Hong Kong Med J 2015 Dec;21(6):511–7 | Epub 6 Nov 2015
DOI: 10.12809/hkmj154599
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Rising incidence of morbidly adherent placenta
and its association with previous caesarean
section: a 15-year analysis in a tertiary hospital in
Hong Kong
Katherine KN Cheng, MB, ChB;
Menelik MH Lee, FHKCOG, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr Katherine KN Cheng (chengkaning@gmail.com)
Abstract
Objectives: To identify the incidence of morbidly
adherent placenta in the context of a rising caesarean
delivery rate within a single institution in the past 15
years, and to determine the contribution of morbidly
adherent placenta to the incidence of massive postpartum
haemorrhage requiring hysterectomy.
Design: Case series.
Setting: A regional obstetric unit in Hong Kong.
Patients: Patients with a morbidly adherent placenta
with or without previous caesarean section scar
from 1999 to 2013.
Results: A total of 39 patients with morbidly adherent
placenta were identified during 1999 to 2013. The
overall rate of morbidly adherent placenta was
0.48/1000 births, which increased from 0.17/1000
births in 1999-2003 to 0.79/1000 births in 2009-2013.
The rate of morbidly adherent placenta with previous
caesarean section scar and unscarred uterus also
increased significantly. Previous caesarean section
(odds ratio=24) and co-existing placenta praevia
(odds ratio=585) remained the major risk factors for
morbidly adherent placenta. With an increasing rate
of morbidly adherent placenta, more patients had
haemorrhage with a consequent increased need for
peripartum hysterectomy. No significant difference
in the hysterectomy rate of morbidly adherent
placenta in caesarean scarred uterus (19/25)
compared with unscarred uterus (8/14) was noted.
This may have been due to increased detection of
placenta praevia by ultrasound and awareness of
possible adherent placenta in the scarred uterus,
as well as more invasive interventions applied to
conserve the uterus.
Conclusion: Presence of a caesarean section scar
remained the main risk factor for morbidly adherent
placenta. Application of caesarean section should be
minimised, especially in those who wish to pursue
another future pregnancy, to prevent the subsequent
morbidity consequent to a morbidly adherent
placenta, in particular, massive postpartum haemorrhage and
hysterectomy.
New knowledge added by this study
- The incidence of morbidly adherent placenta (MAP) including its precursor has increased over the last 15 years.
- MAP can occur in a scarred or an unscarred uterus with similar risks of massive postpartum haemorrhage or hysterectomy.
- There is raised awareness of the possibility of MAP in a scarred or an unscarred uterus and the associated risks of massive postpartum haemorrhage and hysterectomy.
Introduction
Morbidly adherent placenta (MAP)—including
placenta accreta, placenta increta, and placenta
percreta—is a life-threatening condition often
associated with massive postpartum haemorrhage
(PPH) and sometimes hysterectomy.1 2 The condition
results in significant maternal morbidity, maternal
mortality, and socio-economic cost in terms of the
need for invasive surgical intervention, prolonged
hospitalisation, and admission to an intensive care
unit.
The incidence of MAP is on the rise.3 4 In a US study, Wu et al5 reported an incidence of 1 in 533
births for the period from 1982 to 2002. This was
much greater than a previous reported range of 1 in
4027 to 1 in 2510 births6 or even 1 in 70 000 births7
in the 1970s to 1980s. A similar Irish retrospective
study with 36 years of data reported a doubling of the
incidence of placenta accreta in patients with previous caesarean
section from 1.06 per 1000 deliveries before
2002 to 2.37 per 1000 deliveries from 2003 to 2010.8
A recent Canadian study also showed an incidence of
14.4 per 10 000 deliveries in 2009 to 2010.9 Although
the majority of data suggested a rise in such trend,
a few suggested otherwise. The American College
of Obstetricians and Gynecologists accepted a rate
of 1 in 2500 deliveries as the true incidence of the
condition in 2002,10 11 while a national case-control
study in the UK suggested the incidence to be only
1.7 per 10 000 pregnancies overall at the end of
2012.12
Morbidly adherent placenta is most commonly
associated with placenta praevia in women previously
delivered by caesarean section.12 13 14 Despite some
variation in the incidence of MAP, there are very few
reported trends of MAP based on data of a single
institution or within a similar population.
In this study, a retrospective review of data
within a single institution in Hong Kong was
performed to (a) identify the change in incidence of
MAP that included placenta accreta, percreta and
increta, in the context of a rising caesarean delivery
rate within a single institution over the last 15 years,
and (b) to determine the contribution of MAP
to obstetric complications, in particular, massive
PPH with consequent hysterectomy.
Methods
Patients with MAP at Queen Elizabeth Hospital,
Hong Kong, over a 15-year period from 1 January
1999 to 31 December 2013 were retrospectively
identified from the hospital database, Clinical Data
Analysis and Reporting System (CDARS). The
research protocol was approved by the hospital’s
ethics committee.
Diagnosis codes for ‘previous caesarean
section’, ‘placenta praeviae, ‘adherent placenta’
‘placenta accreta’, ‘placenta percreta’, and ‘placenta
increta’ were used. Labour ward records with cases
of obstetrics-related hysterectomy or massive PPH
(>1000 mL) were cross-examined along with the
data from CDARS to ensure no cases of MAP were
missed.
Morbidly adherent placenta was defined
primarily by a histopathology report of an adherent
placenta, in which there was invasion of placental
tissue into the inner or outer myometrium or
through the serosa of the uterus, and was termed
placenta accreta, placenta increta, and placenta
percreta, respectively. It was also defined clinically by
operative reports of a difficult manual removal with
no cleavage plane identified between the placenta
and uterus, resulting in incomplete removal or need
to leave the entire placenta in situ. Histopathology
results were reviewed for each case where available.
The medical records including admission
notes, operative record, and pathology reports
in all of the cases were individually reviewed.
Demographic data, obstetric history, the
number and type of previous caesarean sections, and
information on placenta site were collected. Details
of associated complications, in particular massive
PPH, were reviewed. The subsequent
management plan of MAP was noted and reviewed,
and included (1) conservative management (leaving
part of or the whole placenta in situ) with or without
additional invasive intervention and follow-up, or (2)
immediate invasive intervention (including uterine
or iliac artery embolisation, balloon tamponade,
uterine artery ligation, or hysterectomy).
Cases were then analysed in three different
5-year intervals to identify any changes in the rate
of MAP. These intervals were 1999 to 2003, 2004 to
2008, and 2009 to 2013. Cases of MAP were analysed
in two different groups—a group with scarred uterus
due to previous caesarean section and another group
with unscarred uterus. Their incidence, associated
risk factors, and morbidity associated with MAP
were reviewed and compared.
Statistical analyses were performed using the
Statistical Package for the Social Sciences (Windows
version 19.0; SPSS Inc, Chicago [IL], US). Chi squared
test or Fisher’s exact test for categorical variables
and independent sample t test or analysis of variance
for continuous variables were applied for analysis.
All statistical tests were two-tailed, and a P value of
<0.05 was considered statistically significant.
Results
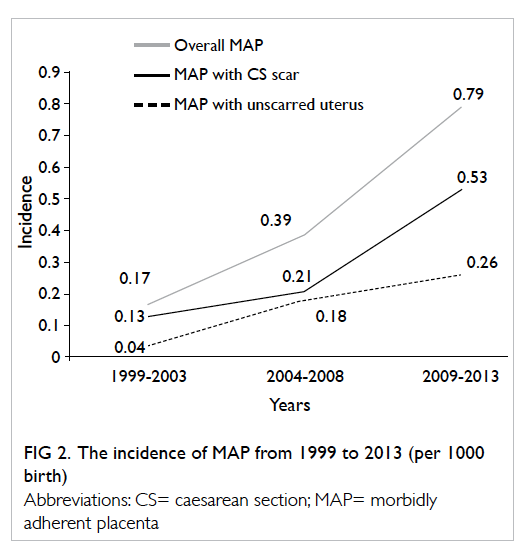
Over the 15-year study period, there were a total of
81 497 deliveries in our hospital. The mean number
of deliveries before 2004 was 4600 per year but this
figure increased dramatically to a mean of 5800
per year from 2004 to 2013. This is likely due to
the introduction of the ‘Individual Visit Scheme’ in
July 2003, where travellers from Mainland China
are allowed visits and to give birth in Hong Kong
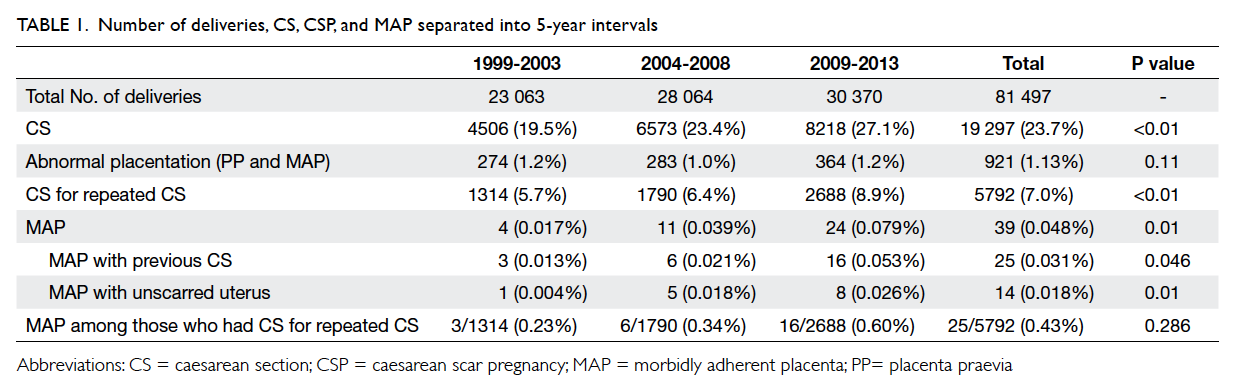
on an individual basis. The overall rate of caesarean
section during the 15-year period was 23.7% and
was increased significantly throughout the years
(P<0.01; Table 1 and Fig 1). As a result, the rate of
caesarean section due to previous caesarean section
also significantly increased from 5.7% in 1999-2003
to 8.9% in 2009-2013 (P<0.01; Table 1 and Fig 1).
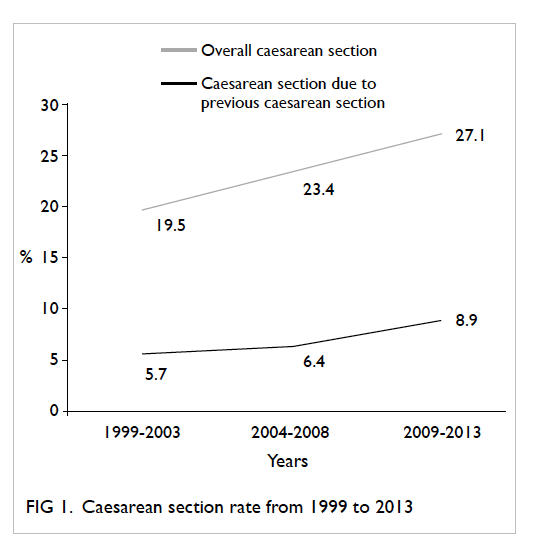
A total of 39 cases of MAP were identified.
The overall rate of MAP was 0.48 per 1000 births,
which has been increased significantly from 1999
to 2013 (P=0.01). Of the 39 cases of MAP, 25 cases
were in a scarred uterus and all deliveries were by
caesarean section; 14 cases were from an unscarred
uterus, of which four were vaginal deliveries and 10
were caesarean section. There were three cases of
placenta percreta and 36 cases of placenta accreta.
The increasing rate of MAP persisted even after
subcategorisation into previous caesarean section
scar or unscarred uterus (Table 1 and Fig 2). There
was also an increasing trend of MAP with caesarean
section scar among cases that had repeated caesarean
section, although the increase was not significant
(P=0.286; Table 1).
The overall incidence of MAP in previous
caesarean section was 0.43% compared with only
0.018% in those with an unscarred uterus. The odds
ratio (OR) of MAP in previous caesarean section was
24 compared with that of unscarred uterus (P<0.05;
95% confidence interval [CI], 12.2-45.2).
Among all the cases of placenta praevia
during the study period, the incidence did not differ
significantly with time and remained an average
of 1.13% (P=0.11; Table 1). Among the 39 cases of MAP, 34 cases had pre-existing placenta praevia.
Placenta praevia remained a major risk factor in the
development of MAP (OR=585; 95% CI, 228.3-1399.7).
Cases with MAP and a previous caesarean
section were compared with those with an unscarred
uterus. The presence of placenta praevia with a
previous scar increased the risk of MAP significantly
(P<0.01; Table 2). There were no significant differences between the two groups for the majority
of other additional underlying risk factors for MAP.
These included mean parity, maternal age, gestational
age at delivery, and the number of previous surgical
termination of pregnancy or surgical evacuations
(Table 2). Overall, there was one case of MAP following in-vitro fertilisation–induced pregnancy
but no cases had a history of hysteroscopic surgery
or a history of uterine artery embolisation.
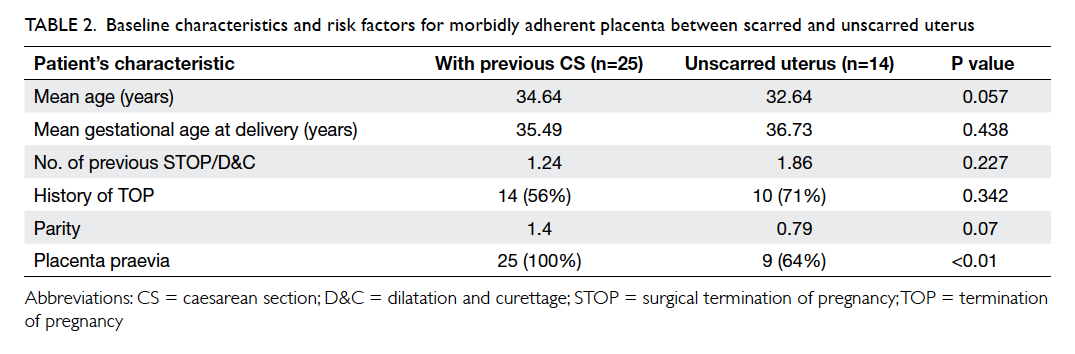
Table 2. Baseline characteristics and risk factors for morbidly adherent placenta between scarred and unscarred uterus
Management of morbidly adherent placenta
in scarred versus unscarred uterus
Among the 39 cases of MAP, 14 cases were from an
unscarred uterus, thus there had been no antenatal
suspicion of a possible MAP. Among the remaining
25 cases where MAP was found in a scarred uterus,
24 cases had placenta praevia diagnosed on antenatal
ultrasonography (USG) and one case had no previous
antenatal USG documentation of placental site. In
three cases, there was antenatal suspicion of placenta
accreta with additional measurement made of the
lower segment thickness by USG. None of the three
cases had signs of MAP, thus no antenatal diagnosis
was made or caesarean hysterectomy planned. For
all cases with co-existing placenta praevia diagnosed
antenatally, counselling including the risk of PPH,
need for multiple medical/surgical interventions
and hysterectomy as a last resort was given prior to
caesarean section.
In terms of the diagnosis of MAP, 27 (69%)
cases were confirmed histologically following
hysterectomy. The remaining 12 were diagnosed
clinically. Among those confirmed histologically, 19
cases were from a scarred uterus and eight from an
unscarred uterus. Of 19 cases from a scarred uterus,
11 had undergone previous intervention (uterine
artery embolisation, uterine artery ligation, or
balloon tamponade) before hysterectomy compared
with one in eight cases of unscarred uterus (Table 3).
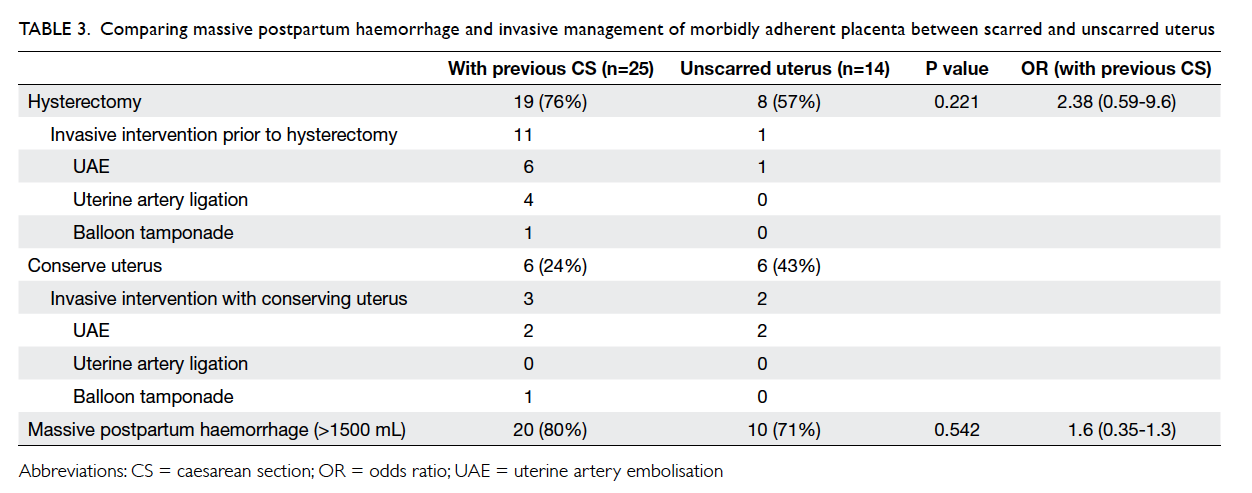
Table 3. Comparing massive postpartum haemorrhage and invasive management of morbidly adherent placenta between scarred and unscarred uterus
Conservative management with the MAP
tissue left in situ was applied in 12 (31%) cases
of MAP (6 cases from each group): three of the
scarred uterus cases required additional invasive
interventions compared with two of the six cases with
unscarred uterus (Table 3). Three cases defaulted from subsequent follow-up and the remaining nine
cases resolved completely in 8 to 49 weeks’ time.
The majority of cases of MAP in patients with
scarred and unscarred uterus were complicated by
massive PPH of >1500 mL (80% vs 71%). The
rate of hysterectomy in both groups was high: 76%
in the scarred uterus group and 57% in unscarred
uterus group (Table 3), although the difference was not significant.
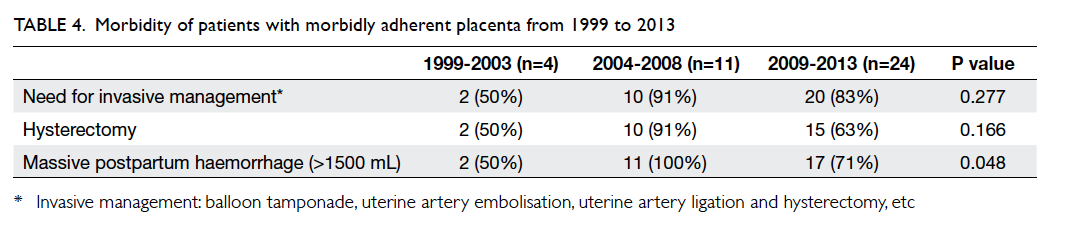
Overall morbidity of morbidly adherent placenta
Throughout the 15-year study period, there was
a significant increase in the proportion of MAP
associated with massive PPH (P=0.048). Thus there
was a consequent increased trend, although not
significant, in the need for invasive intervention and
hysterectomy (Tables 4 and 5), which is a life-saving
last-resort procedure in the management of massive PPH.
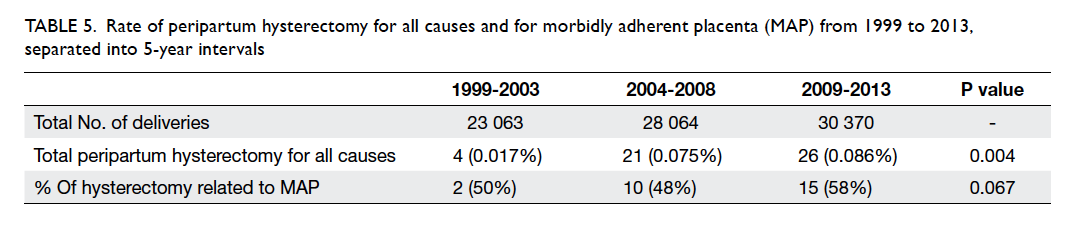
Table 5. Rate of peripartum hysterectomy for all causes and for morbidly adherent placenta (MAP) from 1999 to 2013, separated into 5-year intervals
Discussion
The data derived from this retrospective study
demonstrate a significant increase in the total
number of deliveries and caesarean sections from
1999 to 2013. With an increasing caesarean section
rate, the number of repeated caesarean sections
also increased. Possible explanations include the
high caesarean section rates in China and concerns
about the reported 4.5 per 1000 risk of previous
caesarean scar rupture.15 An alternative explanation
is the large proportion of patients who declined a
vaginal birth after a previous caesarean section or
who declined induction of labour after a previous
caesarean section. It has been reported that up to
32% to 46% of patients with a history of caesarean
section decline induction.16 The rate of MAP hence
increased as a result of more previous caesarean
sections and concurs with the findings from other
countries.3 4 5 6 7 8 Our study further demonstrated an almost tripling of incidence of MAP in the presence
of previous caesarean section from 0.23 to 0.60 per
1000 births during 2009 to 2013. This may be due to
an increasing awareness of the increasing trend of
MAP, especially in those with a caesarean scar.
Previous caesarean section scar has been
identified as one of the most important risk factors
for MAP. Our study demonstrated a 24 times
greater likelihood of developing MAP with previous
caesarean section scar compared with unscarred
uterus. Placenta praevia in the presence of a previous
caesarean section scar was 585 times more likely to
develop into a MAP. Nonetheless our data failed to
determine other reported demographics17 and risk
factors such as mean parity, maternal age, gestational
age at delivery, and previous surgical termination or
surgical evacuation. Previous surgery on the uterus
other than caesarean section (eg myomectomy)
may also predispose to MAP but among our cases
of adherent placenta, no patient had such a history
so comparisons could not be made. As a result,
every effort should be made to avoid caesarean
section delivery and hence reduce subsequent MAP
development.
Morbidly adherent placenta was more likely in
a scarred uterus although it could also occur in an
unscarred uterus. Although the majority of patients
with MAP in our study had a caesarean scar, 36% had
an unscarred uterus. The mean number of surgical
termination of pregnancy or surgical evacuation of
the uterus in the unscarred uterus group was 1.86
compared with 1.24 in the caesarean section scarred
uterus group. In addition, in the unscarred uterus
group, 71% of patients had a history of surgical
termination of pregnancy compared with 56% in the
caesarean section scarred uterus group, although the
difference was not significant. A recent case study has
reported an abnormally invasive placenta as a result
of uterine scarring in a patient with Asherman’s
syndrome.18 Therefore, awareness of the possible
development of MAP is important in pregnant
women with a history of intrauterine procedure
without caesarean section scar or placenta praevia.
The management of patients with complications
associated with MAP can be challenging. Patients
are more likely to develop massive PPH
with a consequent need for intra-operative invasive
intervention (eg balloon tamponade, uterine artery
ligation/embolisation, and hysterectomy) and
hysterectomy compared with those with a normally
adherent placenta.19
Our data clearly demonstrated an increase
in the incidence of massive PPH as the
incidence of MAP increases. The rate of peripartum
hysterectomy associated with MAP also showed
an increasing trend, albeit insignificant. This could
be due to advances in management, including
increasing USG detection of placenta praevia in the
early antenatal period and awareness of a possibly
adherent placenta in cases with a scarred uterus
that facilitates a delivery plan, as well as multiple
interventions (balloon tamponade, uterine artery
embolisation, uterine artery ligation) attempted
in cases with MAP to conserve the uterus as far as
possible. This was reflected by the increased need for
invasive interventions throughout the study period
although not to a significant degree, possibly due to
the small sample size.
Limitations
This was a retrospective overview of our hospital
data over the last 15 years. Data obtained during
the earlier years when the hospital’s Clinical Record
System was first introduced may be inaccurate.
Similarly, historical data were available for only this
15-year period. Given the overall low incidence of
MAP and the limited data available, the strength of
the statistical significance may well be challenged.
In addition, caesarean scar pregnancy, which is a
precursor of MAP, was not included in this study as
the number of cases was too small and no systemic
data were available. Previous studies have shown
that leaving the placenta in situ can reduce the rate
of hysterectomy.20 This issue was not investigated in
this study.
Conclusion
This study demonstrated that the incidence of MAP
has increased over the last 15 years. The results also
remind clinicians that MAP is much more likely to
occur if a previous caesarean scar is present (OR=24),
in particular when it is associated with a placenta
praevia (OR=585). The increased caesarean section
rate and subsequent previous caesarean section
scar were major causes for such increase. Morbidly
adherent placenta resulted in an increasing, albeit
insignificant, trend for massive PPH, and the need
for multiple invasive interventions or hysterectomy
over the last 15 years. Early suspicion and diagnosis
is essential to prevent major obstetric complications,
as well as to aid management of massive PPH
resulting from placenta complications. Every effort
should be made to avoid unnecessary caesarean
section, not only to meet the international caesarean
section rate target but also to reduce the overall
incidence of MAP that may result in significant
maternal morbidity and mortality, as well as socio-economic
costs.
References
1. Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity
associated with multiple repeat cesarean deliveries. Obstet
Gynecol 2006;107:1226-32. Crossref
2. Esakoff TF, Sparks TN, Kaimal AJ, et al. Diagnosis and
morbidity of placenta accreta. Ultrasound Obstet Gynecol
2011;37:324-7. Crossref
3. Chattopadhyay SK, Kharif H, Sherbeeni MM. Placenta
praevia and accreta after previous caesarean section. Eur J
Obstet Gynecol Reprod Biol 1993;52:151-6. Crossref
4. To WW, Leung WC. Placenta previa and previous cesarean
section. Int J Gynaecol Obstet 1995;51:25-31. Crossref
5. Wu S, Kocherginsky M, Hibbard JU. Abnormal
placentation: twenty-year analysis. Am J Obstet Gynecol
2005;192:1458-61. Crossref
6. Pridjian G, Hibbard JU, Moawad AH. Cesarean: changing
the trends. Obstet Gynecol 1991;77:195-200. Crossref
7. Breen JL, Neubecker R, Gregori CA, Franklin JE Jr. Placenta
accreta, increta, and percreta. A survey of 40 cases. Obstet
Gynecol 1977;49:43-7.
8. Higgins MF, Monteith C, Foley M, O’Herlihy C. Real
increasing incidence of hysterectomy for placenta accreta
following previous caesarean section. Eur J Obstet Gynecol
Reprod Biol 2013;171:54-6. Crossref
9. Mehrabadi A, Hutcheon JA, Liu S, et al. Contribution
of placenta accreta to the incidence of postpartum
hemorrhage and severe postpartum hemorrhage. Obstet
Gynecol 2015;125:814-21. Crossref
10. Timor-Tritsch IE, Monteagudo A. Unforeseen
consequences of the increasing rate of cesarean deliveries:
early placenta accreta and cesarean scar pregnancy. A
review. Am J Obstet Gynecol 2012;207:14-29. Crossref
11. ACOG Committee on Obstetric Practice. ACOG
Committee opinion. Number 266, January 2002: placenta
accreta. Obstet Gynecol 2002;99:169-70.
12. Fitzpatrick KE, Sellers S, Spark P, Kurinczuk JJ, Brocklehurst
P, Knight M. Incidence and risk factors for placenta accreta/increta/percreta in the UK: a national case-control study.
PLoS One 2012;7:e52893. Crossref
13. Romero R, Hsu YC, Athanassiadis AP, et al. Preterm
delivery: a risk factor for retained placenta. Am J Obstet
Gynecol 1990;163:823-5. Crossref
14. Parazzini F, Dindelli M, Luchini L, et al. Risk factors for
placenta praevia. Placenta 1994;15:321-6. Crossref
15. Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP.
Risk of uterine rupture during labor among women with a
prior cesarean delivery. N Engl J Med 2001;345:3-8. Crossref
16. Dodd JM, Crowther CA, Grivell RM, Deussen AR. Elective
repeat caesarean section versus induction of labour
for women with a previous caesarean birth. Cochrane
Database Syst Rev 2014;(12):CD004906. Crossref
17. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors
for placenta previa–placenta accreta. Am J Obstet Gynecol
1997;177:210-4. Crossref
18. Engelbrechtsen L, Langhoff-Roos J, Kjer JJ, Istre O. Placenta
accreta: adherent placenta due to Asherman syndrome.
Clin Case Rep 2015;3:175-8. Crossref
19. Lee MM, Yau BC. Incidence, causes, complications,
and trends associated with peripartum hysterectomy
and interventional management for postpartum
haemorrhage: a 14-year study. Hong Kong J Gynaecol
Obstet Midwifery 2013;13:52-60.
20. Fitzpatrick KE, Sellers S, Spark P, Kurinczuk JJ,
Brocklehurst P, Knight M. The management and outcomes
of placenta accreta, increta, and percreta in the UK: a
population-based descriptive study. BJOG 2014;121:62-71. Crossref