DOI: 10.12809/hkmj144340
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Use of robotic-assisted laparoscopic Mitrofanoff
appendicovesicostomy in a paediatric patient: problem encountered
Ivy HY Chan, FRCSEd(Paed), FHKAM (Surgery);
Florence HQ Li, MB, ChB;
Lawrence CL Lan, FRCSEd, FHKAM (Surgery);
Kenneth KY Wong, FRCSEd, FHKAM (Surgery);
Peter KF Yip, FRCSEd, FHKAM (Surgery);
Paul KH Tam, FRCS (Edin, Glasg, Irel), FHKAM (Surgery)
Division of Paediatric Surgery, Department of Surgery, The University of
Hong Kong, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr Ivy HY Chan (ivyhychan@gmail.com)
Abstract
This report is of robotic-assisted laparoscopic
Mitrofanoff appendicovesicostomy in a 12-year-old
patient with detrusor underactivity and hereditary
sensory neuropathy. The whole operation was
performed in 555 minutes with no open conversion.
The patient experienced one episode of stomal
stenosis, which required dilatation. At 3-year
follow-up, the patient had both stomal and urinary
continence. This is a safe and effective procedure
to create a means of urinary catheterisation with
avoidance of a large unsightly scar and comparable
clinical outcome to an open procedure.
Introduction
The da Vinci Surgical System for robotic-assisted
laparoscopic surgery was approved by the US
Food and Drug Administration in 2000.1 Since
its introduction, various types of operations have
been successfully performed by robotic-assisted
laparoscopic surgery. This technique, however, is
limited by its lack of flexibility in the operative field
and the size of paediatric patients. Therefore, its use is
mainly confined in adult patients. Here, we describe
the use of robotic-assisted laparoscopic Mitrofanoff
appendicovesicostomy in a paediatric patient with
detrusor underactivity and sensory neuropathy.
Case report
In September 2009, a 12-year-old girl with hereditary
sensory neuropathy presented to Queen Mary
Hospital with overflow incontinence. She had a rare
hereditary sensory neuropathy, which resulted in no
pain sensation and no sensation of bladder fullness.
As well as sensory neuropathy, she had mild mental
retardation, and studied in a special school.
She presented with overflow incontinence,
difficulty in initiating voiding, long voiding time,
and large volume of post-void residual urine. The
results of investigations—including renal function
test, ultrasound of the urinary system, and magnetic
resonance imaging of the lumbosacral spine—were
normal. Video urodynamics revealed poor bladder
sensation despite high detrusor pressure, low voiding
detrusor pressure, and incomplete emptying. The
overall impression was detrusor underactivity.
The initial treatment plan was for transurethral
clean intermittent urinary catheterisation (CIC) to
be performed regularly by the patient’s caregiver.
Because of the patient’s mental status and
uncooperability, however, she could not tolerate
CIC. After thorough discussion, the patient’s parents
agreed to the patient undergoing Mitrofanoff
appendicovesicostomy.
The operation was performed in a
Trendelenburg position. A 12-mm camera port
was placed at the circumumbilical position. Two
8-mm working ports were placed one each at the
left lower quadrant and right upper quadrant. A
5-mm assistant port was placed at the epigastric
area, mainly for bowel retraction and passing sutures
(Fig).
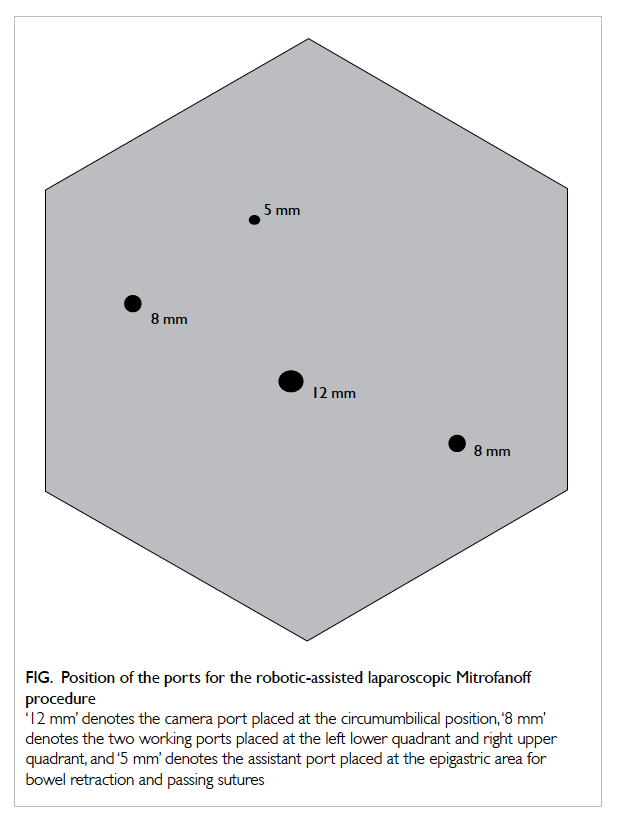
Figure. Position of the ports for the robotic-assisted laparoscopic Mitrofanoff procedure
‘12 mm’ denotes the camera port placed at the circumumbilical position, ‘8 mm’ denotes the two working ports placed at the left lower quadrant and right upper quadrant, and ‘5 mm’ denotes the assistant port placed at the epigastric area for bowel retraction and passing sutures
Preoperative intravenous antibiotics of
amoxicillin-clavulanic acid 30 mg/kg were
administered. A urinary catheter was inserted under
aseptic conditions. The appendix was mobilised
with its mesentery. However, the appendix and its
mesentery appeared to be relatively short (appendix
was approximately 6 cm and mesentery was
approximately 4 cm) in this patient so the right colon
was mobilised en bloc up to the hepatic flexure to
create mobility of the appendix and its mesentery.
Initial mobilisation of the right colon
and bladder was performed with conventional
laparoscopy. The robotic system was docked in to
perform the anastomosis between the bladder and
appendix.
The urinary bladder was partially infused with
normal saline via the urinary catheter. The tip of
the appendix was opened and an 8-French infant
feeding tube was inserted to ease manipulation of
the appendix. The detrusor muscle was incised and
opened by electrocautery at the supero-anterior
aspect of the urinary bladder. Appendicovesicostomy
was performed with 5/0 vicryl in an interrupted
manner. The other end of the appendix was retrieved
at the right lower quadrant of the abdominal wall. A
V flap was created and the stoma was fashioned with
5/0 vicryl. The infant feeding tube was kept in situ as
a stent. The whole operation took 555 minutes (9.25
hours).
The patient’s recovery was complicated by
urinary tract infection with extended-spectrum beta-lactamase–producing Escherichia coli. Intravenous
meropenem 20 mg/kg every 8 hours was initiated
for 14 days. The infant feeding catheter was removed
and the technique of CIC was taught to the patient’s
caregiver.
The continence outcome was good as reported
by the patient’s caregiver. There was no urine leak
from the stoma or urethra. The technique of CIC with
an 8-French catheter 4 times a day was performed
uneventfully by the patient’s caregiver until around 6
months after the operation, when examination under
anaesthesia and cystogram found mild stenosis of
the stoma. Serial dilatation of the stoma site was
suggested. There is no urine leak until the bladder
reaches 400 mL in capacity. At 3-year follow-up, the
patient’s caregiver can catheterise the bladder with
ease and the patient has both stomal and urinary
continence.
Discussion
The Mitrofanoff procedure was described in 1980.2
It uses the appendix to create a channel from the
urinary bladder to the skin surface. This procedure
has helped many patients who cannot tolerate
urethral catheterisation over the past three decades.
The procedure, however, was done via a conventional
open surgery approach until 1993, when Jordan and
Winslow3 described the technique of laparoscopic-assisted
appendicovesicostomy. Despite the benefit
of minimally invasive surgery, this technique has not
become popular. In 2004, Pedraza et al4 and Hsu and
Shortliffe5 described the use of the robotic-assisted
technique in creating an appendicovesicostomy.
Since then, a few case reports or case series6 7 8 have
described this technique. This is largely attributed
to the delicacy of the appendiceal blood supply
and challenging intracorporeal anastomosis. The
surgical robot offers three-dimensional visualisation,
downscaling of surgeons’ tremor and hand
movements, range of motion resembling that of the
human wrist, and increased degrees of freedom.
The benefits of applying robotic technology
for this procedure are greatest at two stages: first
when dissecting the appendiceal blood supply and
second when recreating a circumferential sealed
anastomosis joining the appendix and bladder.
Maintaining the blood supply to the appendix is one
of the most important steps for avoiding cutaneous
stomal stenosis and scarring. The challenge of
making an intracorporeal watertight anastomosis
may also be an important reason for the scarce
reports of the pure laparoscopic approach for this
technique. In view of this, there is no doubt that the
surgical robot has a fine ability to mimic the open
procedure without introducing a large unsightly
abdominal incision.
On the other hand, the operative field is limited
with the robotic system. This created a problem for
this patient, as the appendix and its mesentery was
short. The robotic machine was docked towards
the feet of the patient and the targeted area of
interest was at the pelvis and right lower quadrant.
During mobilisation of the upper part of the right
colon, crowding of instruments was encountered.
As the port was placed as shown in the Figure, the operative field was fixed in the right lower quadrant.
For mobilisation of the right colon, the operative
field moved from the right lower quadrant to the
right upper quadrant. The robotic instruments
were not sufficiently flexible for the different
surgical fields required for this patient, so we
reverted to conventional laparoscopic mobilisation
of the right colon. This necessitated more time
to redock the whole system back to perform the
appendicovesicostomy anastomosis. This is one of
the drawbacks of the robotic-assisted Mitrofanoff
procedure.
The short-term and mid-term outcomes of this
patient are good. She recovered well and became fully
mobilised on day 3 after operation. The continence
outcome of this patient is good, and the caregiver
also found this helpful for doing CIC for this patient.
Conclusion
The robotic-assisted laparoscopic Mitrofanoff
procedure is a feasible and safe operation. The
technique has the advantage of performing the
delicate anastomosis between the appendix and the
bladder intracorporeally. Lack of flexibility when
changing the surgical field is the major drawback.
The robotic-assisted laparoscopic Mitrofanoff
procedure can produce a smaller scar and better
cosmetic outcome.
References
1. Meadows M. Computer-assisted surgery: an
update. Available from: http://web.archive.org/web/20090301135726/http://www.fda.gov/fdac/features/2005/405_computer.html. Accessed 9 Jul 2015.
2. Mitrofanoff P. Trans-appendicular continent cystostomy
in the management of the neurogenic bladder [in French].
Chir Pediatr 1980;21:297-305.
3. Jordan GH, Winslow BH. Laparoscopically assisted
continent catheterizable cutaneous appendicovesicostomy.
J Endourol 1993;7:517-20. Crossref
4. Pedraza R, Weiser A, Franco I. Laparoscopic
appendicovesicostomy (Mitrofanoff procedure) in a child
using the da Vinci robotic system. J Urol 2004;171:1652-3. Crossref
5. Hsu TH, Shortliffe LD. Laparoscopic Mitrofanoff
appendicovesicostomy. Urology 2004;64:802-4. Crossref
6. Storm DW, Fulmer BR, Sumfest JM. Laparoscopic robot-assisted
appendicovesicostomy: an initial experience. J
Endourol 2007;21:1015-8. Crossref
7. Thakre AA, Yeung CK, Peters C. Robot-assisted
Mitrofanoff and Malone antegrade continence enema
reconstruction using divided appendix. J Endourol
2008;22:2393-6. Crossref
8. Willie MA, Zagaja GP, Shalhav AL, Gundeti MS.
Continence outcomes in patients undergoing robotic
assisted laparoscopic mitrofanoff appendicovesicostomy. J
Urol 2011;185:1438-43. Crossref

