DOI: 10.12809/hkmj144326
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Prevention in primary care is better than cure: The Hong Kong Reference Framework for
Preventive Care for Older Adults—translating evidence into practice
Cecilia KL Sin, MB, BS, FHKAM (Family Medicine)1;
SN Fu, MB, BS, FHKAM (Family Medicine)1;
Caroline SH Tsang, MB, ChB, FHKAM (Community Medicine)1;
Wendy WS Tsui, MB, ChB, FHKAM (Family Medicine)1;
Felix HW Chan, MBBCh, FHKAM (Medicine)2
1 Primary Care Office, Department of Health, Hong Kong
2 Clinical Advisory Group on Reference Framework for Preventive Care for
Older Adults in Primary Care Settings, Hong Kong
Corresponding author: Dr Caroline SH Tsang (caroline_tsang@dh.gov.hk)
Abstract
An ageing population is posing a great challenge
to Hong Kong. Maintaining health and functional
independence among older adults is of utmost
importance, and requires the collaborative efforts of
multiple health care disciplines from both the private
and public sectors. The Reference Framework for
Preventive Care for Older Adults, developed by the
Task Force on Conceptual Model and Preventive
Protocols under the auspices of the Working Group
on Primary Care, aims to enhance primary care for
this population group. The reference framework
emphasises a comprehensive, integrated, and
collaborative approach that involves providers of
primary care from multiple disciplines. In addition to
internet-based information, helpful tools in the form
of summary charts and Cue Cards are also produced
to facilitate incorporation of recommendations by
primary care providers into their daily practice. It
is anticipated that wide adoption of the reference
framework will contribute to improving older adults’
health in our community.
Introduction
Advances in medicine and increased life expectancy
mean that Hong Kong is expecting an ageing
population, and a significant increase in the number
and proportion of older adults. According to the
Census and Statistics Department of Hong Kong
SAR, it is estimated that by 2041, the number of
Hong Kong residents aged 65 years and above
will increase from 0.9 million in 2011 (13% of
the population) to around 2.6 million (30% of the
projected population).1
This ageing population poses not only a threat
but also a challenge to the current health care system.
It is anticipated that the prevalence of common
chronic diseases will be further increased with a
consequent escalating demand on various health
services for older adults. Strategies to promote
health, prevent chronic diseases, and preserve
functional ability of older adults are therefore vital.
In order to provide a general reference for
provision of continuous, comprehensive, and
evidence-based care for older adults in the primary
care setting, the Reference Framework for Preventive
Care for Older Adults in Primary Care Settings2 was
developed by the Task Force on Conceptual Model
and Preventive Protocols under the auspices of the
Working Group on Primary Care. It was developed
according to the latest research evidence, with
contributions from the Clinical Advisory Group
that comprises experts from academia, professional
organisations, private and public primary care
sectors, and patient groups.
The reference framework consists of a core
document supplemented by a series of modules that
address various aspects of disease management and
preventive care for older adults.2 To date, the core
document, and the modules on health assessment
and falls have been developed.
This article summarises the main contents and
highlights a practical use of this reference framework
to enhance the delivery of preventive care for older
adults in primary care setting in Hong Kong. Details
of the evidence that supports the recommendations
are available in the core document of the reference
framework.2
Role of primary care in the preventive care of older adults
As the first point of contact, primary care providers
are in a prime position to promote health, prevent
and monitor disease, and reduce functional
disabilities.3 Primary care physicians provide health
education, risk assessment, and follow-up care
for medical conditions. They also advise and refer
patients for appropriate health care services as
necessary, and provide support and advice to family
members and carers. It is firmly established that
patient education and counselling in the primary
care setting contributes to a better understanding of
health and can thus influence an individual to adopt
health protective behaviour.4
Only 0.5% of clinical encounters among older
people at a local primary care level are initiated
for a physical checkup.5 It has been suggested that
apart from designated appointments in primary
care settings, health assessment can be performed
opportunistically over time and during multiple
visits. Indeed, every clinic visit to a primary care
provider should be seen as an opportunity to screen
for any physical, psychological, or social problems.6 7 When one considers that 80% of the Hong Kong
population have consulted a primary care provider in
1 year, with a mean of eight primary care visits per
year,8 there is ample opportunity for primary care
providers to discuss preventive care services.
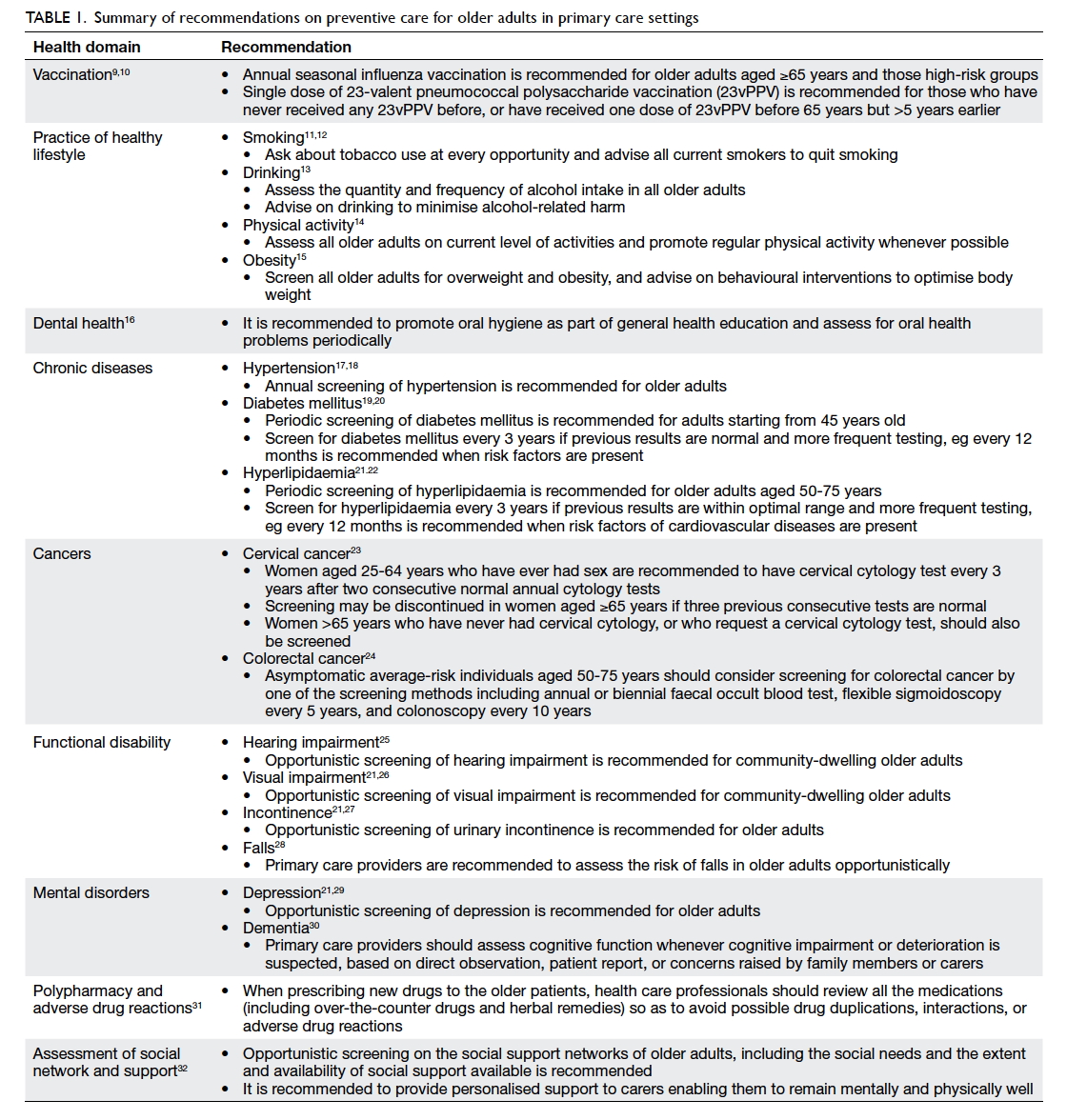
Evidence-based preventive care for older adults
The core document2 provides up-to-date evidence-based
recommendations for preventive care
of older adults in primary care setting. These
recommendations can be categorised into various
health domains, including vaccination, adoption of
a healthy lifestyle, dental health, chronic diseases,
cancers, functional disability, mental disorders,
polypharmacy and adverse drug reactions, and
assessment of social network and support. A
summary of the recommendations is listed in
Table 1.9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 Although the recommendations aim to
support primary care providers in decision-making,
the care provided for each patient should also be
individualised.
Practice of evidence-based recommendations for older adults with different functional capacity
Older adults vary in their needs and functional
capacity. In a healthy active older adult, the emphasis
will often be on health promotion and disease-prevention
activities. At the other extreme, a frail
older adult with additional special needs will require
a comprehensive assessment and formulation of an
individualised care plan. The needs and condition
of an older adult may also change over time. It is
not uncommon to see a healthy active older adult
suddenly becomes disabled following an untoward
event.
In order to formulate a personalised care
plan and effectively implement the evidence-based
recommendations, three categories of functional
capacity of older adults have been proposed—independent with no known chronic diseases,
independent with chronic diseases, and older adults
with disabilities.
For all older adults and as far as applicable,
promotion of a healthy lifestyle and early
identification and appropriate management of risk
factors—such as unhealthy diet, physical inactivity,
and tobacco use—should form the cornerstone in
prevention or management of chronic diseases. A
healthy lifestyle is known to be positively associated
with better physical and mental health as well as
longevity, reduced risk of chronic diseases, and
more quality-adjusted life years.33 34 Thus promoting
a healthy lifestyle should be one of the main focuses
in healthy ageing.
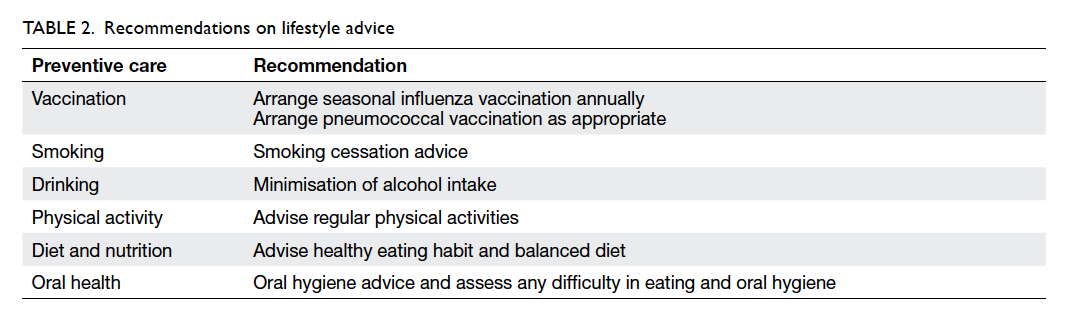
For older adults of all functional stages, a
healthy lifestyle and modification of behavioural risk
factors should be promoted as much as is practical.
Table 2 provides a summary of the recommendations.
Independent with no known chronic disease
Staying active and healthy is essential to the quality
of life. The functional decline that occurs with ageing
may be due, at least in part, to lifestyle, behaviour,
diet, and the environment, which are all modifiable
factors.35
The primary objective for this category of older
adults is to maintain optimal functional capacity
and prevent or delay the development of chronic
disease, thus helping to extend a healthy active life.
In addition to health education and promotion, a
systemic health assessment and early identification
of chronic diseases are important.
The recommended items for assessment in this
category of older adults are listed in Table 3. Details
of preventive care can be found in the respective
chapter of the core document2 and/or module
quoted in brackets.
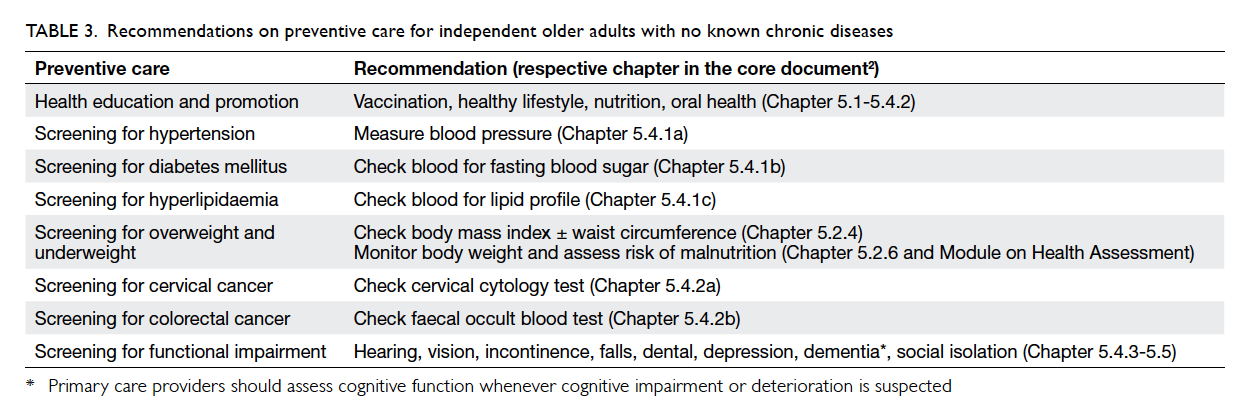
Table 3. Recommendations on preventive care for independent older adults with no known chronic diseases
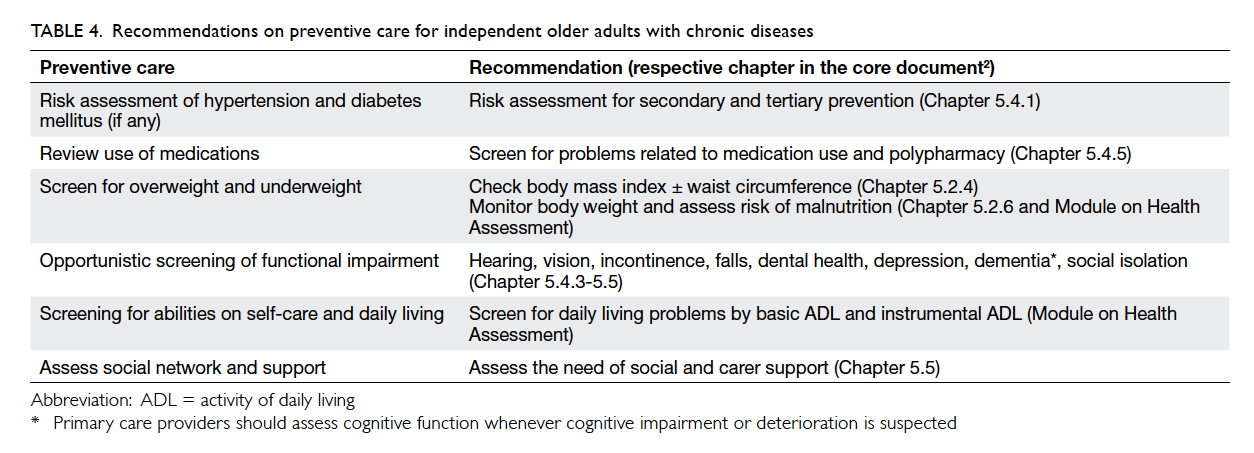
Independent with chronic diseases
Older adults with chronic diseases vary in clinical
heterogeneity, number of chronic conditions,
severity of illness, and functional limitations.
Chronic diseases exert a synergistic effect such that
the combined disabling effect of different diseases
is greater than the combined effect of each.36 As
the number of chronic diseases in an individual
increases, the risk of mortality, poor functional
status, unnecessary hospitalisations, and adverse
drug events also increases.37 38 39 Multiple chronic
diseases can be accompanied by loss of function,
reduced independence, and increased risk of
depressive illness. These subsequently contribute to
frailty and disability.37 40
The objectives of preventive services in these
older adults are to appropriately manage their
chronic diseases with reference to both secondary
and tertiary prevention, as well as to maintain
functional independence. The recommendations on
preventive care for independent older adults with
chronic diseases are summarised in Table 4. Details
about preventive care can be found in the relevant
chapter of the core document and/or module quoted
in brackets.2
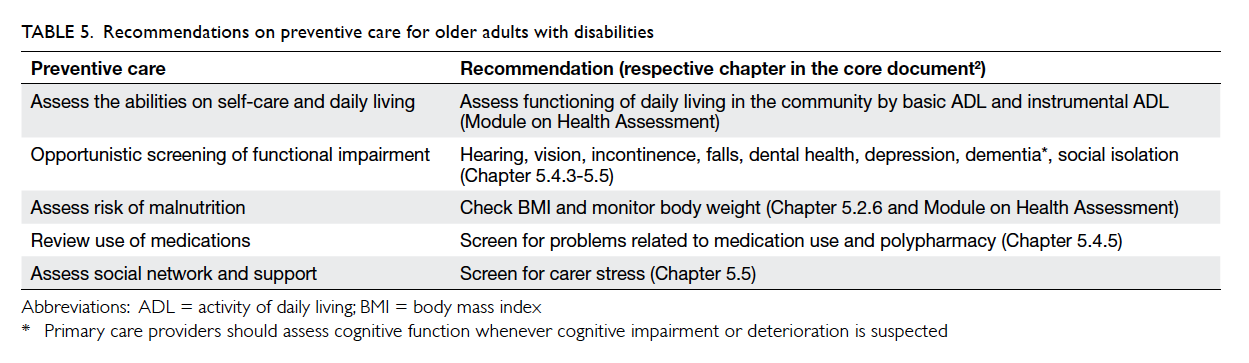
Older adults with disabilities
Older adults who suffer multiple debilitating diseases
(such as stroke, dementia, or arthritis) are likely to
face disabling barriers that inhibit or prevent their
integration into the community. Chronic pain is also
common in this group of older adults and invariably
jeopardises physical, psychological, and social
wellbeing.
The approach to this group is early intervention
to prevent further loss of function, so as to maintain
optimal functional capacity and improve quality
of life, and also facilitate integration into society
for those who have relatively mild disability. A
comprehensive assessment should be offered to
this group of older adults with complex needs, and
should encompass physical, psychological, and social
aspects of care (eg ability in self-care, hearing and
visual impairment, incontinence, falls, depression,
cognitive impairment, malnutrition, polypharmacy,
social support, and carer stress).
The recommendations on preventive care for
older adults with disabilities are listed in Table 5.
Details about preventive care can again be found in
the relevant chapter of the core document and/or
module quoted in brackets.2
The two-page summary
A 2-page summary (Fig) has been developed to
provide a quick reference for primary care providers
on preventive care for older adults. It provides a
summary of the evidence-based recommendations
for preventive activities and the practice of
recommendations for older adults with different
functional capacities. The relevant chapter of the
preventive care is stated in the summary for further
information and supporting evidence. It can also be
downloaded from the Primary Care Office website
(http://www.pco.gov.hk/english/resource/files/Summary_page_older_adult.pdf).
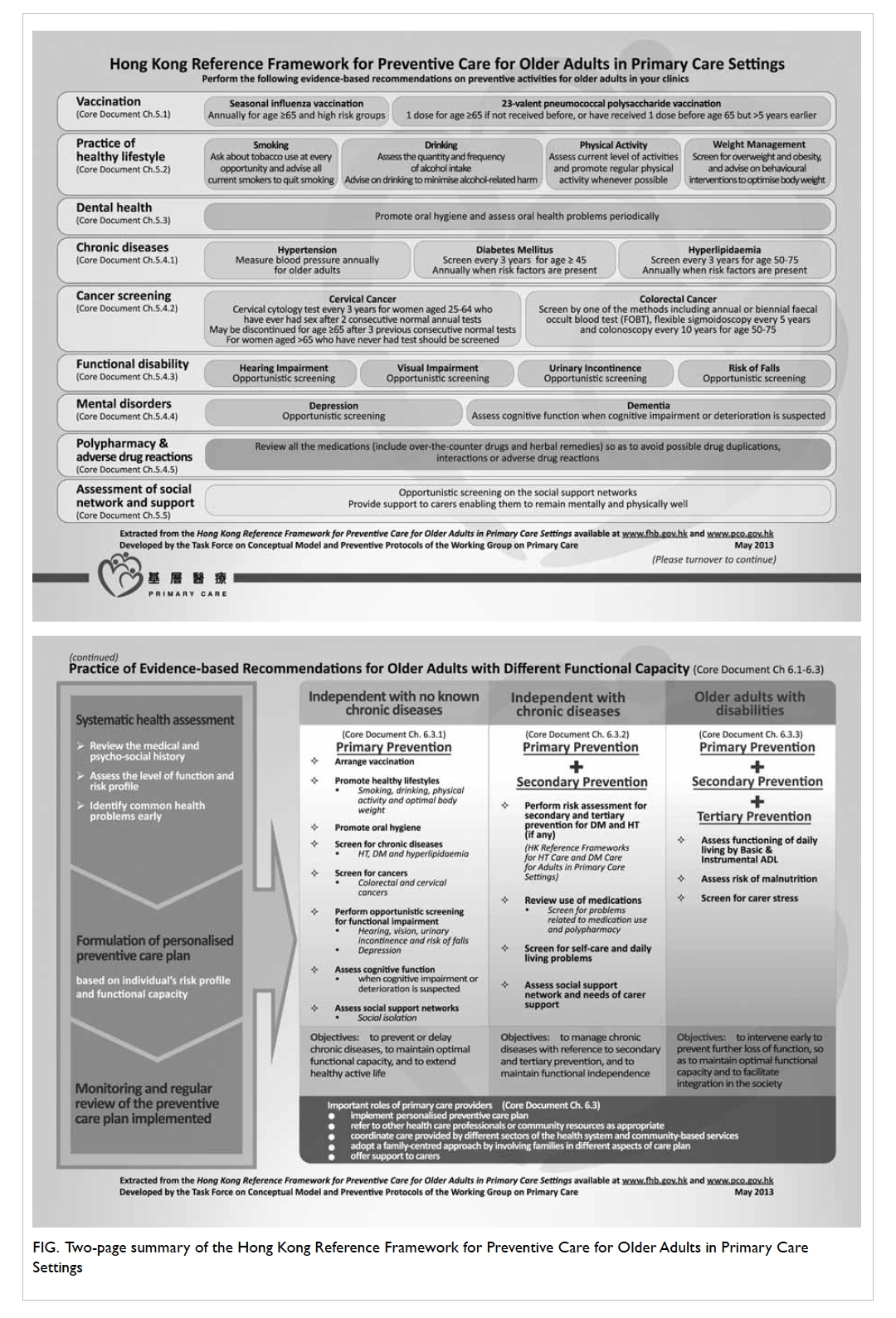
Figure. Two-page summary of the Hong Kong Reference Framework for Preventive Care for Older Adults in Primary Care Settings
Patient education materials
In a busy clinic, patient education material is an
effective means to deliver preventive care information
to patients and their carers. The resources related to
the health care of older adults are available in Annex
3 of the core document.2 These resources provide
information for the local community and help
primary care providers coordinate care with other
professionals and specialists. Families can also be
put in touch with community-based services. With
appropriate care, older adults can achieve optimum
health and improve their quality of life.
Conclusion
Effective preventive care of older adults can be
achieved through health education and promotion,
prevention and monitoring of diseases, and reduction
of functional disabilities. Primary care providers
play an important role in providing patient-centred,
comprehensive, continuing, and coordinated
preventive care to older adults in the community. In
addition, continued efforts of different health care
providers, professional organisations, social service
agencies, and all stakeholders are needed to provide
a supportive environment for active and healthy
ageing. It is hoped that through the development
and promotion of this reference framework, more
emphasis can be placed on preventive care in older
adults. This will improve their health and promote
healthy ageing.
References
1. Hong Kong Population Projections 2012-2041.
Census and Statistics Department, HKSAR. 2012 July. Available from: http://www.statistics.gov.hk/pub/B1120015052012XXXXB0100.pdf. Accessed Jun 2015.
2. Hong Kong Reference Framework for Preventive Care for
Older Adults in Primary Care Settings 2012. Available
from: http://www.pco.gov.hk/english/resource/files/ref_framework_adults.pdf. Accessed 11 Nov 2014.
3. Brotons C, Bulc M, Sammut MR, et al. Attitudes toward
preventive services and lifestyle: the views of primary care
patients in Europe. The EUROPREVIEW patient study.
Fam Pract 2012;29 Suppl 1:i168-76. Crossref
4. Wallace LS, Rogers ES, Roskos SE, Holiday DB, Weiss
BD. Brief report: screening items to identify patients with
limited health literacy skills. J Gen Intern Med 2006;21:874-7. Crossref
5. Lo YY, Lam CL, Mercer SW, et al. Patient morbidity and
management patterns of community-based primary health
care services in Hong Kong. Hong Kong Med J 2011;17(3 Suppl 3):33-7.
6. Canadian Task Force on the Periodic Health Examination.
The Periodic Health Examination 1984. A Report of
the Periodic Health Examination Task Force. Ottawa,
Ontario: Health Services Directorate, Health Services and
Promotion Branch, Department of National Health and
Welfare; 1984: 15.
7. US Preventive Services Task Force. Guide to clinical
preventive services. 2nd ed. Baltimore, MD: Williams &
Wilkins; 1996.
8. Lam CL, Leung GM, Mercer SW, et al. Utilisation patterns
of primary health care services in Hong Kong: does having
a family doctor make any difference? Hong Kong Med J
2011;17(3 Suppl 3):28-32.
9. Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E.
Effectiveness of influenza vaccine in the community-dwelling
elderly. N Engl J Med 2007;357:1373-81. Crossref
10. Moberley SA, Holden J, Tatham DP, Andrews RM.
Vaccines for preventing pneumococcal infection in adults.
Cochrane Database Syst Rev 2008;(1):CD000422. Crossref
11. Ranney L, Melvin C, Lux L, McClain E, Lohr KN. Systematic
review: smoking cessation intervention strategies for
adults and adults in special populations. Ann Intern Med
2006;145:845-56. Crossref
12. Lam TH, Li ZB, Ho SY, et al. Smoking, quitting and
mortality in an elderly cohort of 56,000 Hong Kong
Chinese. Tob Control 2007;16:182-9. Crossref
13. Whitlock EP, Polen MR, Green CA, Orleans T, Klein J;
U.S. Preventive Services Task Force. Behavioral counseling
interventions in primary care to reduce risky/harmful
alcohol use by adults: a summary of the evidence for the
U.S. Preventive Services Task Force. Ann Intern Med
2004;140:557-68. Crossref
14. Elward K, Larson EB. Benefits of exercise for older adults. A
review of existing evidence and current recommendations
for the general population. Clin Geriatr Med 1992;8:35-50.
15. Clinical guidelines on the identification, evaluation, and
treatment of overweight and obesity in adults: the Evidence
Report. NIH Publication No. 98-4083. National Institutes
of Health–National Heart, Lung and Blood Institute–Obesity Education Initiative; 1998.
16. Kressin NR, Boehmer U, Nunn ME, Spiro A 3rd. Increased
preventive practices lead to greater tooth retention. J Dent
Res 2003;82:223-7. Crossref
17. Hong Kong Reference Framework for Hypertension Care
for Adults in Primary Care Settings. Available from: http://www.pco.gov.hk/english/resource/files/RF_HT_full.pdf. Accessed Jun 2015.
18. Blood Pressure Lowering Treatment Trialists’
Collaboration: Turnbull F, Neal B, Ninomiya T, et al. Effects
of different regimens to lower blood pressure on major
cardiovascular events in older and younger adults: meta-analysis
of randomised trials. BMJ 2008;336:1121-3. Crossref
19. Hong Kong Reference Framework for Diabetes Care for
Adults in Primary Care Settings. Available from: http://www.pco.gov.hk/english/resource/files/RF_DM_full.pdf. Accessed Jun 2015.
20. U.S. Preventive Services Task Force. Screening for type
2 diabetes mellitus in adults: U.S. Preventive Services
Task Force recommendation statement. Ann Intern Med
2008;148:846-54. Crossref
21. The Royal Australian College of General Practitioners.
Guidelines for preventive activities in general practice 8th edition. Available from: http://www.racgp.org.au/your-practice/guidelines/redbook/. Accessed 17 Apr 2014.
22. U.S. Preventive Services Task Force. Screening for lipid
disorders in adults: U.S. Preventive Services Task Force
recommendation statement. June 2008. Available from:
http://www.uspreventiveservicestaskforce.org/uspstf08/lipid/lipidrs.htm. Accessed 17 Apr 2014.
23. Sasieni PD, Cuzick J, Lynch-Farmery E. Estimating
the efficacy of screening by auditing smear histories of
women with and without cervical cancer. The National
Co-ordinating Network for Cervical Screening Working
Group. Br J Cancer 1996;73:1001-5. Crossref
24. The Cancer Expert Working Group (CEWG) on Cancer
Prevention and Screening. Recommendations on colorectal cancer screening. Available from: http://www.chp.gov.hk/files/pdf/recommendations_on_crc_screening_2010.pdf. Accessed 17 Apr 2014.
25. Chou R, Dana T, Bougatsos C, Fleming C, Beil T. Screening
adults aged 50 years or older for hearing loss: a review of
the evidence for the U.S. Preventive Services Task Force.
Ann Intern Med 2011;154:347-55. Crossref
26. Chou R, Dana T, Bougatsos C. Screening older adults
for impaired visual acuity: a review of the evidence for
the U.S. Preventive Services Task Force. Ann Intern Med
2009;151:44-58, W11-20.
27. O’Neil B, Gilmour D, Approach to urinary incontinence in
women. Diagnosis and management by family physicians.
Can Fam Physician 2003;49:611-8.
28. Gillespie LD, Robertson MC, Gillespie WJ, et al.
Interventions for preventing falls in older people
living in the community. Cochrane Database Syst Rev
2009:(2):CD007146. Crossref
29. O’Connor EA, Whitlock EP, Beil TL, Gaynes BN. Screening
for depression in adult patients in primary care settings: a
systematic evidence review. Ann Intern Med 2009;151:793-803. Crossref
30. Boustani M, Peterson B, Hanson L, Harris R, Lohr
KN; U.S. Preventive Services Task Force. Screening for
dementia in primary care: a summary of the evidence for
the U.S. Preventive Services Task Force. Ann Intern Med
2003;138:927-37. Crossref
31. Steinman MA, Landefeld CS, Rosenthal GE, Berthenthal
D, Sen S, Kaboli PJ. Polypharmacy and prescribing quality
in older people. J Am Geriatr Soc 2006;54:1516-23. Crossref
32. Lou VW. Caregiving burden: congruence of health
assessment between caregivers and care receivers. Asian J Gerontol Geriatr
2010;5:21-4.
33. Myint PK, Luben RN, Wareham NJ, Bingham SA, Khaw KT.
Combined effect of health behaviours and risk of first ever
stroke in 20,040 men and women over 11 years’ follow-up
in Norfolk cohort of European Prospective Investigation of
Cancer (EPIC Norfolk): prospective population study. BMJ
2009;338:b349. Crossref
34. Myint PK, Smith RD, Luben RN, et al. Lifestyle behaviours
and quality-adjusted life years in middle and older age. Age
Ageing 2011;40:589-95. Crossref
35. Victor CH, Howse K. Effective health promotion with
vulnerable groups: older people. London: Health Education
Authority; 1999.
36. Scott KM, Von Korff M, Alonso J, et al. Mental-physical
co-morbidity and its relationship with disability: results
from the World Mental Health Surveys. Psychol Med
2009;39:33-43. Crossref
37. Lee TA, Shields AE, Vogeli C, et al. Mortality rate in
veterans with multiple chronic conditions. J Gen Intern
Med 2007;22 Suppl 3:403-7. Crossref
38. Vogeli C, Shields AE, Lee TA, et al. Multiple chronic
conditions: prevalence, health consequences, and
implications for quality, care management, and costs. J Gen
Intern Med 2007;22 Suppl 3:391-5. Crossref
39. Wolff JL, Starfield B, Anderson G. Prevalence, expenditures,
and complications of multiple chronic conditions in the
elderly. Arch Intern Med 2002;162:2269-76. Crossref
40. Von Korff M, Ormel J, Katon W, Lin EH. Disability
and depression among high utilizers of health care. A
longitudinal analysis. Arch Gen Psychiatry 1992;49:91-100. Crossref