one third of patients with deranged haemodynamic
parameters (32/104) have elevated CI. Thus, the proportion
of patients with elevated CO or CI, although less
than patients with elevated SVR or SVRI, is still
considerable. For these patients, antihypertensive
therapy that aims to reduce CO may in theory be
more effective than other agents. Diuretics and beta blockers,
which primarily act to reduce CO, may
therefore still play important roles. Nevertheless the
current UK guidelines have not included diuretics
and beta blockers as first-line drugs; while the
current US guidelines have not included a beta
blocker as a first-line drug.15 16 In contrast, both
the current European and Canadian hypertension
guidelines retain diuretics and beta blockers as first-line
options, and the results from our study appear
to support this.20 21
In this study setting, patients with elevated CI
were more likely to be older, female, and have lower
body weight, height and BMI, while those with
predominantly elevated SVRI were more likely to be
younger, male, and have higher body weight and
BMI.
For patients included in our study, the
initiation of pharmacologic treatment was in
keeping with the latest US National Heart, Lung,
and Blood Institute recommendations.15 Doctors in ED needed to initiate or step up therapy in
43% of patients in this study. Of these, about 35%
were given an antihypertensive drug that did not
correlate with their underlying haemodynamic
abnormality. These results suggest that using non-invasive
haemodynamic measurements to guide
treatment in the ED may optimise the choice of
medication for hypertensive patients. Studies have
shown that emergency physicians cannot accurately
estimate the underlying haemodynamic profile
of acutely ill patients.22 23 There are several non-invasive haemodynamic measuring devices available
on the market. The Nexfin (BMEYE, Amsterdam,
The Netherlands) utilising a finger-cuff technology
based on the pulse-contour method can also be
conveniently applied in the ED setting.22 23 As for
impedance cardiography, some work has already
been done in ED patients with congestive heart
failure and non-ED patients with hypertension;
nonetheless more work still needs to be done in ED
hypertensive patients.17 18 19 23
Limitations
It is important to acknowledge that to date, there
has been little evidence that, in the ED setting,
adjusting antihypertensive medications based on
haemodynamic parameters can improve long-term
BP control or cardiovascular outcome. There are two
other limitations to our study. First, as this study was
designed for and conducted in the ED setting, patients
may often have presented with injury, pain, anxiety,
infections, fever, and other factors that could give
rise to transiently elevated BP up to 160/100 mm Hg
or above. White coat hypertension is also a potential
source of bias. This is indeed the same kind of clinical
scenario that ED doctors in practice need
to manage, in which the elevated BP often requires
further observation before a decision for drug
intervention can be made. In our study protocol, this
period of observation ranged from 2 to 14 days, and
we excluded patients with severely elevated BP that
was not sustained. As a result, 54 (23%) of the 232
initially recruited patients were excluded. We believe
that by obtaining BP measurements on two separate
occasions, we have excluded most of the patients
affected by factors causing transient hypertension.
We did not choose a hypertension out-patient clinic
to recruit our subjects because our intention was to
obtain results that can be directly relevant for ED
doctors. Second, many patients who present to the
ED are already on concomitant antihypertensive
drugs that can affect their haemodynamic values.
Although we were aware of this confounding factor,
we did not aim to study the correlation, nor did we
subject our study patients to drug washout periods.
In our study, 121 (74%) patients were on concomitant medications that might influence
haemodynamic values. Regardless of whether or not
patients are already on antihypertensive medications,
defining haemodynamic derangement would still be
valuable in guiding decision-making for the choice
of antihypertensive drug at the point-of-care, be it
introducing a first-line drug, adding a different drug
for combination therapy, or increasing the dose of an
existing drug.
Conclusions
This study identified the profile of haemodynamic
characteristics in Hong Kong ED patients with
poorly controlled hypertension. Antihypertensive
drugs prescribed in the ED did not correlate with the
patient’s primary haemodynamic derangement in
approximately 35% of cases. Therefore, a potential exists for
optimising treatment by a haemodynamically guided
approach to drug selection. A randomised controlled
trial is needed to prove if such an approach will
indeed result in better BP control, achievement of
haemodynamic normalisation, and better outcomes.
References
1. Kearney PM, Whelton M, Reynolds K, Muntner P,
Whelton PK, He J. Global burden of hypertension: analysis
of worldwide data. Lancet 2005;365:217-23. Crossref
2. Guo F, He D, Zhang W, Walton RG. Trends in prevalence,
awareness, management, and control of hypertension
among United States adults, 1999 to 2010. J Am Coll
Cardiol 2012;60:599-606. Crossref
3. Lloyd-Jones D, Adams R, Carnethon M, et al. Heart
disease and stroke statistics—2009 update: a report from
the American Heart Association Statistics Committee and
Stroke Statistics Subcommittee. Circulation 2009;119:e21-181. Crossref
4. Sarnak MJ, Greene T, Wang X, et al. The effect of a lower
target blood pressure on the progression of kidney disease:
long term follow-up of the Modification of Diet in Renal
Disease Study. Ann Intern Med 2005;142:342-51. Crossref
5. Krum H, Jelinek MV, Stewart S, Sindone A, Atherton JJ;
National Heart Foundation of Australia; Cardiac Society of
Australia and New Zealand. 2011 Update to National Heart
Foundation of Australia and Cardiac Society of Australia
and New Zealand Guidelines for the prevention, detection
and management of chronic heart failure in Australia,
2006. Med J Aust 2011;194:405-9.
6. Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction
and secondary prevention of stroke and other vascular
events: a systematic review. Stroke 2003;34:2741-8. Crossref
7. Victor RG. Systemic hypertension: mechanisms and
diagnosis. In: Bonow RO, Mann DL, Zipes DP, et al, editors.
Braunwald’s heart disease: a textbook of cardiovascular
medicine. 9th ed. Philadelphia, US: Elsevier; 2011: 935-54.
8. Meyer S, Todd D, Wright I, Gortner L, Reynolds G. Review
article: Non-invasive assessment of cardiac output with
portable continuous-wave Doppler ultrasound. Emerg
Med Australas 2008;20:201-8. Crossref
9. Chong SW, Peyton PJ. A meta-analysis of the accuracy
and precision of the ultrasonic cardiac output monitor
(USCOM). Anaesthesia 2012;67:1266-71. Crossref
10. Niska RW. Blood pressure measurements at emergency
department visits by adults: United States, 2007-2008.
NCHS Data Brief 2011;72:1-8.
11. The National Heart, Lung, and Blood Institute. National
Institutes of Health. The Seventh Report of the Joint
National Committee on prevention, detection, evaluation,
and treatment of high blood pressure. Available from: http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed 11
Mar 2015.
12. Browner WS, Newman TB, Cummings SR, et al. Estimating
sample size and power: the nitty gritty. In: Hulley SB,
Cummings SR, Browner WS, et al, editors. Designing
clinical research. 2nd ed. Philadelphia, US: Lippincott
Williams & Wilkins; 2001: 65-91.
13. Smith BE. The USCOM in clinical practice. Sydney:
USCOM; 2007.
14. Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang
S, Lynch W. Health, absence, disability, and presenteeism
cost estimates of certain physical and mental health
conditions affecting U.S. employers. J Occup Environ Med
2004;46:398-412. Crossref
15. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based
guideline for the management of high blood pressure
in adults: report from the panel members appointed to
the Eighth Joint National Committee (JNC 8). JAMA
2014;311:507-20. Crossref
16. Krause T, Lovibond K, Caulfield M, McCormack T,
Williams B; Guideline Development Group. Management
of hypertension: summary of NICE guidance. BMJ
2011;343:d4891. Crossref
17. Flack JM. Noninvasive hemodynamic measurements: an
important advance in individualizing drug therapies for
hypertensive patients. Hypertension 2006;47:646-7. Crossref
18. Smith RD, Levy P, Ferrario CM; Consideration of
Noninvasive Hemodynamic Monitoring to Target
Reduction of Blood Pressure Levels Study Group.
Value of noninvasive hemodynamics to achieve blood
pressure control in hypertensive subjects. Hypertension
2006;47:771-7. Crossref
19. Taler SJ, Textor SC, Augustine JE. Resistant hypertension:
comparing hemodynamic management to specialist care.
Hypertension 2002;39:982-8. Crossref
20. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC
Guidelines for the management of arterial hypertension:
the Task Force for the management of arterial hypertension
of the European Society of Hypertension (ESH) and of
the European Society of Cardiology (ESC). J Hypertens
2013;31:1281-357. Crossref
21. Dasgupta K, Quinn RR, Zarnke KB, et al. The 2014 Canadian
Hypertension Education Program recommendations for
blood pressure measurement, diagnosis, assessment of
risk, prevention, and treatment of hypertension. Can J
Cardiol 2014;30:485-501. Crossref
22. Nowak RM, Sen A, Garcia AJ, et al. The inability of
emergency physicians to adequately clinically estimate the
underlying hemodynamic profiles of acutely ill patients.
Am J Emerg Med 2012;30:954-60. Crossref
23. Neath SX, Lazio L, Guss DA. Utility of impedance
cardiography to improve physician estimation of
hemodynamic parameters in the emergency department.
Congest Heart Fail 2005;11:17-20. Crossref

