DOI: 10.12809/hkmj134105
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Fluoroquinolone-induced Achilles tendinitis
PK Tam, MB, BS, FHKAM (Medicine); Carmen TK Ho, MB, BS, FHKAM (Medicine)
Department of Medicine, Tung Wah Hospital, 12 Po Yan Street, Sheung Wan, Hong Kong
Corresponding author: Dr PK Tam (alvintam@graduate.hku.hk)
Abstract
We report a case of Achilles tendinitis after intake
of ciprofloxacin for treatment of respiratory tract
infection. Fluoroquinolone-induced tendinopathy is
an uncommon but increasingly recognised adverse
effect of this antibiotic class. Most of the cases
occur in the Achilles tendon and may lead to tendon
rupture. Possible predisposing risk factors include
use of steroid, patients with renal impairment or
renal transplant, old age, and being an athlete.
The drug should be stopped once this condition is
suspected. Symptomatic treatment should be given
and orthopaedic referral is desirable if tendon
rupture occurs.
Case report
A 59-year-old woman with good past health,
except for post-radioiodine hypothyroidism on
T4 replacement, had a 3-week history of cough
with yellowish sputum but no fever. She visited a
general practitioner and was prescribed a course of
ciprofloxacin for possible respiratory tract infection.
Three days after starting the drug, she noticed
pain and swelling over the left heel. She was not
on any other medications including steroid. She
went hiking regularly and there was no history of
trauma. There was no history of joint or tendon
problems. On presentation in May 2012, physical
examination revealed tenderness and swelling
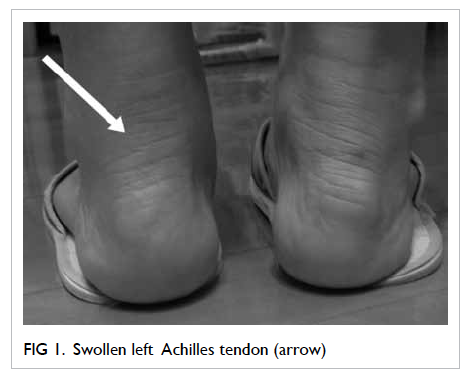
over the left Achilles tendon (Fig 1). Ultrasound revealed Achilles tendinitis with increased flow on power Doppler signal. There were no signs of tear or calcium deposition (Fig 2). Due to the temporal relationship and the absence of other obvious causes, the diagnosis was ciprofloxacin-induced Achilles tendinitis (the Naranjo Scale was 7, ie probable adverse drug reaction).1 Ciprofloxacin was stopped and the patient was advised to avoid hiking until symptoms subsided completely. She recovered fully 2 weeks later.
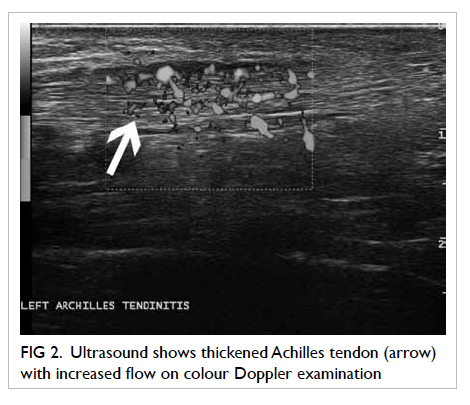
Figure 2. Ultrasound shows thickened Achilles tendon (arrow) with increased flow on colour Doppler examination
Discussion
Fluoroquinolone-induced tendinopathy was first
reported in 19832 and, since then, more than 100 cases
have been reported in the literature. A case-control study from Italy found that use of fluoroquinolone
was associated with higher risk of tendon disorders as well as Achilles tendon rupture (odds ratios, 1.7
and 4.1, respectively) compared with the control population.3 Another case-control study done in the
United Kingdom estimated the risk to be 3.2 cases per 1000 patient-years.4
The commonest fluoroquinolones in
the reported cases included ciprofloxacin and
pefloxacin but, essentially, all the commonly used
fluoroquinolones such as levofloxacin, ofloxacin, and
norfloxacin have been associated with this adverse
event.
Achilles tendon is the commonest affected
site, accounting for nearly 90% of the reported cases.
Other tendons like quadriceps tendon, rotator cuff
tendon, as well as the site of tendon insertion may
also be affected (there were two cases of epicondylitis
reported after quinolone use).5 Tendinitis was the
commonest pathology, present in 83.7% of the
cases. Tendon rupture occurred in about 40% of the
patients.6 A case-control study found that patients
taking fluoroquinolones had a 4-fold increased
risk of Achilles tendon rupture compared with the
general population.3 Other complications related to
tendinitis, such as carpal tunnel syndrome, are also
possible.7
The mean time of symptom onset was about
2 weeks after initiation of the culprit medication,
although it could range from 2 hours to as long as
6 months and, in 50% of the cases, it started within
6 days of drug intake. The mean age of affected
subjects was 59 years.6
Several risk factors have been identified in the development of tendinopathy in patients taking fluoroquinolones. Among them, steroid use was the most significant risk factor. Most of the time, this was related to long-term use of systemic steroids, although even inhaled steroids were thought to be associated with the development of quinolone-induced tendinopathy.8 Other risk factors include old age (>60 years old), haemodialysis, renal impairment, renal transplant recipients, participation in sports
activities, and history of rheumatic disorders.6 9
One previous review stated that males were more likely to develop this side-effect.6 One more recent case-crossover study, however, found that the association of tendinopathy and fluoroquinolone use was stronger in females, although not statistically significant.10 Therefore, it is not sure whether a particular gender is more likely to have this problem.
The underlying pathophysiology of the
tendinopathy is not entirely known. A number
of possible mechanisms have been proposed in
animal and in-vitro studies. Ciprofloxacin could
affect the metabolism of fibroblasts in tendon
structures by reducing collagen synthesis and
increasing extracellular matrix degradation.11 The
chelating property of fluoroquinolones may also
disturb the physiological interaction between cells
and extracellular matrix.12 There was also evidence
that fluoroquinolone increased apotosis in human
tenocytes.13 In renal transplant recipients, the
clearance of the drug may be impaired resulting in
elevated concentrations in the tendon structures.
Other risk factors like age, repeated trauma due to
sports activities, or steroid therapy may impair the
repair process of the tendon, thus, increasing the
risk of tendinopathy in this group of patients.6 14
The tendinopathy usually presents with acute
or subacute onset of pain and swelling over the
tendon. Together with a history of recent consumption
of fluoroquinolones and absence of other obvious
causes of the tendinopathy, the diagnosis can be
established. Imaging like ultrasound or magnetic
resonance imaging is not mandatory but can aid in
diagnosis, especially for visualising deep structures.
Typical ultrasound findings of tendinopathy include
thickened tendon with increased flow on colour
Doppler examination.
The most important step in management is
to stop the culprit drug. Appropriate rest and pain
control are important. Pain can be well-controlled
by non-steroidal anti-inflammatory agents; non-pharmacological
treatments include ice therapy and
therapeutic ultrasound. In case of tendon rupture,
early referral to orthopaedic surgeon is desirable.
Treatment options include immobilisation with
casting or operative repair.
Prevention is also very important. One should
only use fluoroquinolones when really necessary. Our
patient’s symptoms did not suggest genuine lower
respiratory tract infection; therefore, prescription
of antibiotics was indeed not indicated. Moreover,
quinolone is not the recommended first-line
empirical antibiotic for treatment of chest infection
in Hong Kong (it should only be considered in
patients who are sensitive to penicillin or macrolide
group of antibiotics). When use of antibiotics is
really deemed necessary, fluoroquinolones should
be avoided in patients with risk factors. Those with
a history of fluoroquinolone-related tendinopathy
should not be prescribed drugs of this class. We
should also avoid co-prescription with steroid. If
no better alternative is available, patients should be
warned of this potential adverse effect and advised
to stop the drug and seek medical advice if there
are symptoms suggestive of tendinopathy. Athletes
who are prescribed with fluoroquinolones should
be advised to alter their training regimen (reduction
in high-intensity and ballistic activities, decrease
in total training volume) during the course of the
antibiotics.14
References
1. Naranjo CA, Busto U, Sellers EM, et al. A method for
estimating the probability of adverse drug reactions. Clin
Pharmacol Ther 1981;30:239-45. CrossRef
2. Bailey RR, Kirk JA, Peddie BA. Norfloxacin-induced
rheumatic disease. N Z Med J 1983;96:590.
3. Corrao G, Zambon A, Bertù L, et al. Evidence of tendinitis
provoked by fluoroquinolone treatment: a case control
study. Drug Saf 2006;29:889-96. CrossRef
4. van der Linden PD, Sturkenboom MC, Herings RM,
Leufkens HG, Stricker BH. Fluoroquinolones and risk
of Achilles tendon disorders: case-control study. BMJ
2002;324:1306-7. CrossRef
5. Le Huec JC, Schaeverbeke T, Chauveaux D, Rivel J,
Dehais J, Le Rebeller A. Epicondylitis after treatment
with fluoroquinolone antibiotics. J Bone Joint Surg Br
1995;77:293-5.
6. Khaliq Y, Zhanel GG. Fluoroquinolone-associated
tendinopathy: a critical review of the literature. Clin Infect
Dis 2003;36:1404-10. CrossRef
7. Liang VY, Ghearing GR, Zivkovic SA. Carpal tunnel
syndrome after ciprofloxacin-induced tendinitis. J Clin
Neuromuscul Dis 2010;11:165-6. CrossRef
8. Schwald N, Debray-Meignan S. Suspected role of ofloxacin
in a case of arthralgia, myalgia, and multiple tendinopathy.
Rev Rhum Engl Ed 1999;66:419-21.
9. Tsai WC, Yang YM. Fluoroquinolone-associated
tendinopathy. Chang Gung Med J 2011;34:461-7.
10. Wise BL, Peloquin C, Choi H, Lane NE, Zhang Y. Impact
of age, sex, obesity, and steroid use on quinolone-associated
tendon disorders. Am J Med 2012;125:1228.e23-1228.e28.
11. Williams RJ 3rd, Attia E, Wickiewicz TL, Hannafin JA. The
effect of ciprofloxacin on tendon, paratenon and capsular
fibroblast metabolism. Am J Sports Med 2000;28:364-9.
12. Shakibaei M, Pfister K, Schwabe R, et al. Ultrastructure
of Achilles tendons of rats treated with ofloxacin and fed
a normal or magnesium-deficient diet. Antimicrob Agents
Chemother 2000;44:261-6. CrossRef
13. Sendzik J, Shakibaei M, Schäfer-Korting M, Stahlmann R.
Fluoroquinolones cause changes in extracellular matrix,
signalling proteins, metalloproteinases and caspase-3 in
cultured human tendon cells. Toxicology 2005;212:24-36. CrossRef
14. Hal MM, Finnoff JT, Smith J. Musculoskeletal complications
of fluoroquinolones: guidelines and precautions for usage
in the athletic population. PM R 2011;3:132-42. CrossRef