Hong Kong Med J 2015 Aug;21(4):375.e1–2
DOI: 10.12809/hkmj154530
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Acute basilar artery occlusion: an easily missed uncommon but devastating emergency
WP Chu, FRCR, FHKAM (Radiology);
WC Wong, FRCR, FHKAM (Radiology);
Bill A Lo, FRCR, FHKAM (Radiology);
KK Lai, FRCR, FHKAM (Radiology)
Department of Radiology, Tseung Kwan O Hospital, Tseung Kwan O, Hong Kong
Corresponding author: Dr WP Chu (drvictorchu@yahoo.com)
A 55-year-old man was admitted in August 2014
as an emergency with sudden onset of vertigo,
dizziness, and left-sided weakness. Initial Glasgow
Coma Scale score was 15/15. Physical examination
revealed left hemiparesis and an upgoing left plantar
response. Both pupils were reactive with the left one
slightly smaller than the right. Muscle power was
grade 4 over 5 for the left upper and lower limbs.
Urgent computed tomography (CT) examination of
the brain revealed a hyperdense basilar artery, which
was initially unnoticed (Fig 1). Subsequently, the
patient’s level of consciousness rapidly decreased and
intubation was required. Urgent magnetic resonance
angiography (MRA) identified loss of flow-related
signals along the basilar artery (Fig 2). Diffusion-weighted
imaging (DWI) found restricted diffusion at
the pons and bilateral cerebellar hemispheres (Fig 3).
The brainstem appeared normal on the T2-weighted
images and there was loss of flow void at the basilar
artery (Fig 4). These neuroimaging findings were
consistent with acute occlusion of the basilar artery,
cytotoxic oedema at the brainstem and bilateral
cerebellum. The patient died a week later despite
intensive medical intervention.
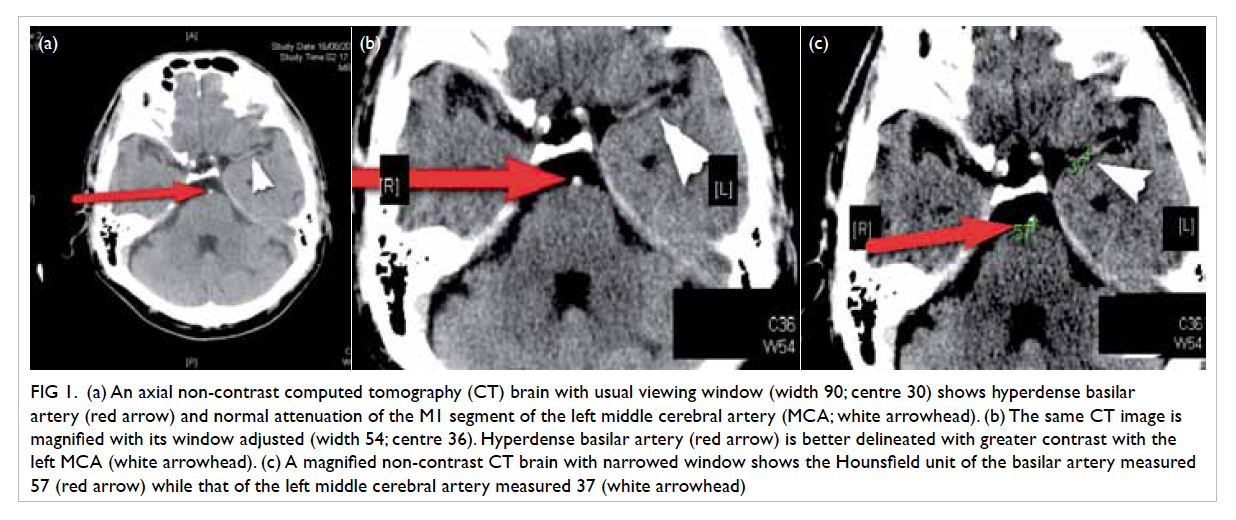
Figure 1. (a) An axial non-contrast computed tomography (CT) brain with usual viewing window (width 90; centre 30) shows hyperdense basilar artery (red arrow) and normal attenuation of the M1 segment of the left middle cerebral artery (MCA; white arrowhead). (b) The same CT image is magnified with its window adjusted (width 54; centre 36). Hyperdense basilar artery (red arrow) is better delineated with greater contrast with the left MCA (white arrowhead). (c) A magnified non-contrast CT brain with narrowed window shows the Hounsfield unit of the basilar artery measured 57 (red arrow) while that of the left middle cerebral artery measured 37 (white arrowhead)
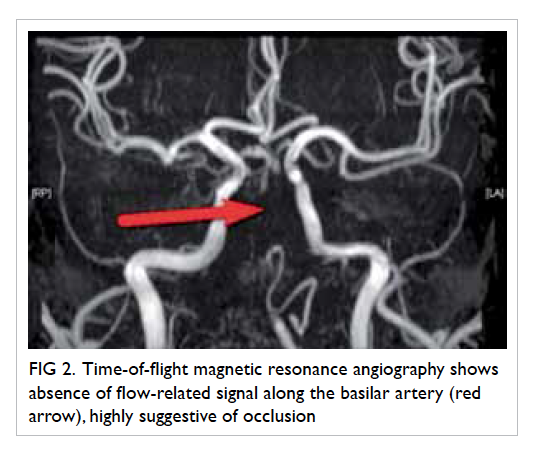
Figure 2. Time-of-flight magnetic resonance angiography shows absence of flow-related signal along the basilar artery (red arrow), highly suggestive of occlusion
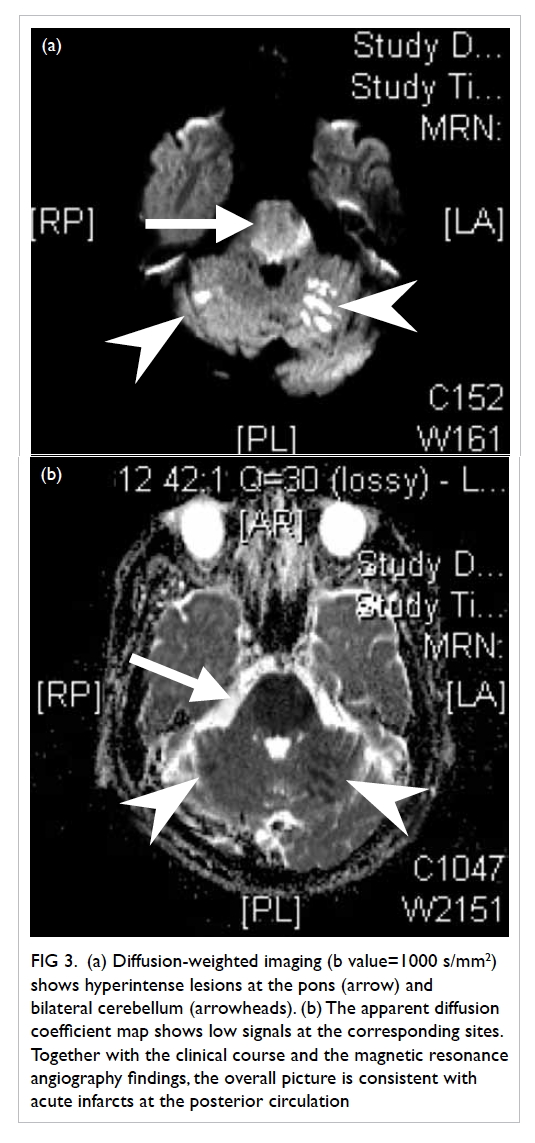
Figure 3. (a) Diffusion-weighted imaging (b value=1000 s/mm2) shows hyperintense lesions at the pons (arrow) and bilateral cerebellum (arrowheads). (b) The apparent diffusion coefficient map shows low signals at the corresponding sites. Together with the clinical course and the magnetic resonance angiography findings, the overall picture is consistent with acute infarcts at the posterior circulation
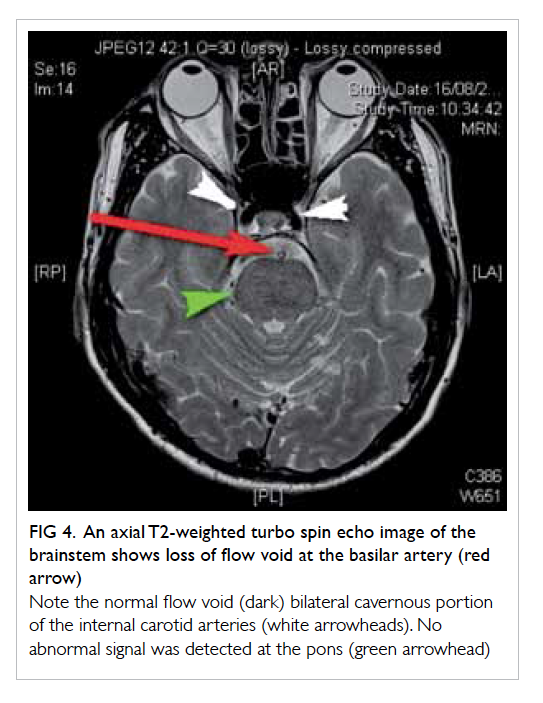
Figure 4. An axial T2-weighted turbo spin echo image of the brainstem shows loss of flow void at the basilar artery (red arrow)
Note the normal flow void (dark) bilateral cavernous portion of the internal carotid arteries (white arrowheads). No abnormal signal was detected at the pons (green arrowhead)
Acute basilar occlusion is a true neurological
emergency. Early diagnosis and treatment are
essential to prevent brainstem infarct and death. It
is uncommon and accounts for 1% of all strokes.1
Nonetheless, when present, a hyperdense basilar
artery is evident on non-contrast CT images in
approximately 65% of patients2 and enables the
diagnosis to be confirmed. Hyperdensity at the
occluded basilar artery is due to an intraluminal
blood clot and is analogous to the ‘hyperdense middle
cerebral artery sign’ of acute thromboembolism of
middle cerebral artery.
A very high index of suspicion is required
because CT findings can be subtle. Diagnosis
requires careful scrutiny of the basilar artery and the
posterior circulation. Hyperdense basilar artery may
be the only sign before development of an established
infarct. Pitfalls to diagnosis include vascular wall
calcification secondary to atherosclerosis, partial
volume averaging, haematocrit elevation, and vessel
dilation. Meticulous evaluation of the CT images
of thin collimation and narrowed window, careful
comparison of the density of the basilar artery with
other intracranial vessels and previous CT images,
if available, will be helpful. A blood clot within
the basilar artery will present as a hyperdense
intraluminal filling defect. Vascular calcification may
present as rim or curvilinear peripheral hyperdensity.
In patients with hemo-concentration, there should
be generalised increased attenuations of the
intracerebral vasculature instead of focal abnormality.
Both magnetic resonance imaging (MRI) and MRA
can demonstrate the extent of vascular occlusion and
the secondary changes including cytotoxic oedema
for patients with diagnostic uncertainty. Limited
sequences, including time-of-flight MRA and DWI,
may be performed within 15 minutes. Of note,
DWI is the most sensitive MRI technique to detect
cytotoxic oedema before radiological changes are
evident on other MRI sequences. Close collaboration
between the neurologists, the neuro-interventional
radiologists, and neurosurgeons is essential for the
management of such patients. Treatment options
include intravenous thrombolysis, catheter-directed
intra-arterial thrombolysis, and endovascular
mechanical thrombectomy. The best approach,
however, needs to be defined by future large-scale
studies.
References
1. Goldmakher GV, Camargo EC, Furie KL, et al. Hyperdense
basilar artery sign on unenhanced CT predicts thrombus
and outcome in acute posterior circulation stroke. Stroke
2009;40:134-9. Crossref
2. Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ,
Schroth G. Basilar artery occlusion. Lancet Neurol
2011;10:1002-14. Crossref

