© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF MEDICAL SCIENCES
Water sampler
Samson SY Wong, FRCPath, FHKCPath
Member, Education and Research Committee, Hong Kong Museum of Medical Sciences Society
Among the collection of artefacts at the Hong
Kong Museum of Medical Sciences, some are less
glamorous than others. One example is a home-made
water sampler that comprises nothing more
than a glass flask tied to a lead sinker and an iron
basket (Fig 1). When lowered to the desired depth,
the stopper of the container was opened by means of
a string. This simple equipment was used by the old
Bacteriological Institute to obtain a sample of local
sources of potable water to test quality including
measurement of bacterial counts. Technically,
there is nothing complicated about the item, but it
reminds us of one of the key roles of a public health
laboratory.

Figure 1. A home-made water sampler for testing water quality used by the old Bacteriological Institute
When the Bacteriological Institute was
established in 1906 in the wake of the 1894 plague
outbreak (during which the aetiological agent
of plague was discovered in Hong Kong), one
of its key duties was the surveillance of plague
and ectoparasites in captured rats. In the first
Government Bacteriologist Annual Report of 1902,
117 839 rats were examined in 1 year for evidence
of plague.1 The report also reviewed the causes of
death as revealed by postmortem examination at the
Government Public Mortuary. From 1906 onwards,
bacteriological examination of public water supplies
began. Water was collected from Pokfulam, Taitam,
and Cheung Sha Wan supplies, as well as from well
and nullah water.2 From the start of monitoring, the
microbiological quality of potable water in Hong
Kong has been maintained at a very high quality.
The provision of a safe water supply has no doubt
played a crucial role in reducing the incidence of
waterborne infections in Hong Kong.
Two classic waterborne infectious diseases,
enteric fever (consisting mainly of typhoid and
paratyphoid fevers) and cholera, featured in the
earliest Report of the Government Bacteriologist. It
was noted that “a very severe outbreak of this disease
[cholera] occurred during 1902 in Hongkong”,1 with
379 fatal cases being examined at the Government
Public Mortuary. In the same year, seven fatal
cases of typhoid fever were examined.1 With the
availability of a safe potable water supply, and hence
lesser reliance on well water and other surface waters
that are prone to faecal contamination, the annual
incidence of both cholera and typhoid/paratyphoid
fevers has substantially reduced over the years
(Fig 2).3 4 The annual number of cholera cases, for
example, has remained a single digit since 2003.4
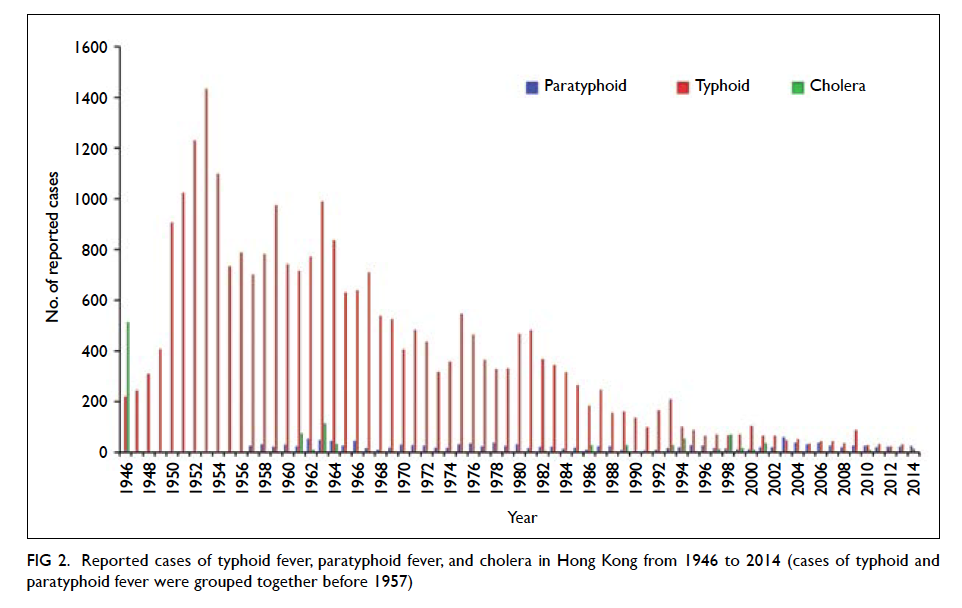
Figure 2. Reported cases of typhoid fever, paratyphoid fever, and cholera in Hong Kong from 1946 to 2014 (cases of typhoid and paratyphoid fever were grouped together before 1957)
As the local transmission of cholera and
typhoid/paratyphoid fever becomes rarer, the
epidemiology of these two diseases also changes.
Instead of being a waterborne disease, cholera has
become primarily a food-borne infection in Hong
Kong, often associated with the consumption of raw
or undercooked seafood.5 Indeed, while waterborne
outbreaks of cholera remain a significant public
health problem in developing countries, the majority
of domestic cases of cholera in developed countries
are now food-borne infections.6 Similarly, for
typhoid and paratyphoid fevers, the majority of cases
in developed countries are the result of food-borne
transmission.7 Although domestic transmission
of these infections still occurs in Hong Kong, an
increasing proportion of cases in recent years have
been imported.7 In 2009, 80% of all notified cases
of typhoid in Hong Kong were imported, especially
from Indonesia and India.8
The provision of a safe potable water supply
is one of the most cost-effective interventions
to prevent communicable diseases. The reduced
incidence of waterborne diseases in Hong Kong over
the past century bears testimony to the relationship
between water, sanitation, hygiene, and health.
References
1. Hunter W. Report of the Government Bacteriologist, for the year 1902. Government Public Mortuary, Hong Kong. 1903.
2. Anon. Report of the Government Bacteriologist, for the year 1906. Government Public Mortuary, Hong Kong. 1907.
3. Disease Prevention and Control Division, Department of Health, Hong Kong. Statistics on Infectious Diseases in Hong Kong, 1946-2001. Government of the Hong Kong Special Administrative Region. 2002.
4. Centre for Health Protection. Number of notifications for notifiable infectious diseases. Available from: http://www.chp.gov.hk/en/data/1/10/26/43/2280.html. Accessed 29 Sep 2015.
5. Scientific Committee on Enteric Infections and Foodborne Diseases, Centre for Health Protection. Epidemiology, Prevention and Control of Cholera in Hong Kong. 2011. Available from: http://www.chp.gov.hk/files/pdf/epidemiology_prevention_and_control_of_cholera_in_hong_kong_r.pdf. Accessed 14 Aug 2014.
6. Steinberg EB, Greene KD, Bopp CA, Cameron DN, Wells JG, Mintz ED. Cholera in the United States, 1995-2000: trends at the end of the twentieth century. J Infect Dis 2001;184:799-802. Crossref
7. Olsen SJ, Bleasdale SC, Magnano AR, et al. Outbreaks of typhoid fever in the United States, 1960-99. Epidemiol Infect 2003;130:13-21. Crossref
8. Scientific Committee on Enteric Infections and Foodborne Diseases, Centre for Health Protection. Epidemiology and Prevention of Typhoid Fever in Hong Kong. 2011. Available from: http://www.chp.gov.hk/files/pdf/review_of_nontyphoidal_salmonella_food_poisoning_in_hong_kong_r.pdf. Accessed 14 Aug 2014.

