Hong Kong Med J 2015 Dec;21(6):524–7 | Epub 14 Aug 2015
DOI: 10.12809/hkmj144437
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
The safety and tolerability of adenosine as a pharmacological stressor in stress perfusion cardiac magnetic resonance imaging in the Chinese population
KH Tsang, MB, BS, FRCR;
Winnie SW Chan, MB, ChB, FHKAM (Radiology);
CK Shiu, MB, BS, FRCR;
MK Chan, MB, BS, FHKAM (Radiology)
Department of Radiology and Imaging, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr KH Tsang (tsang_kh@yahoo.com.hk)
Abstract
Objective: To investigate the safety profile and
effectiveness of adenosine as a pharmacological
stressor in patients with known or suspected
coronary artery disease who underwent cardiac
magnetic resonance imaging perfusion study.
Design: Case series.
Setting: Regional hospital, Hong Kong.
Patients: All patients who underwent adenosine stress cardiac
magnetic resonance imaging from May 2013 to
August 2013 were prospectively interviewed during
the scan.
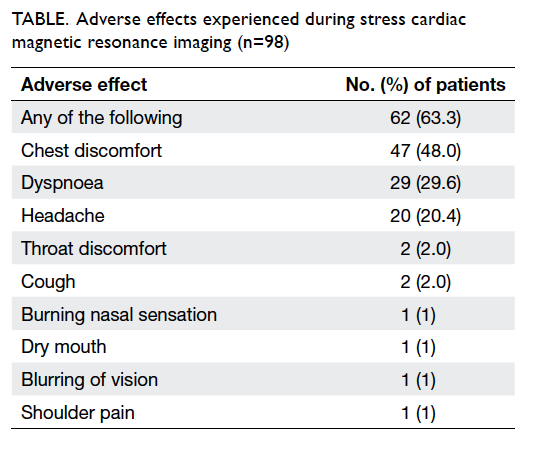
Main outcome measures: Common side-effects
of adenosine as well as any other discomfort
experienced during the scan were recorded.
Haemodynamic changes including systolic and
diastolic blood pressure and pulse rate before and
during adenosine administration were also recorded.
Results: There were 98 consecutive patients with a
mean (± standard deviation) age of 64.0 ± 11.4 years
(range, 10-83 years) and mean body weight of 67.5
± 12.0 kg. Male-to-female ratio was 2.5:1. Of the
98 patients interviewed, 62 (63.3%) experienced
one or more adenosine-associated adverse effects.
Chest discomfort was most frequently experienced
(48.0%), followed by dyspnoea (29.6%) and headache
(20.4%). No life-threatening event occurred.
Following adenosine administration, a significant
rise in pulse rate (75.1 ± 14.3 vs 93.2 ± 14.7 beats/min; P<0.01) and a significant drop in diastolic blood
pressure (75.1 ± 13.3 vs 68.0 ± 13.9 mm Hg; P<0.01)
were noted. There was a general decrease in systolic
blood pressure, although no statistically significant
difference was observed (144.9 ± 17.6 vs 143.1 ± 21.4
mm Hg; P=0.18).
Conclusion: Adenosine stress cardiac magnetic
resonance perfusion study is safe and well tolerated
in clinical practice.
New knowledge added by this
study
- This is the first study of the safety and tolerability of adenosine in our locality. It showed that adenosine is an effective stressor for use in stress cardiovascular magnetic resonance imaging.
- To familiarise clinicians with the workflow of adenosine stress cardiovascular magnetic resonance imaging and its contra-indications in order to facilitate its clinical use.
- Adenosine stress cardiovascular magnetic resonance imaging is a safe and effective method to investigate ischaemic heart disease and should be more widely adopted in local clinical practice.
Introduction
The use of stress perfusion study in cardiac magnetic
resonance imaging (CMR) for the evaluation of
myocardial ischaemia or infarction has increased
significantly over recent years.1 It is increasingly used
in patients with known or suspected coronary artery
disease. The major advantage of CMR is that it does
not involve ionising radiation and allows simultaneous
assessment of myocardial perfusion, function, and
visualisation of myocardial scar with high spatial and
temporal resolution. Global and regional wall motion
abnormalities can also be assessed.
Perfusion imaging allows detection of
myocardial ischaemia (Fig) whereas late gadolinium
enhancement scan allows detection of myocardial
scar and infarction. Recent studies also show that
adenosine stress perfusion CMR provides excellent risk
stratification and intermediate-term prognostic
value in patients with stable coronary artery disease.2
The presence of a myocardial perfusion deficit is an
incremental prognostic risk factor over other risk
factors.2
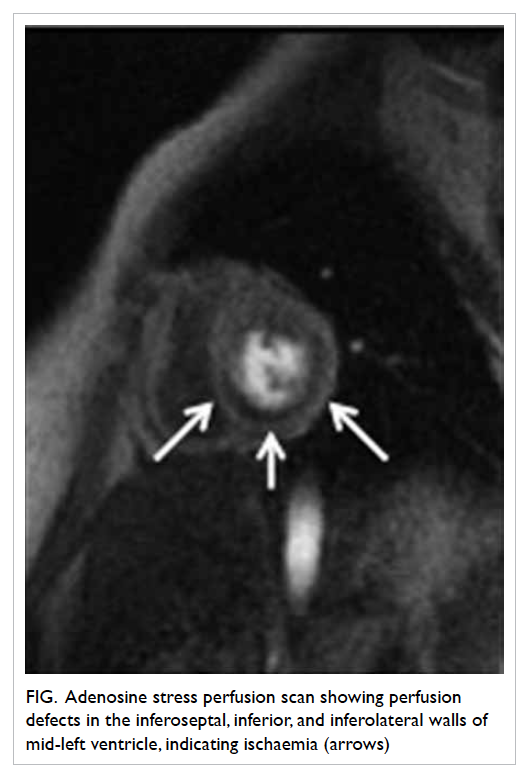
Figure. Adenosine stress perfusion scan showing perfusion defects in the inferoseptal, inferior, and inferolateral walls of mid-left ventricle, indicating ischaemia (arrows)
Studies involving CMR are usually performed
with first-pass perfusion imaging using a vasodilatory
pharmacological stressor. Adenosine is the most
commonly used agent and has been found to be safe
and effective in many studies.3 4 5 6 Its safety profile
in the Chinese population, however, is generally
unknown.
There are three adenosine receptor subtypes,
A1, A2, and A3; A2 can be further subdivided into A2a
and A2b. Stimulation of the A2a receptors on arterial
vascular smooth muscle causes vasodilatation.
Stimulation of A1, A2b, and A3 receptors may result
in dyspnoea, chest pain, atrioventricular block or
bronchospasm, accounting for its adverse side-effects.
4 5 6 7
Adenosine can produce near-maximal
vasodilatation in the normal coronary artery,
resulting in a 4- to 5-times increase in blood flow.
Nonetheless, in myocardial segments supplied
by a stenotic vessel, the arteriolar resistance has
already been reduced at the resting state to maintain
adequate regional blood flow. This means that no
further or only minor reductions can take place.5
Thus, flow heterogeneity occurs during vasodilator
stress and can be readily detected by magnetic
resonance perfusion imaging.
The aim of this study was to investigate the
safety profile and effectiveness of adenosine as a
pharmacological stressor in patients with known or
suspected coronary artery disease who undergo
CMR.
Methods
We prospectively interviewed all patients during
stress CMR from May 2013 to August 2013. Patients
were questioned specifically about common side-effects
of adenosine during stress CMR examination,
as well as any other discomfort experienced during
the scan. Their haemodynamic changes including
systolic and diastolic blood pressure and pulse
rate before and during adenosine administration
were recorded and were monitored continually
throughout the scan. Real-time electrocardiographic
monitoring was performed to identify any heart
block or arrhythmia.
The exclusion criteria included contra-indications
to contrast magnetic resonance imaging
(MRI; non-MRI–compatible metallic objects,
pacemaker, claustrophobia, pregnancy, allergy
to gadolinium contrast) or contra-indications to
adenosine (history of asthma, second- or third-degree
heart block, and severe aortic stenosis). Stress
CMR was not performed in patients with caffeine
intake 24 hours prior to the study.
Paired stress and rest perfusion studies
were performed. In stress perfusion, adenosine
(Adenoscan; Sanofi-Synthelabo, Guildford, UK) was
infused at 140 µg/kg/min through a 20-G antecubital
venous catheter with a total duration of approximately
3 to 7 minutes. Dynamic scanning was performed
by injecting gadolinium-based contrast. Gadoterate
meglumine (Dotarem; Guerbet, Roissy CdG Cedex,
France) as contrast agent was injected via a power injector at
4 mL/s through a 18-G antecubital venous catheter
with a dosage of around 0.1 mmol/kg, followed by a
15-mL saline flush. Adenosine infusion was stopped
immediately after completion of the stress perfusion
scanning sequence.
The patient was allowed to rest. Rest perfusion
study was performed at least 15 minutes after the
stress perfusion study. All stress CMR studies at
our centre were carried out during office hours.
The examination was monitored by the on-duty
radiologist who was present on site. No cardiologist
was on standby or on call in the MRI scanning suite
but was readily reachable during office hours within
the hospital.
Cardiovascular magnetic resonance protocol
Patients were scanned using a 1.5-Tesla MRI
machine (MAGNETOM Sonata; Siemens, Erlangen,
Germany). Myocardial perfusion studies were
performed after the scout imaging and standardised
cine sequences for cardiac axis determination.
First-pass contrast-enhanced magnetic
resonance images were obtained with a saturation-recovery
turbo FLASH sequence (repetition time
195 ms, echo time 1.1 ms, inversion time 110 ms, flip
angle 12 degrees, 28 x 28 cm field of view, 10-mm
section thickness). Acquisition of three short-axis
images of the left ventricle targeting at the base,
mid-ventricle, and apex was continuously repeated
every, or every other, heartbeat depending on heart
rate. A total of 70 images were acquired at each slice
location for perfusion study. Images were acquired
at rest and stress.
Scanning for stress perfusion study was
commenced when target heart rate was achieved or
when the patient had symptoms of chest discomfort.
The target heart rate was an increase in resting heart
rate. Patients were instructed to begin holding their
breath at the start of the image acquisition and to
maintain the breath-hold for as long as possible and
to breathe slowly if breath could no longer be held.
Statistical analysis
Systolic and diastolic blood pressure and heart rate
were recorded at rest before the adenosine infusion
and immediately after adenosine infusion. Data were
presented as mean and standard deviations. Student’s
paired t test was used to compare intrapersonal
difference in blood pressure and pulse pre- and post-drug
administration. Statistical significance was
taken at a P value of <0.05. Analysis was performed
using the Statistical Package for the Social Sciences
(Windows version 22.0; SPSS Inc, Chicago [IL], US).
Results
A total of 98 consecutive patients were included
from May 2013 to August 2013. Four patients were
excluded: three had a history of asthma and one
had known second-degree heart block. The mean
(± standard deviation) age was 64.0 ± 11.4 years
(range, 10-83 years). The mean body weight was 67.5
± 12.0 kg and the male-to-female ratio was 2.5:1.
The clinical indications for adenosine stress CMR
were mainly to investigate myocardial ischaemia
in patients with suspected coronary disease or to
look for disease progress in patients with known
ischaemic heart disease with stenting or previous
coronary artery bypass.
In our study group, 51 (52.0%) patients were
investigated with suspected coronary artery disease,
41 (41.8%) were investigated prior to stenting
or bypass, five (5.1%) were for investigation of
cardiomyopathy, and one (1%) was scanned for
known coronary artery fistula. The mean duration
of adenosine administration was 3.2 ± 0.9 minutes
before the start of scanning of perfusion study.
Of the 98 patients, 62 (63.3%) experienced
one or more adenosine-associated adverse effects.
The remaining patients (36.7%) experienced no
discomfort. Chest discomfort was the most frequent
adverse effect experienced by 47 (48.0%) patients,
followed by dyspnoea (29.6%) and headache (20.4%).
Eight (8.2%) patients also experienced other adverse
effects (Table).
In our cohort of patients, 51 (52.0%) had
a history of significant coronary stenosis. Stenting
had been performed previously in 40 (40.8%), of
whom two also had previous coronary bypass.
Previous coronary bypass without stenting had been
performed in one patient and the remainder had no
stent or bypass.
Chi squared test and Fisher’s exact test were
used to compare overall side-effect and individual
side-effect occurrence in patients with significant
coronary stenosis with those having no known
significant stenosis. All P values were >0.05 revealing
no significant difference between the two groups of
patients regarding occurrence of adverse effects.
Regarding the haemodynamic effects, a
significant drop in diastolic blood pressure was
observed following adenosine administration (75.1 ±
13.3 vs 68.0 ± 13.9 mm Hg; P<0.01). A significant rise
in pulse rate was also noted (75.1 ± 14.3 vs 93.2 ± 14.7
beats/min; P<0.01). There was a general decrease
in systolic blood pressure although no statistically
significant difference was observed (144.9 ± 17.6 vs
143.1 ± 21.4 mm Hg; P=0.18). There was no premature
termination of the examination. No arrhythmia was
recorded and no prescription of aminophylline as an
antidote to adenosine was required.
Discussion
This study shows that adenosine is a safe
pharmacological stressor for stress perfusion study
in CMR. Adverse effects were experienced by the
majority of patients (63.3%) but none required
treatment and there were no life-threatening
events. Patient discomfort subsided quickly after
stress perfusion study when adenosine infusion was
stopped due to the short half-life of the agent.
No death, myocardial infarction, heart block,
arrhythmia, or bronchospasm was recorded. These
complications have been reported in the literature,
albeit rarely. Their complete absence in our study
may have been due to the relatively small sample size
or patient selection factors. Nonetheless, relevant
drugs, aminophylline, atropine, and adrenaline
should be available in case of emergency.
Chest pain was the most frequent complaint, in
agreement with other studies that report a frequency
of 10% to 57%.3 4 5 6 In our study, all patients experienced
mild chest pain but without the need to abandon the
examination. The mechanism of adenosine-induced
chest pain is unclear. Direct activation of myocardial
nociceptors is one possible explanation.8
Dyspnoea was another common complaint in
our study, reported by 12% to 45% of patients in other
studies.3 4 5 6 This may be due to stimulation of carotid
chemoreceptors leading to an increase in respiratory
rate and depth. Transient heart block was not seen in
our patients but has been reported in 0.8% to 10% of
patients in other series.3 4 5 6
Some of the reported side-effects in our
patients were not the usual recognised side-effects
of adenosine and their occurrence may be incidental.
Patients were briefed about the common side-effects
especially chest discomfort before the CMR
examination. This is standard practice of many CMR
centres. This may potentially affect the incidence of
some of the reported side-effects.
There was an insignificant drop in systolic
blood pressure despite the vasodilatory effect of the
drug due to the compensatory effect of the increased
heart rate.
The excellent safety profile of adenosine
can be attributed to its short half-life (6-10 s) that
makes its effects quickly reversible after the drug is
discontinued.9 10 Careful screening and exclusion of
patients with contra-indications to adenosine will
also help to minimise significant adverse effects.
Drug safety can be further enhanced as the effects of
adenosine can be quickly halted by aminophylline,
although the antidote is rarely needed. In our study,
adenosine was well tolerated and there was no need
to terminate scanning due to drug intolerance.
Conclusion
With the increasing clinical use of adenosine
stress CMR, the safety of the drug in the magnetic
resonance environment needs to be established.
We showed that adenosine is a safe and effective
pharmacological stressor to be used in stress CMR
for the assessment of myocardial ischaemia. The
majority of patients experienced adverse effects that
were transient and self-limiting. No life-threatening
events were reported.
References
1. Gerber BL, Raman SV, Nayak K, et al. Myocardial first-pass
perfusion cardiovascular magnetic resonance: history,
theory, and current state of the art. J Cardiovas Magn
Reson 2008;10:18. Crossref
2. Buckert D, Dewes P, Walcher T, Rottbauer W, Bernhardt P.
Intermediate-term prognostic value of reversible perfusion
deficit diagnosed by adenosine CMR: a prospective follow-up
study in a consecutive patient population. JACC
Cardiovasc Imaging 2103;6:56-63. Crossref
3. Luu JM, Filipchuk NG, Friedrich MG. Indications, safety
and image quality of cardiovascular magnetic resonance:
experience in >5000 North American patients. Int J Cardiol
2013;168:3807-11. Crossref
4. Voigtländer T, Schmermund A, Bramlage P, et al. The
adverse events and hemodynamic effects of adenosine-based
cardiac MRI. Korean J Radiol 2011;12:424-30. Crossref
5. Karamitsos TD, Arnold JR, Pegg TJ, et al. Tolerance and
safety of adenosine stress perfusion cardiovascular magnetic
resonance imaging in patients with severe coronary artery
disease. Int J Cardiovasc Imaging 2009;25:277-83. Crossref
6. Khoo JP, Grundy BJ, Steadman CD, Sonnex EP, Coulden
RA, McCann GP. Stress cardiovascular MR in routine clinical practice: referral patterns,
accuracy, tolerance, safety and incidental findings. Br J
Radiol 2012;85:e851-7. Crossref
7. Hori M, Kitakaze M. Adenosine, the heart, and coronary
circulation. Hypertension 1991;18:565-74. Crossref
8. Sylvén C, Beermann B, Jonzon B, Brandt R. Angina
pectoris-like pain provoked by intravenous adenosine in
healthy volunteers. Br Med J (Clin Res Ed) 1986;293:227-30. Crossref
9. Wilson RF, Wyche K, Christensen BV, Zimmer S, Laxson
DD. Effects of adenosine on human coronary arterial
circulation. Circulation 1990;82:1595-606. Crossref
10. Belardinelli L, Linden J, Berne RM. The cardiac effects of
adenosine. Prog Cardiovasc Dis 1989;32:73-97. Crossref