Hong Kong Med J 2016 Apr;22(2):98–105 | Epub 11 Mar 2016
DOI: 10.12809/hkmj154591
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Prevalence of motor problems in children with attention deficit hyperactivity disorder in
Hong Kong
KW Tsui, MB, BS, FHKCPaed1;
Kelly YC Lai, MB, BS, FHKAM (Psychiatry)2;
Marshall MC Lee, FHKCPsy3;
Caroline KS Shea, FHKCPsy3;
Luke CT Tong, FHKCPaed, FHKAM (Paediatrics)1
1 Department of Paediatrics and Adolescent Medicine, Alice Ho Miu Ling
Nethersole Hospital, Tai Po, Hong Kong
2 Department of Psychiatry, The Chinese University of Hong Kong, Shatin,
Hong Kong
3 Department of Psychiatry, Alice Ho Miu Ling Nethersole Hospital, Tai Po,
Hong Kong
Corresponding author: Dr KW Tsui (tsuikw@ha.org.hk)
An earlier version of this paper was presented at the Combined PN and
DBP Joint Scientific Meeting, organised by the Hong Kong Society of Child
Neurology and Developmental Paediatrics held in Hong Kong on 27 March
2014.
Abstract
Introduction: Local data on the occurrence of
motor problems in children with attention deficit
hyperactivity disorder are not available but an
understanding of this important issue may enable
better planning of medical services. We aimed to
determine the prevalence of motor problems in
children with attention deficit hyperactivity disorder
in a local population.
Methods: In this descriptive cross-sectional
study, children aged 6 to 9 years diagnosed with
attention deficit hyperactivity disorder over a
period of 6 months from 1 July to 31 December
2011 were recruited from the Joint Paediatric
and Child Psychiatric ADHD Program in New
Territories East Cluster in Hong Kong. Movement
Assessment Battery for Children and Developmental
Coordination Disorder Questionnaire–Chinese
version were used to determine the presence of
motor problems.
Results: Data from 95 participants were included
in the final analysis. The number of children who
had no, borderline, or definite motor problems was
63, 15, and 17, respectively. It is estimated that up
to one third of local children with attention deficit
hyperactivity disorder might have developmental
coordination disorder.
Conclusions: Motor problems are common in local
children with attention deficit hyperactivity disorder
and figures are comparable with those from other
parts of the world. Despite the various limitations of
this study, the magnitude of the problem should not
be overlooked.
New knowledge added by this study
- This study determined the prevalence of motor problems in local children with attention deficit hyperactivity disorder (ADHD), which was not previously available in Hong Kong.
- It is important to include motor performance as part of the assessment and management of children with ADHD.
Introduction
Attention deficit hyperactivity disorder (ADHD)
is one of the most common neurodevelopmental
problems in children. In Hong Kong, the prevalence
of ADHD among primary one Chinese schoolboys
has been reported to be 8.9%.1 Associated
neurodevelopmental co-morbidities and mental
health problems are frequently found among
individuals with ADHD. The majority (67%)
have at least one co-morbidity and the degree of
functional impairment increases stepwise with the
number of associated co-morbidities that includes
dyslexia, other specific learning disorders, motor
incoordination, anxiety, depression, oppositional
defiance disorder, tics, and Tourette syndrome.2 3 A
diverse group of motor problems has been found to
be co-morbid with ADHD, including an increase in
associated movements.4 Individual subtests of the
Motor Function Neurological Assessment reveal that
80% to 96% of children with ADHD, compared with
0% to 44% of a control group, demonstrate moderate-to-severe problems in motor inhibition and proximal
truncal stabilisation.5 Children with ADHD also
experience greater difficulties in handwriting and
penmanship, which is independent of other motor
problems associated with the disorder.6 7
Developmental coordination disorder (DCD)
is a well-recognised motor disability in an otherwise
healthy individual. The Diagnostic and Statistical
Manual of Mental Disorders, 5th edition (DSM-5)
defines DCD as marked impairment in performance
of motor skills, significantly interfering with daily
activities and/or academic achievements.8 The
degree of coordination deficit is not consistent with
the child’s intellectual ability and is not caused by
pervasive developmental disorder or general medical
condition. The prevalence of DCD in the normal
population varies from 4% to 19%.9 10 11 12 Clinically, DCD
is a heterogeneous condition with coordination
deficits involving gross motor skills, fine motor
skills, or both. Affected children show difficulties and
restricted participation in daily living, eg self-care
activities, academic achievement, leisure, and sports.
Internalising symptoms and motor coordinating
problems frequently co-occur in these children but
their causal relationship is unclear.13 This condition
is believed to be lifelong and the majority of affected
children will not outgrow the problems. They will continue to
experience motor difficulties, poor self-concept, and
various kinds of problems at school.14 Children with
DCD benefit from accommodation in school and
multidisciplinary interventions that focus on task-specific
training activities relevant to daily living and
function.15 16 17
The prevalence of DCD in children with
ADHD has been reported to be as high as 30% to
50%, depending on case definitions.18 19 The presence of ADHD co-morbid with DCD carries the worst
prognosis and predicts poor psychosocial function
in early adulthood.20 Therefore early identification
and intervention in DCD is important in this group
of children who are already adversely affected by
ADHD.
Local data on the occurrence of motor
problems in children with ADHD are not available
but an understanding of this important issue may
enable better planning of medical services. As such,
the aim of this study was to estimate the prevalence
of motor problems in a sample of children with
ADHD at a public hospital in Hong Kong.
Methods
The participants were selected from patients referred
to the Joint Paediatric and Child Psychiatric ADHD
Program, a collaboration of Paediatricians and Child
Psychiatrists of the New Territories East Cluster
(NTEC) of Hong Kong over a period of 6 months
from 1 July to 31 December 2011. The hospitals in
NTEC serve a population of approximately one
million and this ADHD Program is the only public
service provided for children with ADHD within
the cluster. Hospital records of patients aged 6 to
9 years at their first visit were reviewed. Potential
candidates were those with a diagnosis of ADHD
clearly documented in their record and in whom
medication for ADHD was indicated. This study also
included children with confirmed ADHD but whose
parents had declined drug treatment. The diagnosis
of ADHD was based on DSM-IV through clinical
judgement of individual physicians during the clinic
visit. Rating scales, such as Strengths and Weaknesses
of ADHD symptoms and Normal Behavior Scale,
were used in some patients as a reference but the
diagnosis of ADHD remained clinical in our daily
practice. In order to recruit patients with a more
definitive diagnosis of ADHD, only those in whom
drug treatment was indicated were included as
potential candidates. This sample should therefore
represent most children diagnosed with ADHD in a
clinic setting. Patients were excluded when hospital
records documented the presence of intellectual
disability, features of autistic spectrum disorder,
or medical conditions that could affect motor
performance, such as cerebral palsy, hemiplegia, or a
neuromuscular condition. This was consistent with
the exclusion criteria for DCD in DSM-IV.
Movement Assessment Battery for Children
(MABC) is commonly used as a standardised tool
to diagnose DCD in both clinical and research
settings.21 It provides an objective and quantitative
measure of the motor performance of children
between 4 and 12 years of age. There is good
concurrent validity between MABC and Bruininks-Oseretsky test22 and a local study has also shown that this instrument provides satisfactory inter-rater and
test-retest reliability.23 The assessment comprises
eight test items related to three motor domains,
namely manual dexterity, ball skills, and balance
(static and dynamic). The sum of scores from the
eight test items generates a total impairment score
(TIS) and categorises children into one of the three
groups—no, borderline, or definite motor problems.
The Developmental Coordination Disorder
Questionnaire (DCDQ) is a parent-reporting
questionnaire first developed in Canada as a reliable
and valid screening tool for DCD.24 25 It comprises
statements by which parents rate their child’s motor
performance in comparison with other children of
the same age for ball games, balance, and handwriting
skills across home, school, and play environments.
A Chinese version of the DCDQ (DCDQ-C) has
been validated in Taiwan as a screening tool for
DCD in a Chinese-speaking community.26 Parents
responded to each of the 15 questions on a 5-point
Likert scale to generate a total raw score which was
then converted into a probability of having DCD.
A score of >40% chance is suggestive of DCD while
25% to 40% chance indicates a suspected case. In this
study, DSM-IV was used to diagnose DCD and the
questionnaire provided information on one of the
diagnostic criteria about any impairment in daily
functions related to motor performance.
The selected candidates were invited to attend
a one-to-one study session that lasted approximately
30 minutes. The investigator performed MABC
on the children after obtaining consent from the
parents/carers. Baseline information was also
collected and included age, gender, primary school
level, ADHD medication use, drugs taken before
assessment, gestational age, birth weight, and socio-economic
group.
Statistical analysis was performed using the
Statistical Package for the Social Sciences (Windows
version 16.0; SPSS Inc, Chicago [IL], US). The result
of MABC was used as the diagnostic standard for
calculation of DCD prevalence in children with
ADHD. A diagnosis of DCD was made when the
TIS was ≥10, indicating ‘borderline’ (TIS=10 to
13.5) or ‘definite’ (TIS >13.5) motor problems, and
representing the 15th or 5th percentile of TIS in a
general population, respectively. The cut-off at either
the 5th or 15th percentile varied among published
data. As diagnosis of DCD requires fulfilling other
criteria, such as impairment of daily activities, raising
the cut-off to the 15th percentile in MABC could
improve the sensitivity of the test. Nonetheless, use
of the DCDQ-C avoided the risk of overdiagnosis.
Prevalence was expressed as the percentage of DCD
cases in participants with ADHD who underwent
MABC assessment. The Chi squared test was
applied to detect any difference in characteristics
of participants with and without DCD. Analysis of
variance was used to detect any significant difference
in TIS of the MABC between DCDQ-C–defined
motor performance groups. The concurrent validity
was investigated by testing the probability score
of DCDQ-C against TIS of MABC with Pearson’s
correlation coefficient. Sensitivity, specificity, and
positive and negative predictive values of DCDQ-C
were calculated.
Ethical approval was obtained from the
Joint Chinese University of Hong Kong and NTEC Clinical Research Ethics
Committee.
Results
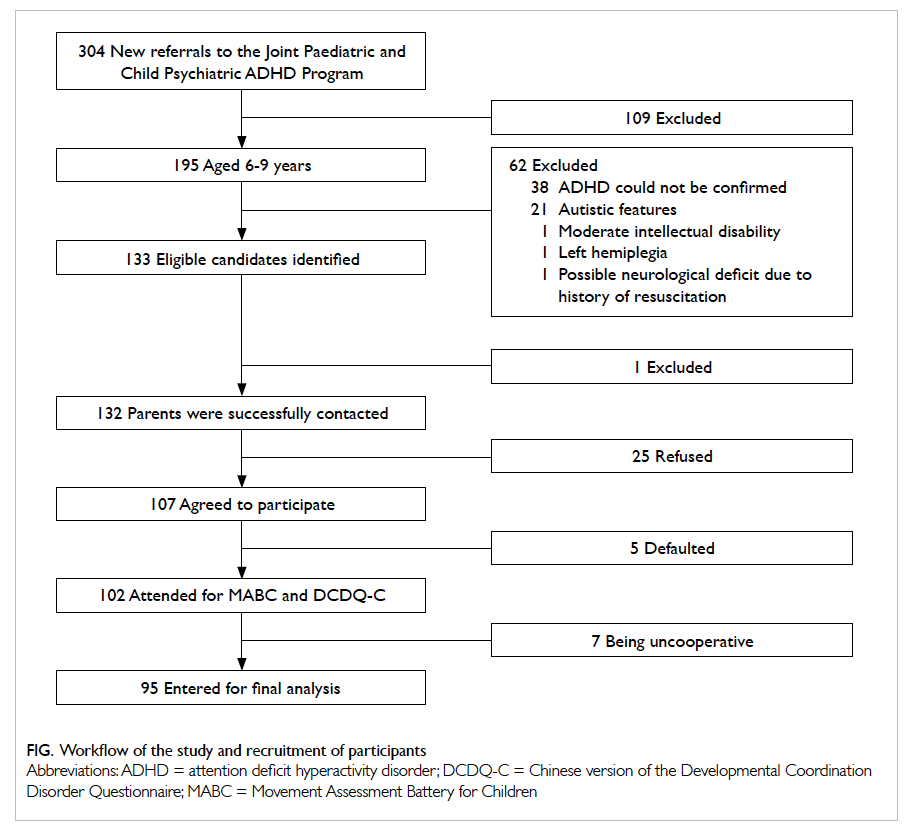
From 1 July to 31 December 2011, 304 new cases
were referred to the Joint Paediatric and Child
Psychiatric ADHD Program of NTEC. Of the 195
potential candidates aged 6 to 9 years, diagnosis
of ADHD was unconfirmed in 38. After exclusion
of 21 patients with autistic features, one patient
with moderate intellectual disability, one patient
with left hemiplegia, and one patient with possible
neurological deficit following cardiopulmonary
resuscitation, 133 children were eligible for this
study. Of the 132 parents who were successfully
contacted, 107 agreed to participate. The MABC
was tested on 102 candidates and five defaulted.
The results of seven participants were rejected as
they were uncooperative, making MABC scoring
unreliable. Of the 133 eligible candidates, statistical
analysis was performed on results from 95 (71.4%),
with 63 males and 32 females and a mean age of 7.8
years. The Figure summarises the workflow of this study and the candidate recruitment process.
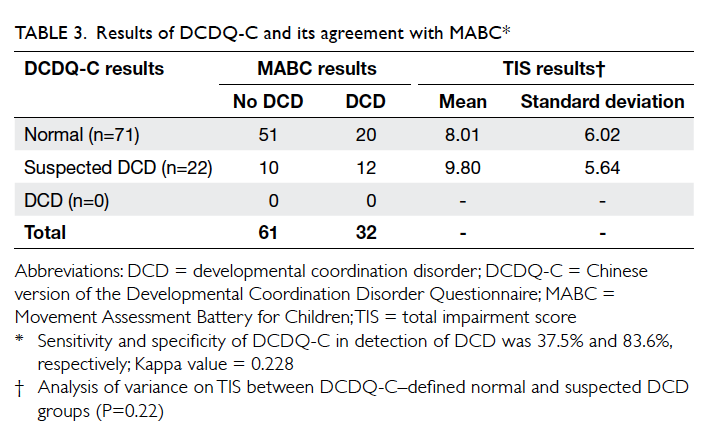
Table 1 shows the results of MABC performed
on the 95 participants. Based on the TIS, three
motor performance groups were identified: no
motor problem (n=63; mean TIS=4.75 with 95%
confidence interval [CI] of 4.1-5.4), borderline
motor problem (n=15; mean TIS=11.53 with 95%
CI of 11.0-12.1), and definite motor problem (n=17;
mean TIS=18.53 with 95% CI of 16.6-20.5). Using
the 15th percentile of motor performance in MABC
as a cut-off, the prevalence of motor problems in this
group of children with ADHD was 33.7% (95% CI,
24.2%-43.2%).
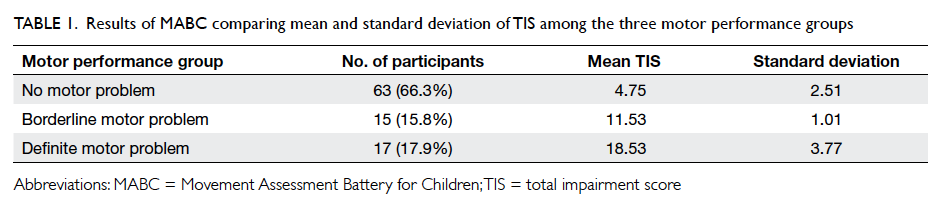
Table 1. Results of MABC comparing mean and standard deviation of TIS among the three motor performance groups
Table 2 shows the baseline information about
the two groups with motor problems (borderline
and definite) and the group with no motor problems
and includes sex, perinatal history, socio-economic
background, drug treatment, and previous motor
training. There was no statistical difference between
these two groups, except for a history of receiving
motor training at a younger age (P=0.002).
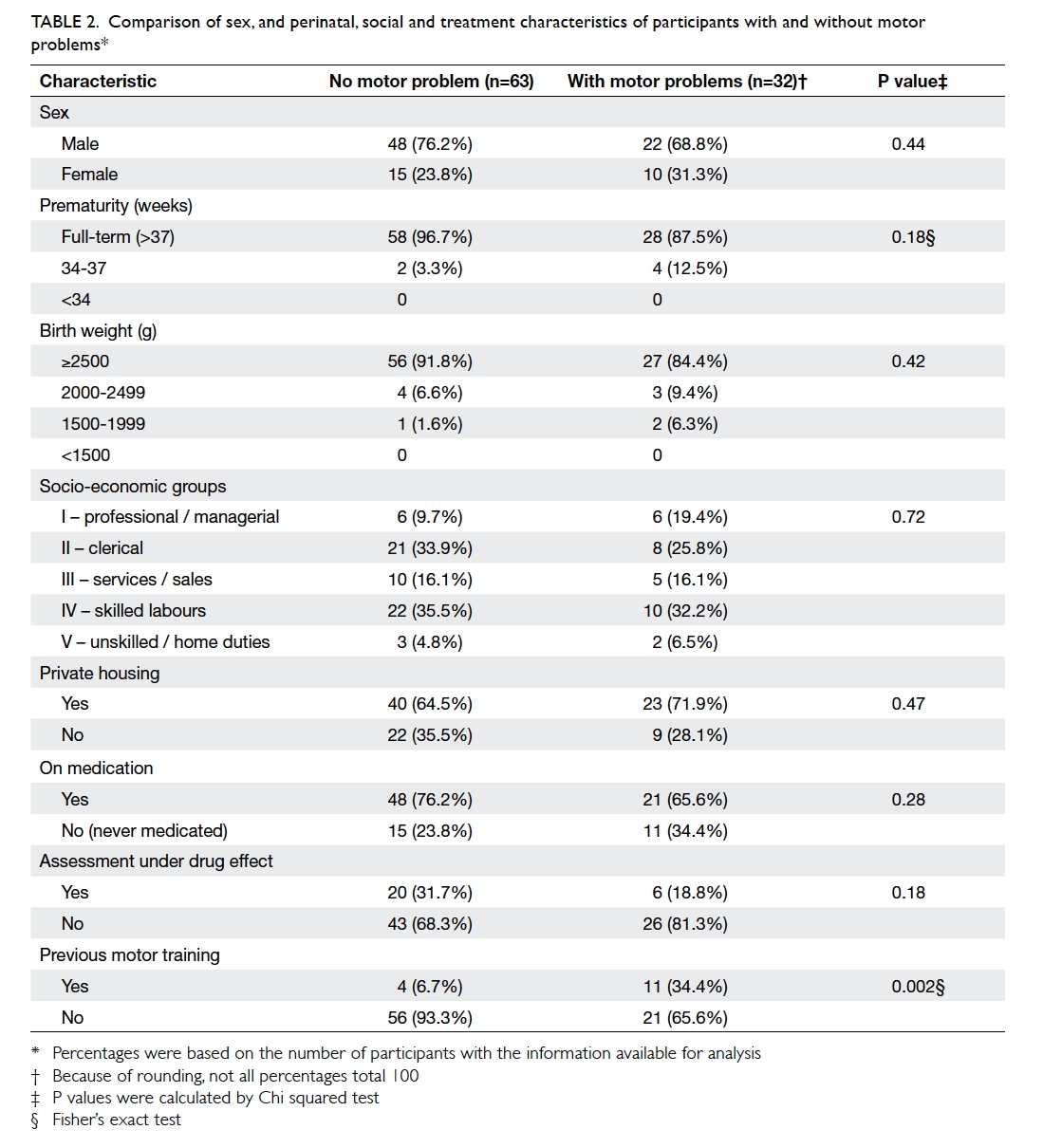
Table 2. Comparison of sex, and perinatal, social and treatment characteristics of participants with and without motor problems
Two carers who accompanied a child to the
study session could not read Chinese, therefore
93 completed DCDQ-C were analysed. The
questionnaire identified 71 and 22 participants with
no motor problems and suspected motor problems,
respectively, but none was found to have definite
DCD (>40% chance) [Table 3]. For correlation between MABC and DCDQ-C, the Kappa value was
0.228 indicating a low agreement between the two
instruments (P=0.023). Using MABC as a standard
measure for motor performance, sensitivity and
specificity of DCDQ-C on identification of DCD
was 37.5% and 83.6%, respectively. The positive
predictive value of DCDQ-C was 54.5% and the
negative predictive value was 71.8%. Thus DCDQ-C
could quite reliably exclude DCD but was rather
insensitive when identifying motor problems in
children with ADHD in Hong Kong.
Discussion
In this clinic sample of children with ADHD, the
results of MABC revealed that 15.8% had borderline
and 17.9% had definite motor problems. Overseas
studies have often used the 15th percentile of TIS in
MABC as the cut-off for identification of DCD.17 19 25
By using the same standard here, participants who
belonged to the borderline and definite motor
problem groups could be potentially diagnosed as
having DCD. A diagnosis of DCD, however, requires
confirmation of motor problems and impaired
daily functions. Initially, DCDQ-C was intended to
provide the impairment criteria for a DCD diagnosis
but it could not be reliably applied here due to the
significant lack of agreement with MABC in this
study sample. We therefore estimated that DCD may
occur in up to one third of patients with ADHD, a
figure that is comparable with the literature.
In our clinical experience, motor difficulties
are usually not a common presenting symptom
during a medical consultation for ADHD. There are
a few possible reasons why motor performance may
be overlooked. First, the parents of these children
are often overwhelmed by the symptoms of ADHD
and attribute all difficulties to a single diagnosis.
In addition, it may be difficult for parents to
differentiate symptoms related to motor impairment
from those related to ADHD, for examples, bumping
into objects, poor postural stability, and illegible
handwriting. Second, cultural influences may play
a part. Hong Kong children adopt a very sedentary
lifestyle and are probably the most physically
inactive students in the world.27 Sports skills are not
essential for most local children in the school and
social environment. Third, there was less diversity
for participation in leisure activities among ADHD
children compared with their normal peers.28
Children with ADHD were encouraged to participate
in tutorial lessons to support academic achievement,
rather than other non–academic-related activities.
They spent many hours after school every day for
completion of homework and revision, leaving little
time for sports or other leisure activities. Limited
participation in physical activities masks underlying
motor problems and conversely means any motor
talent goes unrecognised. Therefore, clinicians who
manage children with ADHD should be aware of
these issues and need to consider motor problems (or
DCD) as a factor that causes persistent impairment,
especially when the symptoms of ADHD improve.
The prevalence of DCD in children born
extremely premature (<29 weeks) or with extremely
low birth weight (<1000 g) has been reported to be
high, which was around 42% in one study.29 A recent
meta-analysis of studies in school-aged children
with very low birth weight (VLBW)/very preterm
reported an odds ratio (OR) of up to 8.66.30 In our
study, 6.5% and 10.8% of children had a history of
prematurity or low birth weight, respectively, but
none was born very preterm or with VLBW. It
was therefore not surprising to see no significant
difference between the groups with and without
motor problems in terms of maturity and birth
weight. Local figures published in 1998 show that
the incidence of very preterm delivery (<34 weeks)
and very/extremely low birth weight (<1500 g) was
2.22% and 1.25%, respectively.31 The sample size of
the current study was simply not large enough to
include these children.
There are studies that show improved motor
performance and quality of life in children with co-morbid
ADHD and DCD following treatment with
methylphenidate.32 33 34 As shown in Table 2, a lower prevalence of motor problems was found in children
who were prescribed regular medication or who had
taken medication prior to the assessment (OR=0.6
and 0.5, respectively) but this was not statistically
significant (P=0.28 and 0.18, respectively). This may
be because we recruited some children who had been
recently diagnosed with ADHD and medication was
not yet optimised at the time of MABC testing, or
simply because of a lack of statistical power due to
the small number of subjects. To better understand
this issue, further studies should be carried out to
specifically examine the effect of ADHD medication
on motor performance.
Of the 15 participants who had received
previous motor training, 11 had motor problems. This
group was quite heterogeneous and, interestingly,
many parents could not recall the exact reason for
the motor training. As mentioned before, DCD is a
relatively stable condition and intervention should
focus on specific motor skills. Previous training
does not preclude children from having future
motor problems as demand for activities, such as
handwriting and participation in sports, increases
when children progress from preschool to primary
school. It is therefore vital to determine whether
motor skills are at an age-appropriate level for both
academic and extracurricular activities and provide
task-specific training whenever indicated.
Although the DCDQ-C has been validated for
use in Taiwan, which is a Chinese community similar
to Hong Kong, the questionnaire was not appropriate
for local Hong Kong children. This demonstrates the
need to be cautious when adopting an assessment tool
from overseas without local validation, even from an
area with comparable cultural and socio-economic
background. Furthermore, a questionnaire cannot
replace detailed history taking in clinical practice
that is indispensable when making a diagnosis of
neurodevelopmental disorders, such as ADHD and
DCD.
Since DCDQ-C could not reliably reflect
motor performance in this group of children, the
degree of impairment in daily activities was not
adequately assessed to make a definite diagnosis of
DCD. A local study of the prevalence of DSM-IV
disorders in Chinese adolescents pointed out that
figures would be overestimated if the impairment
criteria were not taken into account.35 Although
MABC used alone would probably overdiagnose
DCD by not considering the impairment factors, it
is worth noting that 17.9% of our study candidates
had definite motor problems. This is actually below
the 5th percentile of the general population. Thus
the magnitude of motor difficulties is substantial
and motor problems (with or without a diagnosis
of DCD) should not be overlooked in children with
ADHD.
Limitations of this study
There are some limitations to this study. Parents
who perceived their children to have motor problems
were more keen to participate, leading to a selection
bias in the recruitment of children. Although all
children were diagnosed with ADHD, they were
not a homogeneous group. They were diagnosed by
different physicians and were not at a uniform stage
of drug treatment. Even though MABC is a widely
used tool in Hong Kong, the lack of a local norm
might still affect the validity of this study.
Conclusions
Motor problems in children with ADHD are as
common in Hong Kong as in other countries and
DCD may have been present in up to 33.7% of
this clinic sample. Acknowledgement of their own
strength and weakness will enable patients to better
plan future goals. Provision for assessment and
management of DCD and other motor problems
should be a fundamental part of a comprehensive
programme to manage ADHD.
References
1. Leung PW, Luk SL, Ho TP, Taylor E, Mak FL, Bacon-Shone
J. The diagnosis and prevalence of hyperactivity in Chinese
schoolboys. Br J Psychiatry 1996;168:486-96. Crossref
2. Larson K, Russ SA, Kahn RS, Halfon N. Patterns of
comorbidity, functioning, and service use for US children
with ADHD, 2007. Pediatrics 2011;127:462-70. Crossref
3. Gillberg C, Gillberg IC, Rasmussen P, et al. Co-existing
disorders in ADHD—implications for diagnosis and
intervention. Eur Child Adolesc Psychiatry 2004;13 Suppl
1:I80-92. Crossref
4. Licari M, Larkin D. Increased associated movements:
Influence of attention deficits and movement difficulties.
Hum Mov Sci 2008;27:310-24. Crossref
5. Stray LL, Stray T, Iversen S, Ruud A, Ellertsen B, Tønnessen
FE. The Motor Function Neurological Assessment (MFNU)
as an indicator of motor function problems in boys with
ADHD. Behav Brain Funct 2009;5:22. Crossref
6. Brossard-Racine M, Majnemer A, Shevell M, Snider L,
Bélanger SA. Handwriting capacity in children newly
diagnosed with attention deficit hyperactivity disorder.
Res Dev Disabil 2011;23:2927-34. Crossref
7. Shen IH, Lee TY, Chen CL. Handwriting performance
and underlying factors in children with attention deficit
hyperactivity disorder. Res Dev Disabil 2012;33:1301-9. Crossref
8. Diagnostic and Statistical Manual of Mental Disorders
(DSM-5). 5th ed. Washington DC: American Psychiatric
Association; 2013.
9. Missiuna C, Cairney J, Pollock N, et al. A staged approach
for identifying children with developmental coordination
disorder from the population. Res Dev Disabil 2011;32:549-59. Crossref
10. Tsiotra GD, Flouris AD, Koutedakis Y, et al. A comparison
of developmental coordination disorder prevalence
rates in Canadian and Greek children. J Adolesc Health
2006;39:125-7. Crossref
11. Kadesjö B, Gillberg C. Developmental coordination
disorder in Swedish 7-year-old children. J Am Acad Child
Adolesc Psychiatry 1999;38:820-8. Crossref
12. Wright HC, Sugden DA. A two-step procedure for
the identification for children with developmental
coordination disorder in Singapore. Dev Med Child
Neurol 1996;38:1099-105. Crossref
13. Cairney J, Veldhuizen S, Szatmari P. Motor coordination
and emotional-behavioral problems in children. Curr Opin
Psychiatry 2010;23:324-9. Crossref
14. Losse A, Henderson SE, Elliman D, Hall D, Knight E,
Jongmans M. Clumsiness in children—do they grow out
of it? A 10-year follow-up study. Dev Med Child Neurol
1991;33:55-68. Crossref
15. Sugden DA, editor. Leeds consensus statement:
developmental coordination disorder as a specific learning
difficulty. In: ESRC Research Seminar Series 2004-2005.
Leeds (UK): Economic & Social Research Council; 2006.
16. Polatajko HJ, Cantin, N. Developmental coordination
disorder (dyspraxia): an overview of the state of the art.
Semin Pediatr Neurol 2005;12:250-8. Crossref
17. Watemberg N, Waiserberg N, Zuk L, Lerman-Sagie T.
Developmental coordination disorder in children with
attention-deficit-hyperactivity disorder and physical
therapy intervention. Dev Med Child Neurol 2007;49:920-5. Crossref
18. Pitcher TM, Piek JP, Hay DA. Fine and gross motor ability
in males with ADHD. Dev Med Child Neurol 2003;45:525-35. Crossref
19. Tseng MH, Howe TH, Chuang IC, Hsieh CL. Cooccurrence
of problems in activity level, attention, psychosocial
adjustment, reading and writing in children with
developmental coordination disorder. Int J Rehabil Res
2007;30:327-32. Crossref
20. Rasmussen P, Gillberg C. Natural outcome of ADHD with
developmental coordination disorder at age 22 years: a
controlled, longitudinal, community-based study. J Am
Acad Child Adolesc Psychiatry 2000;39:1424-31. Crossref
21. Henderson SE, Sugden DA. Movement assessment battery
for children. London: Psychological Corporation; 1992.
22. Croce RV, Horvat M, MaCarthy E. Reliability and
concurrent validity of the movement assessment battery
for children. Percept Mot Skills 2001;93:275-80. Crossref
23. Chow SM, Henderson SE. Interrater and test-retest
reliability of the Movement Assessment Battery for Chinese
preschool children. Am J Occup Ther 2003;57:574-7. Crossref
24. Wilson BN, Kaplan BJ, Crawford SG, Campbell A, Deway
D. Reliability and validity of a parent questionnaire on
childhood motor skills. Am J Occup Ther 2000;54:484-93. Crossref
25. Schoemaker MM, Flapper B, Verheij NP, Wilson BN,
Reinders-Messelink HA, de Kloet A. Evaluation of the
Developmental Coordination Disorder Questionnaire as a
screening instrument. Dev Med Child Neurol 2006;48:668-73. Crossref
26. Tseng MH, Fu CP, Wilson BN, Hu FC. Psychometric
properties of a Chinese version of the Developmental
Coordination Disorder Questionnaire in community-based
children. Res Dev Disabil 2010;31:33-45. Crossref
27. Macfarlane D. Children’s physical activity patterns and the
implications for health. In: Johns DP, Lindner KJ, editors.
Physical activity and health of Hong Kong youth. Hong
Kong: The Chinese University Press; 2006: 67-87.
28. Shimoni M, Engel-Yeger B, Tirosh E. Participation in leisure
activities among boys with attention deficit hyperactivity
disorder. Res Dev Disabil 2010;31:1234-9. Crossref
29. Goyen TA, Lui K. Developmental coordination disorder
in “apparently normal” schoolchildren born extremely
preterm. Arch Dis Child 2009;94:298-302. Crossref
30. Edwards J, Berube M, Erlandson K, et al. Developmental
coordination disorder in school-aged children born very
preterm and/or at very low birth weight: a systematic
review. J Dev Behav Pediatr 2011;32:678-87. Crossref
31. Leung TN, Roach VJ, Lau TK. Incidence of preterm
delivery in Hong Kong Chinese. Aust NZ J Obstet Gynaecol
1998;38:138-41. Crossref
32. Bart O, Podoly T, Bar-Haim Y. A preliminary study on
the effect of methylphenidate on motor performance in
children with comorbid DCD and ADHD. Res Dev Disabil
2010;31:1443-7. Crossref
33. Flapper BC, Schoemaker MM. Effects of methylphenidate
on quality of life in children with both developmental
coordination disorder and ADHD. Dev Med Child Neurol
2008;50:294-9. Crossref
34. Stray LL, Stray T, Iversen S, Ruud A, Ellertsen B.
Methylphenidate improves motor functions in children
diagnosed with hyperkinetic disorder. Behav Brain Funct
2009;5:21. Crossref
35. Leung PW, Hung SF, Ho TP, et al. Prevalence of DSM-IV
disorders in Chinese adolescents and the effects of an
impairment criterion: a pilot community study in Hong
Kong. Eur Child Adoles Psychiatry 2008;17:452-61. Crossref