Hong Kong Med J 2015 Apr;21(2):114–23 | Epub 10 Mar 2015
DOI: 10.12809/hkmj144398
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Surveillance of emerging drugs of abuse in Hong Kong: validation of an analytical tool
Magdalene HY Tang, PhD1;
CK Ching, FRCPA, FHKAM (Pathology)1;
ML Tse, FHKCEM, FHKAM (Emergency Medicine)2;
Carol Ng, BSW, MA3;
Caroline Lee, MSc1;
YK Chong, MB, BS1;
Watson Wong, MSc1;
Tony WL Mak, FRCPath, FHKAM (Pathology)1; Emerging Drugs of Abuse Surveillance Study Group
1 Toxicology Reference Laboratory, Hospital Authority, Hong Kong
2 Hong Kong Poison Information Centre, Hospital Authority, Hong Kong
3 Hong Kong Lutheran Social Service, the Lutheran Church – Hong Kong Synod, Homantin, Hong Kong
Corresponding author: Dr Tony WL Mak (makwl@ha.org.hk)
Abstract
Objective: To validate a locally developed
chromatography-based method to monitor
emerging drugs of abuse whilst performing regular
drug testing in abusers.
Design: Cross-sectional study.
Setting: Eleven regional hospitals, seven social
service units, and a tertiary level clinical toxicology
laboratory in Hong Kong.
Participants: A total of 972 drug abusers and
high-risk individuals were recruited from acute,
rehabilitation, and high-risk settings between 1
November 2011 and 31 July 2013. A subset of the
participants was of South Asian ethnicity. In total,
2000 urine or hair specimens were collected.
Main outcome measures: Proof of concept that
surveillance of emerging drugs of abuse can be
performed whilst conducting routine drug of abuse
testing in patients.
Results: The method was successfully applied
to 2000 samples with three emerging drugs
of abuse detected in five samples: PMMA
(paramethoxymethamphetamine), TFMPP
[1-(3-trifluoromethylphenyl)piperazine], and
methcathinone. The method also detected
conventional drugs of abuse, with codeine,
methadone, heroin, methamphetamine, and
ketamine being the most frequently detected drugs.
Other findings included the observation that South
Asians had significantly higher rates of using opiates
such as heroin, methadone, and codeine; and that
ketamine and cocaine had significantly higher
detection rates in acute subjects compared with the
rehabilitation population.
Conclusions: This locally developed analytical
method is a valid tool for simultaneous surveillance
of emerging drugs of abuse and routine drug
monitoring of patients at minimal additional cost
and effort. Continued, proactive surveillance and
early identification of emerging drugs will facilitate
prompt clinical, social, and legislative management.
New knowledge added by this
study
- A locally developed method is a valid tool for monitoring the penetrance of emerging drugs of abuse into our society whilst performing regular drugs of abuse testing.
- Implementation of the analytical method in the routine drug monitoring of drug abusers will enable simultaneous surveillance of novel drugs of abuse at minimal extra cost and effort.
- Continued and proactive surveillance of emerging drugs of abuse in the population will facilitate prompt measures in the clinical, social, and legislative management of these constantly changing and potentially dangerous drugs.
Introduction
Despite continuous efforts, drug abuse remains a
major social and medical problem in today’s society.
In particular, there has been a rapid and continued
growth of ‘emerging’ drugs of abuse (DOA) on a global
scale.1 2 Emerging DOA, also called designer drugs or novel psychoactive substances, bear a chemical and/or pharmacological resemblance to conventional
DOA and pose a threat to public health, but are
often (initially) not controlled by law. They are easily
accessible from street dealers or through the internet,
and are often presumed to be safer than conventional
DOA owing to their ‘legal’ or ‘herbal’ nature.1 3 In
Hong Kong, the drug scene has also been penetrated
in recent years by such substances as the piperazine
derivative TFMPP [1-(3-trifluoromethylphenyl)piperazine],4 the synthetic cannabinoids,5 the methamphetamine derivative PMMA (paramethoxymethamphetamine),6 and the NBOMe (N-methoxybenzyl derivatives of phenethylamine).7
Some of these novel drugs pose a significant health
threat and numerous fatalities have been reported
worldwide.8 9 10 In particular, PMMA and the NBOMe
drugs have been associated with severe clinical
toxicity and fatalities in Hong Kong.6 7
Effective diagnosis and treatment of emerging
DOA intoxication rely on the timely and accurate
detection of these substances. Whilst immunoassay
and drug screening methods are well-established
for conventional DOA, laboratory analysis of novel
drugs is not so readily available. This inevitably leads
to the delayed discovery of emerging drugs and
consequently early medical and social intervention is
compromised. Recently, a liquid chromatography–tandem mass spectrometry (LC-MS/MS)–based
method has been established locally that allows the
simultaneous detection of 47 commonly abused
drugs in addition to over 45 emerging DOA and their
metabolites in urine11 and hair (the latter manuscript
in preparation). The aim of the current study was to
validate this analytical method as a tool to monitor
emerging DOA whilst performing regular DOA
testing by applying the method to 2000 urine and
hair specimens collected from drug abusers as well
as high-risk individuals.
Methods
Sample collection
Between 1 November 2011 and 31 July 2013, 964
urine and 1036 hair specimens (n=2000 in total) were
collected for analysis. Subjects who were included in
the study were patients/clients of the units listed, and
who were suspected to be actively using DOA and
who agreed to participate in the study: (i) substance
abuse clinics within the Hospital Authority (Castle
Peak Hospital, Kowloon Hospital, Kwai Chung
Hospital, Pamela Youde Nethersole Eastern Hospital,
Prince of Wales Hospital, Queen Mary Hospital); (ii)
accident and emergency (A&E) departments within
the Hospital Authority (Pamela Youde Nethersole
Eastern Hospital, Pok Oi Hospital, Princess Margaret
Hospital, Queen Mary Hospital, Tuen Mun Hospital,
United Christian Hospital, Yan Chai Hospital); (iii)
the Hong Kong Poison Information Centre (HKPIC)
toxicology clinic; (iv) counselling centres for
psychotropic substance abusers (CCPSA; Evergreen
Lutheran Centre, Rainbow Lutheran Centre, Cheer
Lutheran Centre); (v) various rehabilitation centres
including the Society of Rehabilitation and Crime
Prevention (SRACP), Operation Dawn and Caritas Wong Yiu Nam Centre; and (vi) Youth Outreach.
Pregnant women and individuals aged under 18 years
were excluded from the study. The majority of the
participants were Chinese, although those recruited
from SRACP were exclusively South Asians.
The study was approved by the institutional
ethics review boards (Kowloon West Cluster: KW/FR-11-011 (41-05); Kowloon Central/Kowloon East
Cluster: KC/KE-11-0170/ER-2; Hong Kong West Cluster: UW 11-398; Hong Kong East Cluster: HKEC-2011-068; New Territories West Cluster: NTWC/CREC/989/11; New Territories East Cluster: CRE-2011.427). Subjects donated samples on a voluntary basis and informed consent was obtained. Each
subject donated either urine or hair, or both, at each
donation episode. Some gave repeated sample(s):
donations were at least 8 weeks apart. Urine was
collected in a plain plastic bottle and frozen until
analysis. For hair, a lock of hair was collected from
the back of the head for analysis. The root end was
identified to facilitate segmental analysis.
Sample analysis
The methodology for urine analysis has been detailed
in a separate publication.11 In brief, the urine sample
was subjected to an initial glucuronidase digestion,
followed by solid phase extraction and sample
concentration. The hair sample (first 3-cm segment)
was first decontaminated and subsequently
subjected to simultaneous micro-pulverisation
and extraction in solvent. The final filtrates were
analysed by LC-MS/MS performed on an Agilent
6430 triple-quadrupole mass spectrometer (Agilent
Technologies, Singapore) coupled with Agilent
1290 Infinity liquid chromatography system. The
47 conventional and 47 emerging DOA identified
for analysis are listed in Table 1. The analytical
method had previously been validated according to
international guidelines.12
Statistical analysis
Statistical analysis was performed using Fisher’s
exact test, with a P value of less than 0.05 considered
statistically significant. Comparison of the drug
detection rates was made between (i) different ethnic
groups and (ii) samples collected in the rehabilitation
and acute settings.
Results
Subject demographics
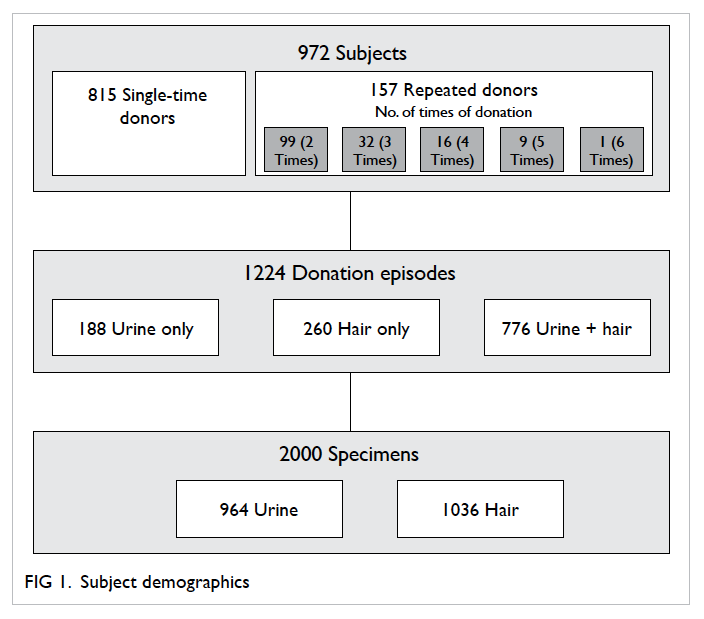
In total, 972 individuals took part in the study (720
males, 252 females). Their respective mean and median age was 35 and 33 years (range,
18-74 years). Of the 972 subjects, 815 were single-time
donors and 157 donated repeated samples
(between 2 and 6 donations each). There were 1224
donation episodes (815 from single-time donors; 409
from repeated donors) and 2000 specimens collected
in total, of which 964 were urine and 1036 were hair
(Fig 1). Of the 1224 donation episodes, the subjects
were recruited from: substance abuse clinics (n=822),
drug rehabilitation and counselling centres (n=320),
youth hangout centre (n=41), HKPIC toxicology
clinic (n=28), and A&E departments (n=13).
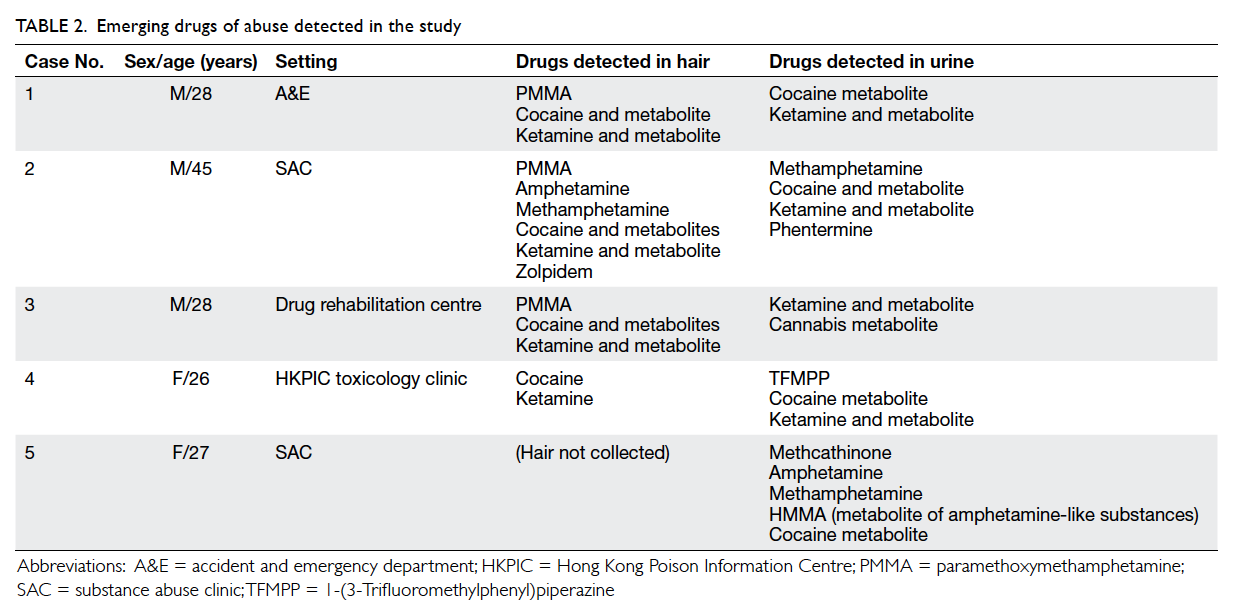
Emerging drugs of abuse
In the 2000 specimens analysed, five specimens were
found to contain three emerging DOAs: PMMA,
TFMPP, and methcathinone. A methamphetamine
derivative, PMMA, was detected in three hair
specimens (cases 1-3, Table 2). All three hair samples
were also found to contain cocaine and ketamine.
Nonetheless, PMMA was not detected in the
subjects’ concurrent urine sample.
A piperazine derivative, TFMPP, was detected
in one urine specimen (case 4, Table 2), together with
cocaine and ketamine. Nonetheless TFMPP was not
detected in the parallel hair sample.
Methcathinone, also known as ephedrone, is
a cathinone (beta-keto amphetamine) analogue. It
was detected in combination with amphetamine,
methamphetamine, and cocaine metabolite in one
urine specimen (case 5, Table 2). No parallel hair
specimen was available from this subject.
Conventional drugs of abuse
Analysis of the 964 urine samples revealed the
presence of 19 types of conventional DOA (Fig 2a).
Codeine was the most common, being detected in
47% of the urine samples, followed by methadone
(35%), heroin (22%), methamphetamine (21%),
ketamine (20%), zopiclone (20%), amphetamine
(17%), midazolam (17%), and dextromethorphan
(14%). Cocaine and cannabis were detected in 6%
and 3% of urine samples, respectively.
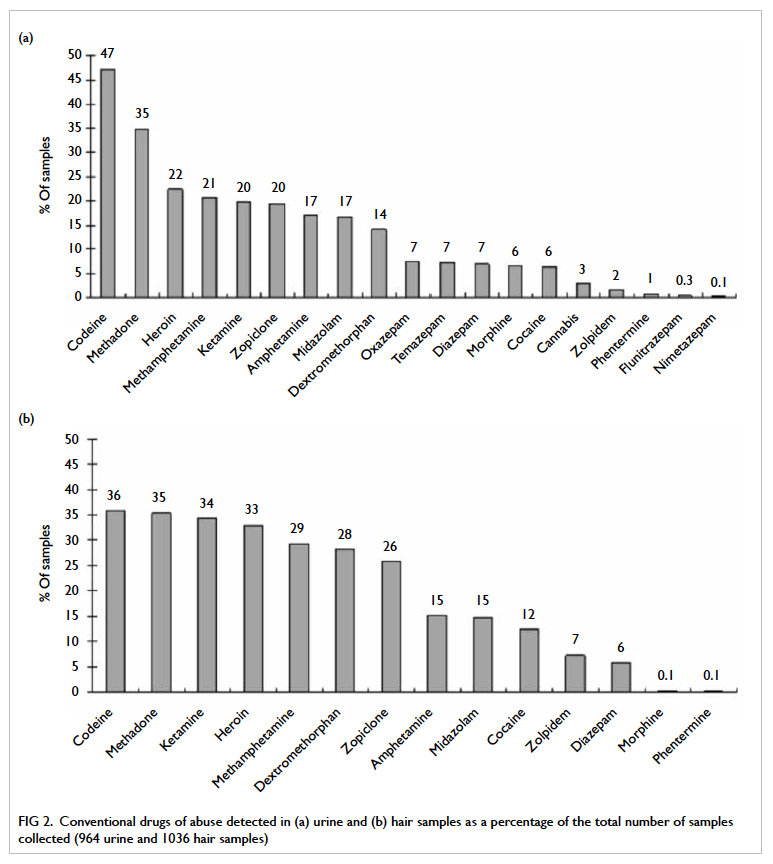
Figure 2. Conventional drugs of abuse detected in (a) urine and (b) hair samples as a percentage of the total number of samples collected (964 urine and 1036 hair samples)
In hair specimens (1036 in total), 14 types
of conventional DOA were detected (Fig 2b).
Codeine (36%) and methadone (35%) were the most
prevalent, followed by ketamine (34%), heroin (33%),
methamphetamine (29%), dextromethorphan (28%),
and zopiclone (26%). Cocaine and zolpidem were
detected in 12% and 7% of the samples, respectively.
Ethnic minority
A subset of participants (n=130) were of South Asian
ethnicity. These subjects donated 248 specimens in
130 episodes. Their drug use pattern was significantly
different to that of Chinese. Comparison of
urinalysis results revealed that South Asians had a
significantly higher proportion of opiate use such as
heroin, methadone, and codeine (P<0.001) as well as
dextromethorphan (P<0.05; Fig 3a). On the contrary,
ketamine, zopiclone, and diazepam (P<0.001) as well
as cocaine and amphetamine (P<0.05) were detected
at significantly higher rates in Chinese compared
with South Asians. Analysis of hair specimens
showed a largely similar pattern of discrepancy
between the two ethnicities (Fig 3b).
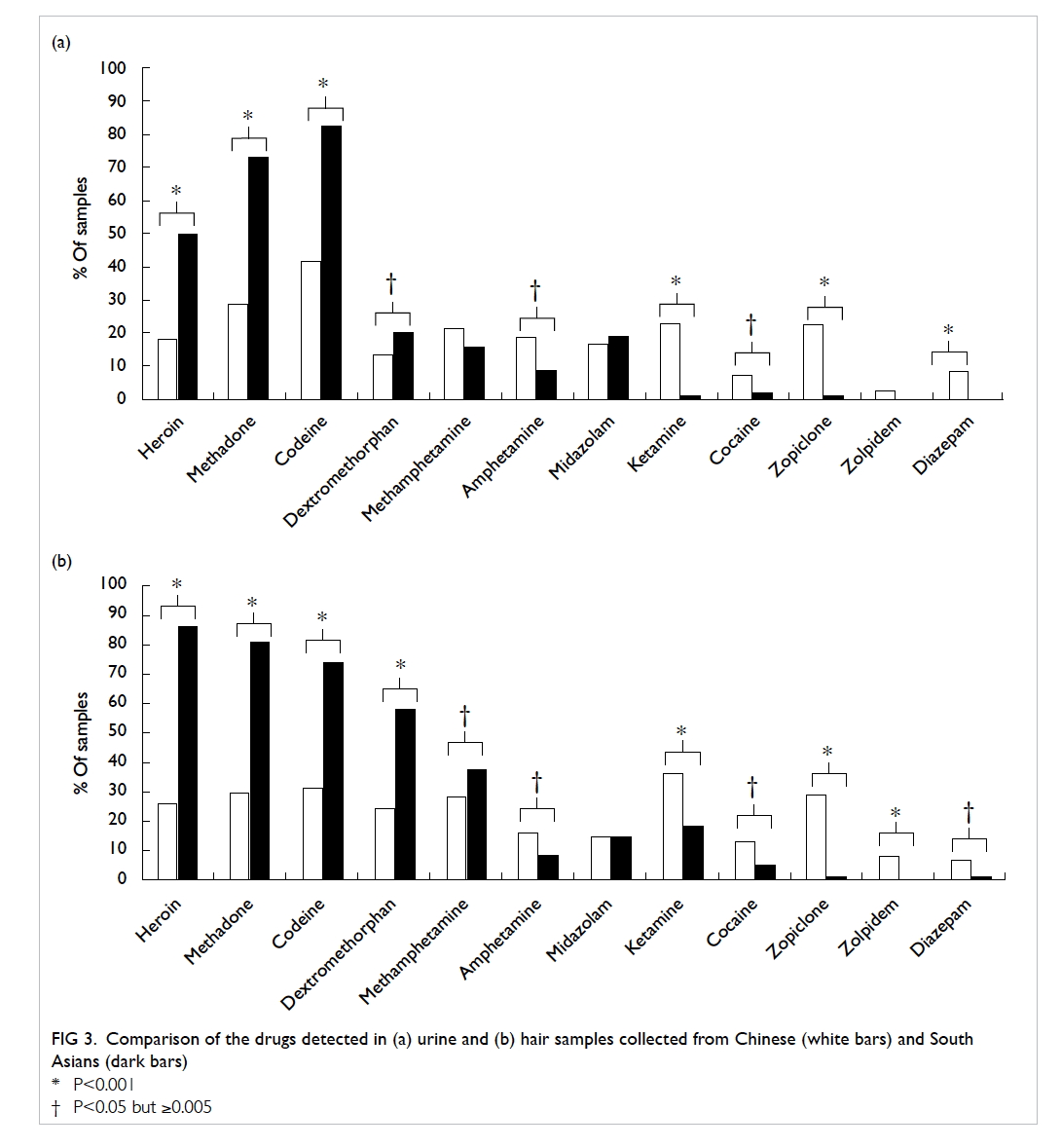
Figure 3. Comparison of the drugs detected in (a) urine and (b) hair samples collected from Chinese (white bars) and South Asians (dark bars)
Collection site setting
The urine samples in the current study were collected
from different settings: 38 samples from acute setting
(A&E departments and HKPIC toxicology clinic); 885
samples from drug rehabilitation setting (substance
abuse clinics, CCPSA and other rehabilitation
centres); and 41 from a high-risk population (youth
hangout). A comparison of drugs detected between
the acute and rehabilitation settings revealed a
significantly higher detection rate of ketamine
and cocaine (P<0.001) in the former (Fig 4). Drugs
such as codeine, methadone, heroin, zopiclone, and
dextromethorphan were detected at higher rates in
samples collected in a rehabilitation setting.
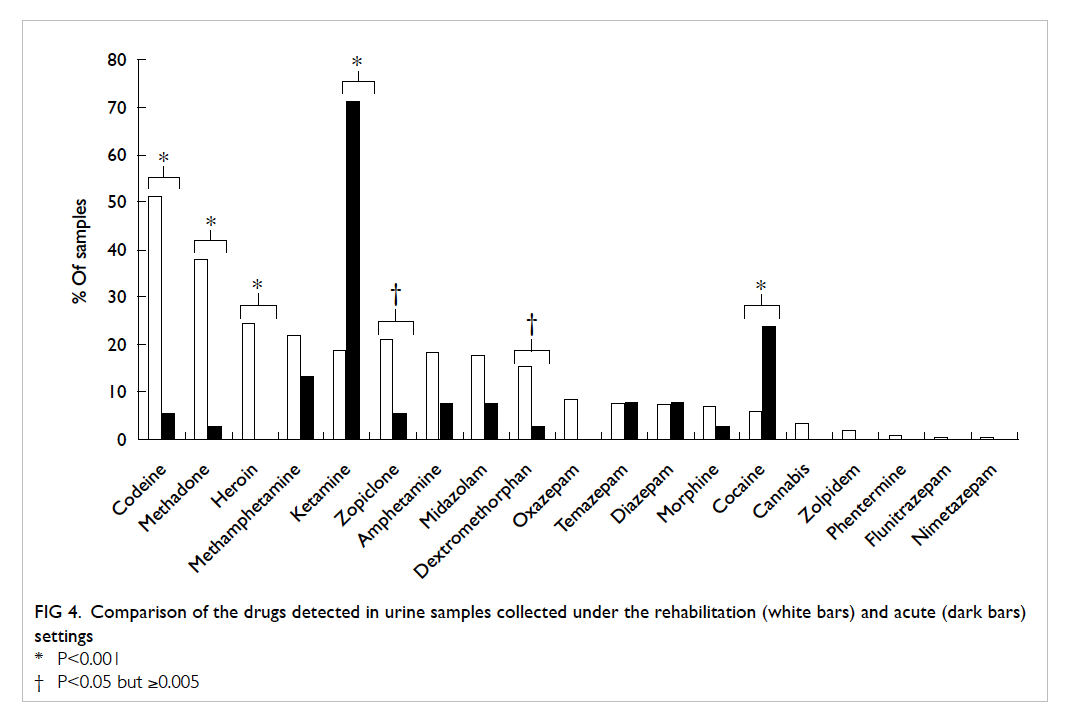
Figure 4. Comparison of the drugs detected in urine samples collected under the rehabilitation (white bars) and acute (dark bars) settings
Discussion
Emerging DOA are constantly being monitored
worldwide by agencies such as the European
Monitoring Centre for Drugs and Drug Addiction
(EMCDDA). In 2008, 13 emerging DOA were
reported for the first time to EMCDDA; by 2012,
73 new drugs had been reported within a year.1
Recent years have also seen the emergence of such
designer drugs in Hong Kong, some of which have
caused severe morbidity and fatalities.4 5 7 The early
identification of emerging drugs enables prompt
counteractive measures in terms of their clinical
and social management, and the surveillance of
emerging drugs in the population is increasingly
being adopted globally as a proactive approach to
combat drug abuse.13 14 15 In view of this, the present
study was conducted to validate a locally developed
LC-MS/MS method to screen for emerging DOA
in the local population whilst simultaneously
monitoring routine DOA. The study was conducted
over a 21-month period. Multiple clinical and social
service units from across the city collaborated in
the study for a wider geographical coverage and
more representative results. In 2013, approximately
10 069 drug abusers were reported in Hong Kong.16
This study population (972 subjects) was estimated
to represent 9.7% of the total potential subjects.
Regarding the response or participation rate, due to
practical concerns and limited manpower, it was not
possible for every collaborating unit to document
fully the number of subjects approached or the
number who refused consent.
The current results revealed the presence
of three emerging drugs (PMMA, TFMPP, and
methcathinone) in five specimens. This low
prevalence is an expected finding due to the intrinsic
nature of ‘emerging’ rather than ‘established’
drugs. Nevertheless, PMMA is a highly toxic
methamphetamine derivative that has been sold on
the drug market as MDMA (3,4-methylenedioxy-methamphetamine) substitute.8 The drug has been reported to have caused up to 90 fatalities
worldwide over the years, including eight fatalities in
Taiwan.8 17 In particular, PMMA-associated fatalities have also been reported recently in Hong Kong.6
On the other hand, TFMPP is a piperazine
derivative with mild hallucinogenic effects and,
when taken with another piperazine derivative
benzylpiperazine (BZP), causes ecstasy-like
effects.18 Piperazine derivatives are known to cause
dissociative and sympathomimetic toxicity.19 The
drug TFMPP was first reported in Hong Kong in
20104 and has been identified as an emerging drug in
Ireland in recent years.15
Another emerging DOA detected in the
study, methcathinone, gained popularity from the
1970s to 1990s, and was recently reported as a ‘re-emerging’
DOA in Sweden.14 It is an amphetamine-like
stimulant and is among a group of synthetic
cathinone compounds, commonly known as “bath
salts”, that have been associated with numerous
fatalities worldwide.20 Other highly toxic cathinone
derivatives include mephedrone and MDPV (methylenedioxypyrovalerone),9 10 both of which are also covered in the analytical method
but were not detected in the current study.
Of the conventional DOA, the opiates,
methamphetamine, and ketamine were among
the most frequently detected in this study. This is
consistent with the data on reported drug abusers that
was published by the local Central Registry of Drug
Abuse.21 Since this manuscript focuses on screening
for emerging DOA, detailed analysis of conventional
drug use such as gender and age differences was not
performed. However, an interesting finding was the
observation that significantly higher proportions of
South Asian drug abusers used opiates such as heroin,
methadone, and codeine compared with Chinese;
Chinese drug abusers were much more likely to
use ketamine, cocaine, zopiclone, and diazepam.
This highlights the ethnic differences in drug use
and indicates that alternative approaches may be
required for the clinical and social management of
ethnic minorities in Hong Kong.
It is of interest to note the particularly high
percentage of ketamine and cocaine detected in
urine samples collected at A&E departments and
toxicology clinic compared with the other collection
sites. This may indicate that these drugs carry a more
acute and severe toxicity profile relative to the other
drugs with a consequent need of hospitalisation.
A previous study on drug driving in Hong Kong
also reported ketamine as the most prevalent drug
detected in driver casualties who presented to the
A&E department.22 Comparison of hair analysis
results was not made here, since the main focus
was on the difference between acute and non-acute
cases; hair specimens would be less helpful since this
biological matrix does not reflect recent exposure to
drugs (see below for further discussion).
The present study showed a broadly similar
pattern in urine and hair matrices in terms
of the conventional DOA detected. Cocaine,
dextromethorphan, and zolpidem were detected at
higher rates in hair compared with urine, and may
indicate the relatively high deposition efficiency
of these drugs in hair matrix. It should be noted,
however, that the metabolites of zolpidem were not
included in the current assay, and may decrease its
sensitivity for detection in urine. Urine and hair
specimens have different ‘detection windows’, that
is, they reflect different time frames of drug intake.
Detection in urine indicates recent intake (within
hours/days); thus this matrix is useful for the
management of acute toxicity and drug overdose.
The detection window of hair is much longer
(weeks/months), enabling this matrix to be used for
monitoring long-term drug use or abstinence.
When interpreting the results of the current
study, it should be noted that some drugs may
have been taken for therapeutic reasons, for
example codeine, methadone, phentermine, or the
tranquilizers/benzodiazepines. It was not possible in
this study to differentiate medical use from abuse. It
should also be noted that some drugs may be present
as metabolites of others, for example temazepam and
oxazepam (both of which are diazepam metabolites)
and the emerging drug mCPP (metabolite of the
antidepressant trazodone). Morphine is also the
metabolite of codeine and heroin; it was only
reported here as a drug in the absence of either
codeine or heroin in the same sample.
Effective control of novel drugs depends on
their early identification. A number of means to
monitor emerging DOA have been proposed, such
as conducting population surveys, analysing online
test purchases, or wastewater analysis.3 Population
surveys suffer the potential drawback of obtaining
inaccurate data, since the actual identity of the drugs
may differ from the claimed ingredients, for example,
BZP being sold as ‘MDMA’ tablets.23 Analysing
drug items purchased online is a costly approach
due to the vast number of products available.
Wastewater analysis may be used for monitoring
conventional DOA, but the approach may not be
easily adapted to the surveillance of emerging drugs
due to the anticipated minute levels (ng/L range)
in wastewater.24 All the above approaches require
a considerable amount of financial and manpower
resources. We propose the integration of emerging
DOA surveillance into the routine drug monitoring
of patients using the established analytical method.
This surveillance approach is accurate, readily
attainable, and is also achieved with minimal extra
cost and effort since it is a convenient by-product of
the routine drug monitoring of patients. Additionally,
its applicability in A&E department patients allows
the early identification of highly toxic novel drugs.
The proposed analytical method is LC-MS/MS–based, and offers several advantages over traditional DOA testing by immunoassay methods.
First, development of an immunoassay is a lengthy
process (in terms of years) involving the generation
of antibodies. Immunoassay analysis also depends
solely on the availability of commercial kits. These
features do not favour early detection of new
compounds given the protean nature of emerging
drugs. In contrast, LC-MS/MS–based methods
are much more versatile, permitting in-house
enhancement of the method to allow detection of
new compounds as soon as they enter the market.
Second, although immunoassay methods require
minimal capital investment, their running costs are
high due to the generation of antibodies. On the
other hand, LC-MS/MS methods require a high
initial investment in analysers, but the running cost
is lower in the long term as the reagents involved are
relatively inexpensive. Lastly, unlike immunoassay
methods that are only preliminary in nature
and require further confirmatory testing, mass
spectrometry analysis is already confirmatory with
accurate and definitive results.
In addition to laboratory analysis, the emerging
DOA surveillance team requires the expertise of
medical doctors to keep a close watch on emerging
drugs on the market, especially those with high
clinical toxicity. Based on this ‘toxico-intelligence’,
scientists should then enhance the analytical method
to include such emerging substances. Hence, the
effective control of emerging drugs will require
a team of trained medical doctors and scientists,
as well as versatile technology that enables the
continual expansion of analytical coverage. In view
of the resource requirements, specialised toxicology
centres may be better suited for the purpose.
The present study has proven the concept that
a locally developed analytical method is a valid tool
to monitor emerging DOA whilst simultaneously
performing regular DOA testing in patients.
Implementation of the method in the routine drug
monitoring of abusers will enable the continued
and proactive surveillance of novel drugs in the
population with minimal extra cost and effort. This
surveillance gathers important information so that
society can be prepared in terms of legislation, as well as
social and clinical management of these potentially
dangerous drugs. Further expansion of the analytical
coverage will help keep abreast of the rapid and
constant change in the designer drug scene.
Acknowledgements
This study was financially supported by the Beat
Drugs Fund (Narcotics Division, Security Bureau
of the HKSAR Government), project reference
BDF101021. The authors are also grateful to all
participants and for the generous assistance received
from participating clinical divisions within the
Hospital Authority and social service units.
Declaration
No conflicts of interests were declared by authors.
Appendix
Members of the Emerging Drugs of Abuse Surveillance Study Group:
YH Lam, MPhil1;
WH Cheung, FHKCPsych, FHKAM (Psychiatry)2;
Eva Dunn, FHKCPsych, FHKAM (Psychiatry)3;
CK Wong, FHKCPsych, FHKAM (Psychiatry)3;
YC Lo, MSc, FIBMS4;
M Lam, FHKCPsych, FHKAM (Psychiatry)5;
Michael Lee, MSc6;
Angus Lau, MSW7;
Albert KK Chung, FHKCPsych, FHKAM (Psychiatry)8;
Sidney Tam, FHKCPath, FHKAM (Pathology)9;
Ted Tam, BSW10;
Vincent Lam, BA(Hon)11;
Hezon Tang, MSW12;
Katy Wan, BSocSc, MA13;
Mamre Lilian Yeh, BA, MSc14;
MT Wong, FHKCPsych, FHKAM (Psychiatry)15;
CC Shek, FHKCPath, FHKAM (Pathology)16;
WK Tang, MD, FHKAM (Psychiatry)17;
Michael Chan, FRCPA, FHKAM (Pathology)18;
Jeffrey Fung, FRCSEd, FHKAM (Emergency Medicine)19;
SH Tsui, FRCP (Edin), FHKAM (Emergency Medicine)20;
Albert Lit, FCEM, FHKAM (Emergency Medicine)21;
Joe Leung, FHKCEM, FHKAM (Emergency Medicine)22
1 Toxicology Reference Laboratory, Hospital
Authority, Hong Kong
2 Substance Abuse Assessment Unit, Kwai Chung
Hospital, Hong Kong
3 Department of Psychiatry, Pamela Youde
Nethersole Eastern Hospital, Hong Kong
4 Department of Pathology, Pamela Youde
Nethersole Eastern Hospital, Hong Kong
5 Department of General Adult Psychiatry, Castle
Peak Hospital, Hong Kong
6 Department of Clinical Pathology, Tuen Mun
Hospital, Hong Kong
7 The Society of Rehabilitation and Crime
Prevention, Hong Kong
8 Department of Psychiatry, Queen Mary Hospital,
Hong Kong
9 Department of Pathology and Clinical
Biochemistry, Queen Mary Hospital, Hong Kong
10 Youth Outreach, Hong Kong
11 Evergreen Lutheran Centre, Hong Kong Lutheran
Social Service, the Lutheran Church — Hong Kong Synod
12 Cheer Lutheran Centre, Hong Kong Lutheran
Social Service, the Lutheran Church — Hong Kong Synod
13 Rainbow Lutheran Centre, Hong Kong Lutheran
Social Service, the Lutheran Church — Hong Kong
Synod
14 Operation Dawn Ltd (Gospel Drug Rehab Centre),
Hong Kong
15 Department of Psychiatry, Kowloon Hospital,
Hong Kong
16 Department of Pathology, Queen Elizabeth
Hospital, Hong Kong
17 Department of Psychiatry, the Chinese University
of Hong Kong, Hong Kong
18 Department of Chemical Pathology, Prince of
Wales Hospital, Hong Kong
19 Accident and Emergency Department, Tuen Mun
Hospital, Hong Kong
20 Accident and Emergency Department, Queen
Mary Hospital, Hong Kong
21 Accident and Emergency Department, Princess
Margaret Hospital, Hong Kong
22 Accident and Emergency Department, Pamela
Youde Nethersole Eastern Hospital, Hong Kong
References
1. European Monitoring Centre for Drugs and Drug
Addiction (EMCDDA), Europol. New drugs in Europe,
2012. EMCDDA-Europol 2012 Annual Report on the
implementation of Council Decision 2005/387/JHA; 2012.
2. Nelson ME, Bryant SM, Aks SE. Emerging drugs of abuse.
Emerg Med Clin North Am 2014;32:1-28. Crossref
3. Brandt SD, King LA, Evans-Brown M. The new drug
phenomenon. Drug Test Anal 2014;6:587-97. Crossref
4. Poon WT, Lai CF, Lui MC, Chan AY, Mak TW. Piperazines:
a new class of drug of abuse has landed in Hong Kong.
Hong Kong Med J 2010;16:76-7.
5. Tung CK, Chiang TP, Lam M. Acute mental disturbance
caused by synthetic cannabinoid: a potential emerging
substance of abuse in Hong Kong. East Asian Arch
Psychiatry 2012;22:31-3.
6. The first mortality case of PMMA in Hong Kong. 本港首次發現服用毒品PMMA後死亡個案. RTHK. 2014 Feb 4. http://m.rthk.hk/news/20140204/982353.htm.
7. Tang MH, Ching CK, Tsui MS, Chu FK, Mak TW. Two
cases of severe intoxication associated with analytically
confirmed use of the novel psychoactive substances
25B-NBOMe and 25C-NBOMe. Clin Toxicol (Phila)
2014;52:561-5. Crossref
8. Lin DL, Liu HC, Yin HL. Recent paramethoxymethamphetamine
(PMMA) deaths in Taiwan. J Anal
Toxicol 2007;31:109-13. Crossref
9. Maskell PD, De Paoli G, Seneviratne C, Pounder DJ.
Mephedrone (4-methylmethcathinone)-related deaths. J
Anal Toxicol 2011;35:188-91. Crossref
10. Durham M. Ivory wave: the next mephedrone? Emerg Med
J 2011;28:1059-60. Crossref
11. Tang MH, Ching CK, Lee CY, Lam YH, Mak TW.
Simultaneous detection of 93 conventional and emerging
drugs of abuse and their metabolites in urine by UHPLC-MS/MS. J Chromatogr B Analyt Technol Biomed Life Sci
2014;969:272-84. Crossref
12. The fitness for purpose of analytical methods: A
laboratory guide to method validation and related topics.
EURACHEM Working Group; 1998.
13. Archer JR, Dargan PI, Hudson S, Wood DM. Analysis of
anonymous pooled urine from portable urinals in central
London confirms the significant use of novel psychoactive
substances. QJM 2013;106:147-52. Crossref
14. Helander A, Beck O, Hägerkvist R, Hultén P. Identification of novel psychoactive drug use in Sweden based on
laboratory analysis—initial experiences from the STRIDA
project. Scand J Clin Lab Invest 2013;73:400-6. Crossref
15. O’Byrne PM, Kavanagh PV, McNamara SM, Stokes SM.
Screening of stimulants including designer drugs in urine
using a liquid chromatography tandem mass spectrometry
system. J Anal Toxicol 2013;37:64-73. Crossref
16. Newly/previously reported drug abusers by sex. Central
Registry of Drug Abuse. Available from: http://www.nd.gov.hk/statistics_list/doc/en/t11.pdf. Accessed 3 Feb 2015.
17. European Monitoring Centre for Drugs and Drug
Addiction (EMCDDA). EMCDDA risk assessments:
Report on the risk assessment of PMMA in the framework
of the joint action on new synthetic drugs; 2003.
18. Arbo MD, Bastos ML, Carmo HF. Piperazine compounds
as drugs of abuse. Drug Alcohol Depend 2012;122:174-85. Crossref
19. Wood DM, Button J, Lidder S, Ramsey J, Holt DW, Dargan
PI. Dissociative and sympathomimetic toxicity associated
with recreational use of 1-(3-trifluoromethylphenyl)
piperazine (TFMPP) and 1-benzylpiperzine (BZP). J Med
Toxicol 2008;4:254-7. Crossref
20. Zawilska JB, Wojcieszak J. Designer cathinones—an
emerging class of novel recreational drugs. Forensic Sci Int
2013;231:42-53. Crossref
21. Reported drug abusers by sex by common type of drugs
abused. Central Registry of Drug Abuse. Available from:
http://www.nd.gov.hk/statistics_list/doc/en/t15.pdf. Accessed 11 Jul 2014.
22. Wong OF, Tsui KL, Lam TS, et al. Prevalence of drugged
drivers among non-fatal driver casualties presenting
to a trauma centre in Hong Kong. Hong Kong Med J
2010;16:246-51.
23. Wood DM, Dargan PI, Button J, et al. Collapse, reported
seizure—and an unexpected pill. Lancet 2007;369:1490. Crossref
24. van Nuijs AL, Gheorghe A, Jorens PG, Maudens K, Neels
H, Covaci A. Optimization, validation, and the application
of liquid chromatography-tandem mass spectrometry for
the analysis of new drugs of abuse in wastewater. Drug Test
Anal 2014;6:861-7. Crossref