DOI: 10.12809/hkmj144259
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Magnetic resonance imaging features of vascular leiomyoma of the ankle
Alta YT Lai, MB, BS, FRCR1;
CW Tam, FRCR, FHKAM (Radiology)1;
John SF Shum, FRCR, FHKAM (Radiology)2;
Jennifer LS Khoo, FRCR, FHKAM (Radiology)1;
WL Tang, FHKCPath, FHKAM (Pathology)3
1 Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
2 Radiology Department, Hong Kong Baptist Hospital, Kowloon Tong, Hong Kong
3 Department of Clinical Pathology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
Corresponding author: Dr Alta YT Lai (altalai@gmail.com)
Abstract
Vascular leiomyoma is a benign soft tissue tumour
with a predilection for middle-aged women. It is
most often seen in the extremities, particularly in the
lower leg. The typical lesion is a small, slow-growing
subcutaneous nodule. These tumours are often
unexpected or preoperatively confused with other
soft tissue tumours including low-grade sarcomas,
leading to wide surgical excision. This may partly
be due to the relatively few studies delineating the
characteristic imaging features of this entity. Here,
the imaging findings of a case of vascular leiomyoma
in the ankle are presented. Literature review of the
magnetic resonance imaging findings of published
reports and series of vascular leiomyomas of the
extremities is also performed.
Case report
A 47-year-old previously healthy Hong Kong
Chinese man presented in January 2012 with a
2-year history of a slow-growing painless mass over
the right medial malleolus. Physical examination
showed a soft, well-marginated, non-tender mass
measuring 2 cm in diameter over the right medial
malleolus. The patient was referred for ultrasound
and subsequently magnetic resonance imaging (MRI;
Figs a to i). The lesion was excised. Macroscopically,
it was a disc-shaped mass with smooth outer surface.
Cut section showed a mass with a thin capsule and
homogeneous, greyish-to-whitish material without
necrosis. Microscopy showed proliferation of
smooth muscle cells associated with thick-walled
blood vessels without evidence of malignancy. The
histopathological diagnosis was vascular leiomyoma
(Figs j and k).
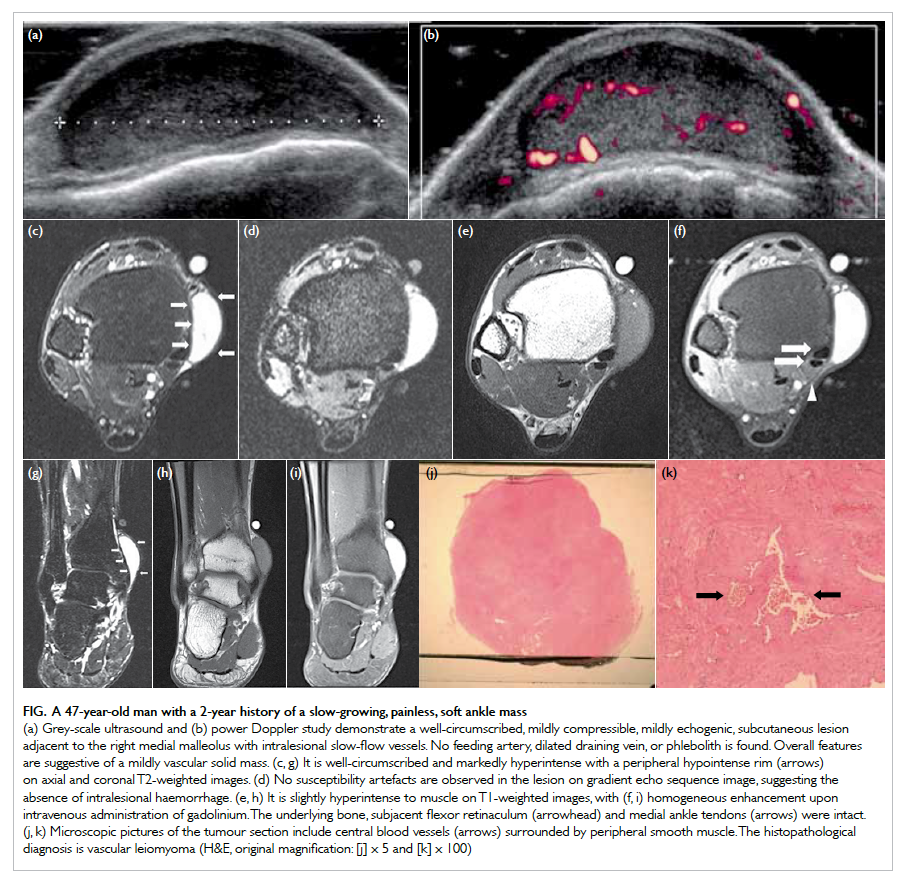
Figure. A 47-year-old man with a 2-year history of a slow-growing, painless, soft ankle mass
(a) Grey-scale ultrasound and (b) power Doppler study demonstrate a well-circumscribed, mildly compressible, mildly echogenic, subcutaneous lesion adjacent to the right medial malleolus with intralesional slow-flow vessels. No feeding artery, dilated draining vein, or phlebolith is found. Overall features are suggestive of a mildly vascular solid mass. (c, g) It is well-circumscribed and markedly hyperintense with a peripheral hypointense rim (arrows) on axial and coronal T2-weighted images. (d) No susceptibility artefacts are observed in the lesion on gradient echo sequence image, suggesting the absence of intralesional haemorrhage. (e, h) It is slightly hyperintense to muscle on T1-weighted images, with (f, i) homogeneous enhancement upon intravenous administration of gadolinium. The underlying bone, subjacent flexor retinaculum (arrowhead) and medial ankle tendons (arrows) were intact. (j, k) Microscopic pictures of the tumour section include central blood vessels (arrows) surrounded by peripheral smooth muscle. The histopathological diagnosis is vascular leiomyoma (H&E, original magnification: [j] x 5 and [k] x 100)
Discussion
Vascular leiomyoma, angiomyoma or
angioleiomyoma, is a rare benign smooth muscle
tumour that originates in the tunica media of
veins and arteries. It can be located in the skin,
subcutaneous fat, or superficial fasciae of the
extremities. It has a predilection for middle-aged
women. It can occur anywhere in the body, but is
most often seen in the extremities, particularly in
the lower leg.1
The most frequent clinical presentation is a
mass that enlarges slowly over several years. The
size usually ranges from subcentimetre to a few
centimetres in diameter, but occasionally may grow
larger. They are usually oval or round in shape, and
can be located in the skin, subcutaneous fat, or the
superficial fasciae of the extremities.
Pain, with or without tenderness, has been
reported in about 60% of patients, and is thought
to be caused by the active contraction of smooth
muscles resulting in local ischaemia, and is also
suggested to be mediated by intratumoural nerve
fibres.2 Treatment usually consists of marginal
excision.2
Angioleiomyomas are rarely diagnosed
preoperatively. In a series of 10 cases by Gupte et
al1 in 2008, the preoperative or pre-biopsy imaging
diagnoses included sarcoma not otherwise specified,
schwannoma, myositis ossificans, synovial
sarcoma, and fibroma. This may be partly due to the
relatively few studies delineating the characteristic
imaging features of this entity. The preoperative
differentiation of angioleiomyoma from other soft
tissue tumours is of clinical importance, especially
sarcomas, since angioleiomyomas are benign and can
be treated with simple excision. Literature review of
the MRI findings of currently published reports and
series of vascular leiomyomas of the extremities is
presented below.
Literature review
Materials, methods, and patient demographics
A PubMed search of the English literature
was performed, using the key words “vascular
leiomyoma”, “angioleiomyoma”, and “angiomyoma”.
From 1998 to 2011, 36 cases of biopsy-proven
vascular leiomyomas in the extremities of adults
with detailed descriptions of T1-weighted images
(T1WI) and T2-weighted images (T2WI) were
found. Articles without detailed descriptions or
figures of T1WI and T2WI were excluded. Not all
studies in the literature may have been included in
this review because of unavailability in PubMed or
in English language. After including our case, this
review has 37 cases. The mean age of the patients
was 51 years (range, 20-72 years). There were 16 male
and 17 female patients; the gender of the remaining
four patients was not stated.
Results
Among the 26 lesions with documented sizes, the
mean size of the lesions was 3.2 cm (range, 0.4-12
cm). Overall, 40.5% (15/37) of the lesions were in the
upper limb and 59.5% (22/37) were in the lower limb.
All of them were located in the subcutaneous layer,
were well-defined, and round, oval or disc-shaped.
On T1WI, 91.9% (34/37) of the tumours showed
isointense–to–slightly high signal intensity, 5.4%
were heterogeneous, and 2.7% showed low signal
intensity. On T2WI, all the cases demonstrated high
signal intensity. Signal voids were seen in 10.8% (4/37)
of the tumours, either on T1WI or T2WI. Among the
33 cases in which contrast was administered, only two
(6.1%) cases showed no or poor enhancement, 93.9%
(31/33) showed enhancement, 42.4% (14/33) were
homogeneous, and 39.4% (13/33) were described
as showing heterogeneous enhancement. One case
showed peripheral enhancement, one showed central
enhancement. One case showed rapid enhancement
and one case demonstrated slow enhancement.
Among the cases in which the presence or absence
of peripheral hypointense rim was recorded, a
hypointense rim was found on T2WI in 85.2% of
cases (23/27; Table1 2 3 4 5 6 7 8 9 10 11 12 13 14).
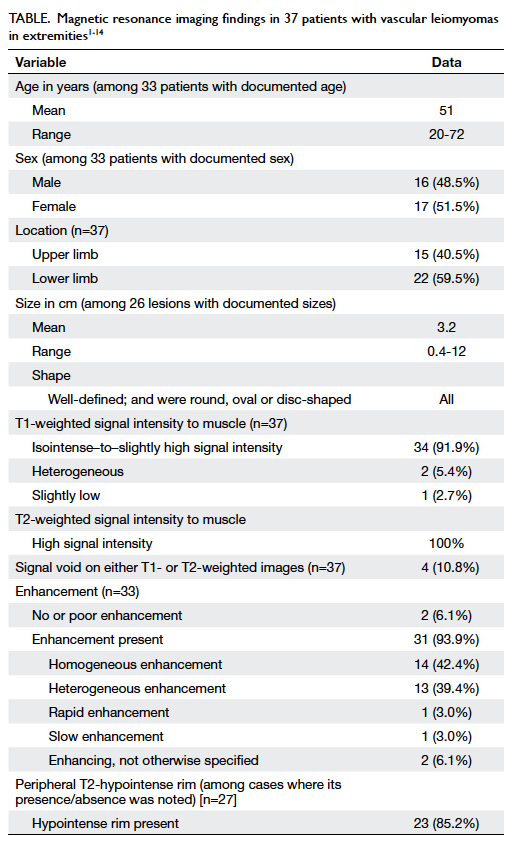
Table. Magnetic resonance imaging findings in 37 patients with vascular leiomyomas in extremities1 2 3 4 5 6 7 8 9 10 11 12 13 14
Vascular leiomyomas often show similar signal
intensity to that of muscle on T1WI. A T2WI is
expected to demonstrate mixed areas that are hyper- and
isointense to muscle. A well-defined peripheral
T2-hypointense rim may be seen, representing
the fibrous capsule. It has been reported that T2-hyperintense areas correlated with strong contrast
enhancement, whereas isointense areas did not show
enhancement after intravenous administration of
contrast material.3 It was suggested that the smooth
muscle and numerous vessels corresponded to the
hyperintense areas, and the fibrous tissue appeared
isointense on T2WI. Tortuous vascular structures
with signal void may also be seen.
Imaging differentials
The differentials of a well-defined, enhancing,
subcutaneous nodule or mass with T2-hyperintense
signals include synovial sarcoma, other low-grade
soft tissue sarcomas, haemangioma, neurogenic
tumour, and nodular fasciitis.
Low-grade sarcomas such as synovial sarcoma
and low-grade myxofibrosarcoma may be slow-growing and appear well-circumscribed on MRI,
giving the misleading impression that the lesion
is well-localised. Haemorrhage may be present in
synovial sarcomas, which may be seen as fluid-fluid
levels, T2 hypointensity, or “triple signal intensity”,
namely areas of hyperintensity, isointensity and
hypointensity relative to fat, due to presence of
cystic, solid and fibrous elements with haemorrhage.
It is unknown whether the absence of haemorrhage,
a more homogeneous appearance, and the presence
of a peripheral hypointense rim are reliable
distinguishing features favouring angioleiomyoma
over otherwise benign-appearing, soft tissue
sarcomas; this may be a potential knowledge gap that
future prospective comparison studies may serve to
fill.
Haemangiomas may show homogeneous
signals if these are small, making it challenging to
differentiate from angioleiomyomas. Phleboliths
can be sought for on plain radiographs. Fatty and
serpentine vascular elements may be identified in
haemangiomas, which are pathognomonic. The
classical ‘target’ sign, ‘split-fat’ sign, and fusiform
tumour shape demonstrated in neurogenic tumours
are not found in angioleiomyomas. Although nodular
fasciitis demonstrates similar shape and size as
angioleiomyomas, linear extension along the fascia,
surrounding oedema, low T1 signal, heterogeneous
T2 signal, and non-homogeneous enhancement
are features that differ from characteristic imaging
features of angioleiomyoma.15
On microscopic examination, the presence
of tortuous vascular channels surrounded by
smooth muscle bundles and areas of myxoid change
may be seen. This explains the heterogeneity of
signal intensity in the tumour on T2WI. Magnetic
resonance imaging–histopathological correlation
published by Hwang et al2 stated that the smooth
muscle and numerous vessels within each type
of vascular leiomyoma corresponded with the
hyperintense areas on T2WI, and the tough fibrous
tissue appeared isointense on T2WI. In addition,
a well-defined peripheral hypointense area on
T2WI correlated with the fibrous capsule, and the
interlacing isointense areas within the tumour
correlated with the various quantity of connective
tissue and intravascular thrombus.3
Conclusions
Vascular leiomyoma should be considered a possible
diagnosis when a well-demarcated oval or round
subcutaneous mass with T1-isointense–to–slightly
high signal, T2-high signal intensity, hypointense
rim, and intense enhancement is seen in the soft
tissue of the extremities. It is unknown whether
the absence of haemorrhage, a more homogeneous
appearance, and the presence of a peripheral
hypointense rim are reliable distinguishing features
favouring angioleiomyoma over otherwise benign-appearing
soft tissue sarcomas; this may be a
potential knowledge gap that future prospective
comparison studies may serve to fill.
References
1. Gupte C, Butt SH, Tirabosco R, Saifuddin A.
Angioleiomyoma: magnetic resonance imaging features in
ten cases. Skeletal Radiol 2008;37:1003-9. CrossRef
2. Hwang JW, Ahn JM, Kang HS, Suh JS, Kim SM, Seo
JW. Vascular leiomyoma of an extremity: MR imaging–pathology
correlation. AJR Am J Roentgenol 1998;171:981-5. CrossRef
3. Yoo HJ, Choi JA, Chung JH, et al. Angioleiomyoma in soft
tissue of extremities: MRI findings. AJR Am J Roentgenol
2009;192:W291-4. CrossRef
4. Kinoshita T, Ishii K, Abe Y, Naganuma H. Angiomyoma
of the lower extremity: MR findings. Skeletal Radiol
1997;26:443-5. CrossRef
5. Turhan-Haktanir N, Haktanir A, Demir Y, Tokyol C,
Acar M. Toe leiomyoma: A case report with radiological
correlation. Acta Chir Belg 2006;106:92-5.
6. Nagata S, Nishimura H, Uchida M, Hayabuchi N, Zenmyou
M, Fukahori S. Giant angioleiomyoma in extremity: report
of two cases. Magn Reson Med Sci 2006;5:113-8. CrossRef
7. Hamoui M, Largey A, Ali M, et al. Angioleiomyoma in the
ankle mimicking tarsal tunnel syndrome: a case report and
review of the literature. J Foot Ankle Surg 2010;49:398.e9-15.
8. Shafi M, Hattori Y, Doi K. Angioleiomyoma of distal ulnar
artery of the hand. Hand (N Y) 2010;5:82-5. CrossRef
9. Gulati MS, Kapoor A, Maheshwari J. Angiomyoma of the
knee joint: value of magnetic resonance imaging. Australas
Radiol 1999;43:353-4. CrossRef
10. Kugimoto Y, Asami A, Shigematsu M, Hotokebuchi T.
Giant vascular leiomyoma with extensive calcification in
the forearm. J Orthop Sci 2004;9:310-3. CrossRef
11. Waldt S, Rechl H, Rummeny EJ, Woertler K. Imaging of
benign and malignant soft tissue masses of the foot. Eur
Radiol 2003;13:1125-36.
12. Sookur PA, Saifuddin A. Indeterminate soft-tissue tumors
of the hand and wrist: a review based on a clinical series of
39 cases. Skeletal Radiol 2011;40:977-89. CrossRef
13. Okahashi K, Sugimoto K, Iwai M, Oshima M, Takakura Y.
Intra-articular angioleiomyoma of the knee: a case report.
Knee 2006;13:330-2. CrossRef
14. Stock H, Perino G, Athanasian E, Adler R. Leiomyoma of
the foot: sonographic features with pathologic correlation.
HSS J 2011;7:94-8. CrossRef
15. Walker EA, Fenton ME, Salesky JS, Murphey MD. Magnetic
resonance imaging of benign soft tissue neoplasms in
adults. Radiol Clin North Am 2011;49:1197-217. CrossRef
Find HKMJ in MEDLINE:

