Hong Kong Med J 2014;20(6):511–8 | Epub 29 Aug 2014
DOI: 10.12809/hkmj134150
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Nurse-led orthopaedic clinic in total joint replacement
Jason CH Fan, FHKAM (Orthopaedic Surgery); Carmen KM Lo, MN; Carson KB Kwok, FHKAM (Orthopaedic Surgery); KY Fung, FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and Traumatology, Alice Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
This study was presented at the 33rd Annual Congress of the Hong Kong
Orthopaedic Association on 23 November 2013.
Corresponding author: Dr Jason CH Fan (fchjason@netvigator.com)
Abstract
Objectives: To introduce the practice of a nurse-led
orthopaedic clinic for managing stable patients
after total hip or knee replacement and to evaluate
its efficacy.
Design: Case series.
Setting: A public hospital in Hong Kong.
Patients: Patients who had stable primary total knee
replacement or total hip replacement done for longer
than 2 years were managed in a nurse-led total joint
replacement pilot clinic.
Results: From July 2012 to March 2014, 431 patients
(including 317 with total knee replacement and
114 with total hip replacement) were handled, and
408 (94.7%) nurse assessments were independently
performed. Six cases of prosthesis-related
complications were diagnosed. One patient was
hospitalised for prosthetic complications within
3 months after follow-up. The satisfaction rate
was 100%. From November 2012 to April 2013, an
advanced practice nurse, one resident specialist,
and one associate consultant independently charted
Knee Society Knee Score or Harris Hip Score for the
patients attending preoperative assessment clinic
to check the inter-observer reliability. Overall, 23
patients with 37 knees and 11 patients with 17 hips
were examined. The mean correlation coefficient
between assessments by the associate consultant
and advanced practice nurse was 0.912 for Knee
Society Knee Score, and 0.761 for Harris Hip Score.
The advanced practice nurse could achieve better
or equally good correlation with associate consultant when compared with the correlation between resident specialist and associate consultant (0.866 and 0.521 for Knee Society Knee Score and Harris Hip Score, respectively) and with international standard.
Conclusion: Nurse-led total joint replacement clinic
was safe, reliable, and well accepted by patients.
New knowledge added by this
study
- Management of stable postoperative total joint replacement patients by well-trained nurses is safe, reliable, and well accepted by patients.
- Nurse-led clinics should be established for managing patients with total joint replacement to handle the escalating workload in Hong Kong.
- Well-structured nurse training should be organised for managing stable patients with total joint replacement in orthopaedic clinics.
Introduction
Nursing practice is moving towards both
proletarianisation and professionalisation.1 The
former means the transfer of some basic routine care
to less-skilled assistants. The latter means advanced
nursing practice with nurses handling complex
health problems using advanced health assessment
and intervention measures. Nurse-led clinic is one
of the forms of professionalisation and has been
adopted in Hong Kong since 1990s. Diabetes clinic,
wound clinic, and continence clinic are the three
most common nurse-led clinics in Hong Kong2
and they have demonstrated significant impact on
patient outcomes.3 Orthopaedic nurses in total joint
replacement (TJR) have been focusing on patient
education in preoperative assessment clinics.
In order to enhance the role of orthopaedic
nurses and ensure the continuity of patient care
before and after TJR, a new advanced nursing
practice was introduced, namely, the Ambulatory
Comprehensive Arthroplasty Clinic (ACAC), a
nurse-led orthopaedic postoperative clinic in TJR.
An advanced practice nurse (APN) with 17 years of
post-registration experience and 5 years of advanced
nursing practice was interviewed and showed
dedication and enthusiasm towards the orthopaedic
work in TJR. She received some basic training from
November 2011 and the ACAC started in January
2012. She ran the clinic one session each week
under the supervision of an associate consultant
(AC) till June 2012, and then independently. She
was supported by a multidisciplinary team and
could refer patients to physiotherapy, occupational
therapy, and prosthetics and orthotics as indicated.
She also participated in a multidisciplinary meeting
for day-patient rehabilitation after TJR.
The APN continued with her one-on-one
training by an AC specialised in TJR. Each week,
she observed about 15 cases in the specialist TJR
clinic and two cases in the preoperative assessment
clinic. She was exposed to and was taught the basic
knowledge on total knee replacement (TKR) and
total hip replacement (THR), the proper way to
chart Knee Society Knee Score (KSKS) and Harris
Hip Score (HHS), and about physical findings
and radiographic features of stable prosthesis,
infection, and aseptic loosening. Reading material
and tutorials were also provided to teach her about
various complications of TJR. Until March 2014, she
completed about 110 weeks of continuous training.
As we have been using KSKS and HHS since
1998 for assessing the progress of patients after TJR,
these were retained as part of the assessment tools
in ACAC for continuity of care. In part of the KSKS
and HHS, physical examination is necessary. It was a
difficult area for the APN and could lead to potential
error and discrepancy. Therefore, part of the APN
training was concentrated in this area and a separate
study was launched to test her reliability.
This article aimed to introduce the practice of
a nurse-led orthopaedic clinic for managing stable
postoperative patients with TKR and THR and
describe the outcomes in a series of cases. This also
presents the result of the reliability of the APN in
charting various scores.
Methods
From August 1997 to December 2013, 895 primary
TKRs and 268 primary THRs were performed in
Alice Ho Miu Ling Nethersole Hospital. Until 31
December 2013, 801 TKRs and 232 THRs were
performed for more than 2 years and were followed
up yearly in the specialist out-patient clinic. During
each follow-up, the assessment included history
taking and physical examination, charting KSKS
or HHS, and checking radiographs. Patients who
had undergone primary TKR or THR more than 2
years ago and who were assessed as being stable and
minimally symptomatic by specialists were recruited
in the ACAC for yearly follow-up. One day before
follow-up, the AC analysed the radiographs taken in
the earlier year and the finding was discussed with
the APN for teaching purpose. During ACAC, the
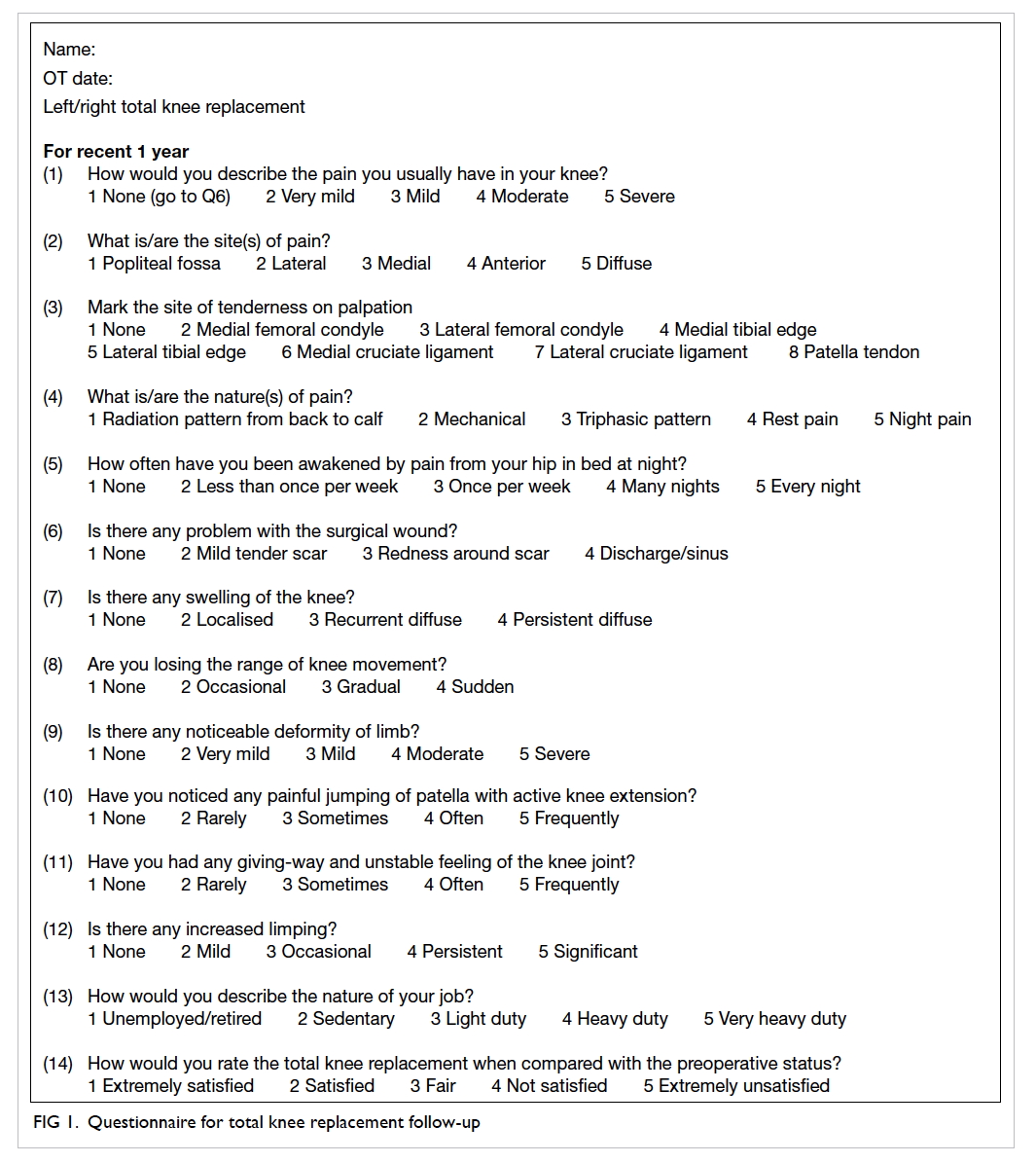
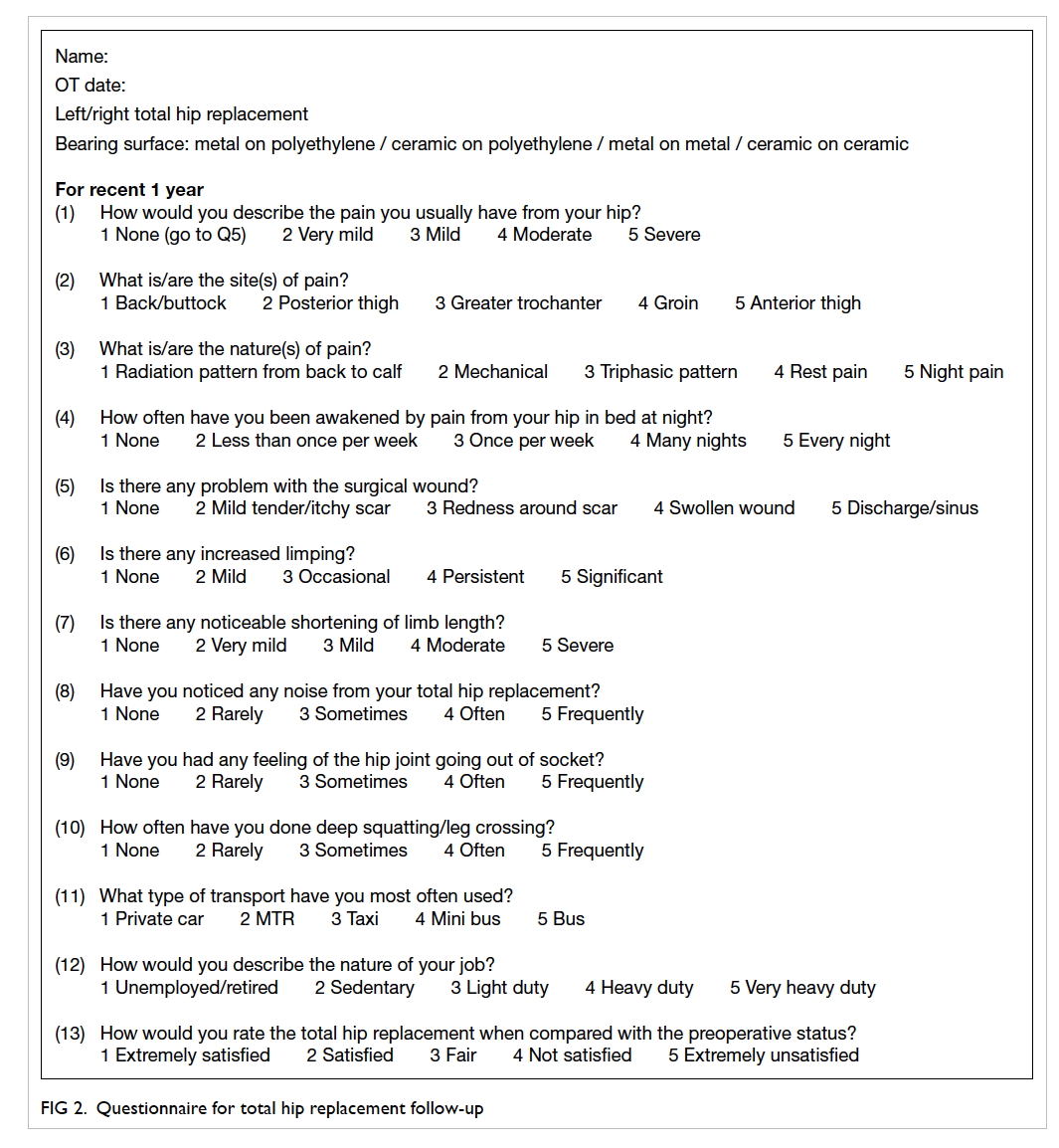
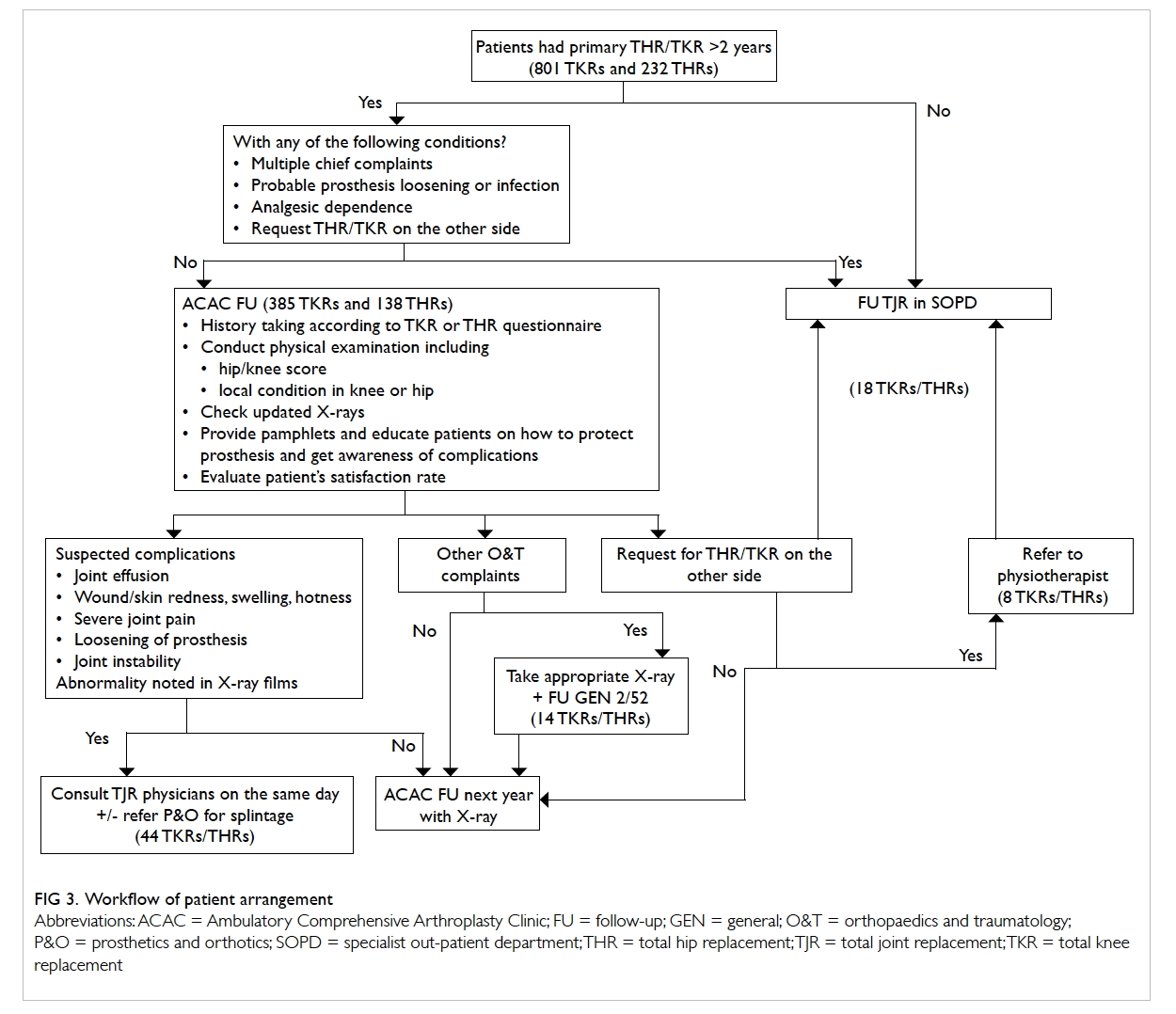
APN assessed the patients by TKR (Fig 1) or THR (Fig
2) questionnaire, charted KSKS or HHS, interpreted
follow-up radiographs, and then educated the patients
on care of and precautions with the prosthesis. The
findings were recorded in consultation notes in the
computer medical system (CMS). Patients were
managed according to the workflow (Fig 3). When the
TJR specialist was consulted on-site for any problem
related to the prosthesis, minor procedures like knee
aspiration could be done by the specialist at the same
consultation. After the clinic, the questionnaires and
the radiographs were screened by the specialist for
any significant problems.
The questionnaires were collected and the
consultation notes in CMS were studied. The
relevant data were then summarised and described
in an Excel file, including the number of cases of
TKRs and THRs, the number of on-site specialist
consultations, the number of prosthesis-related
complications diagnosed by the APN, the number
of patients referred to orthopaedic clinic and other
health care professionals, the number of medication
prescriptions, patients’ satisfaction, and patients’
acceptance of consultation without medication.
Patients’ waiting time for the clinic was also
obtained by calculating the difference between the
consultation time and the allocated time slot. The
CMS was also checked for any hospital admission
or clinic attendance for any problems related to TJR
after ACAC follow-up.
From November 2012 to April 2013, an APN,
one resident with specialist qualification (RS), and
one AC independently charted KSKS or HHS for
patients attending the preoperative assessment
clinic. Knee Society Knee Score is composed of
function score (FS) and knee score (KS)—FS is
made up of three components and KS is made up of
seven components. Harris Hip Score is composed of
17 components. Overall, 23 patients with 37 knees
and 11 patients with 17 hips were examined. In
order to analyse the inter-rater reliability between
the AC and APN (comparison A), between AC
and RS (comparison B), and between RS and APN
(comparison C), each component of the KSKS and
HHS was analysed for single-measure intraclass
correlation coefficient (ICC) and statistical
significance using the Statistical Package for the
Social Sciences (Windows version 15.0; SPSS Inc,
Chicago [IL], US). To see any statistically significant
difference between ICCs among the three groups
and between comparison A and international
standards,4 5 Fisher’s z-transformation was performed
by online calculator (www.vassarstats.net/rdiff.html).
Results
In the initial period from January to June 2012,
on-site specialist consultation was necessary in 21
(22.8%) cases out of the 92 cases (68 TKRs and 24
THRs). From July 2012 to March 2014, a total of 431
patients (including 317 TKRs and 114 THRs) were
managed and 408 (94.7%) nurse assessments were
independently performed. Six cases of prosthesis-related
complication were diagnosed including two
cases of patellar clunk in TKR, two cases of TKR
loosening, and two cases of THR loosening. Number
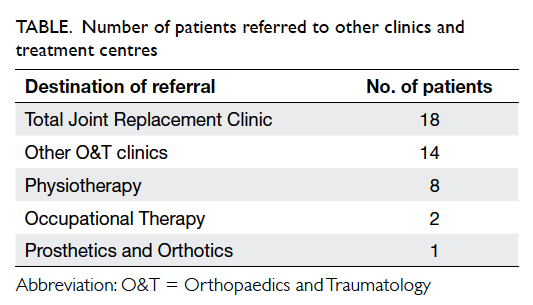
of referrals to other orthopaedic clinics and health
care professionals is shown in the Table. Among the 523 patients on ACAC follow-up, 131 (25.0%) requested medications. Average patient waiting time improved over the study period (26 minutes in December
2012, 18 minutes in April 2013, and 14 minutes in
March 2014). Of these 523 patients, 485 patients were interviewed; 354 were extremely satisfied and 131 were satisfied with ACAC follow-up by the nurse, and 373 (76.9%) patients accepted follow-up without drug prescription.
One patient who had undergone right TKR 12
years ago was hospitalised at 3 months after nurse
clinic follow-up because of sudden onset of right
knee effusion. X-ray showed no sign of prosthesis
loosening. Surgical exploration of the right knee
showed catastrophic wear of the polyethylene insert
while the prosthesis was stable. Two patients at 6
months after nurse assessment attended general out-patient
clinic for getting analgesics.
Study of reliability of the advanced practice
nurse in charting Knee Society Knee Score
and Harris Hip Score
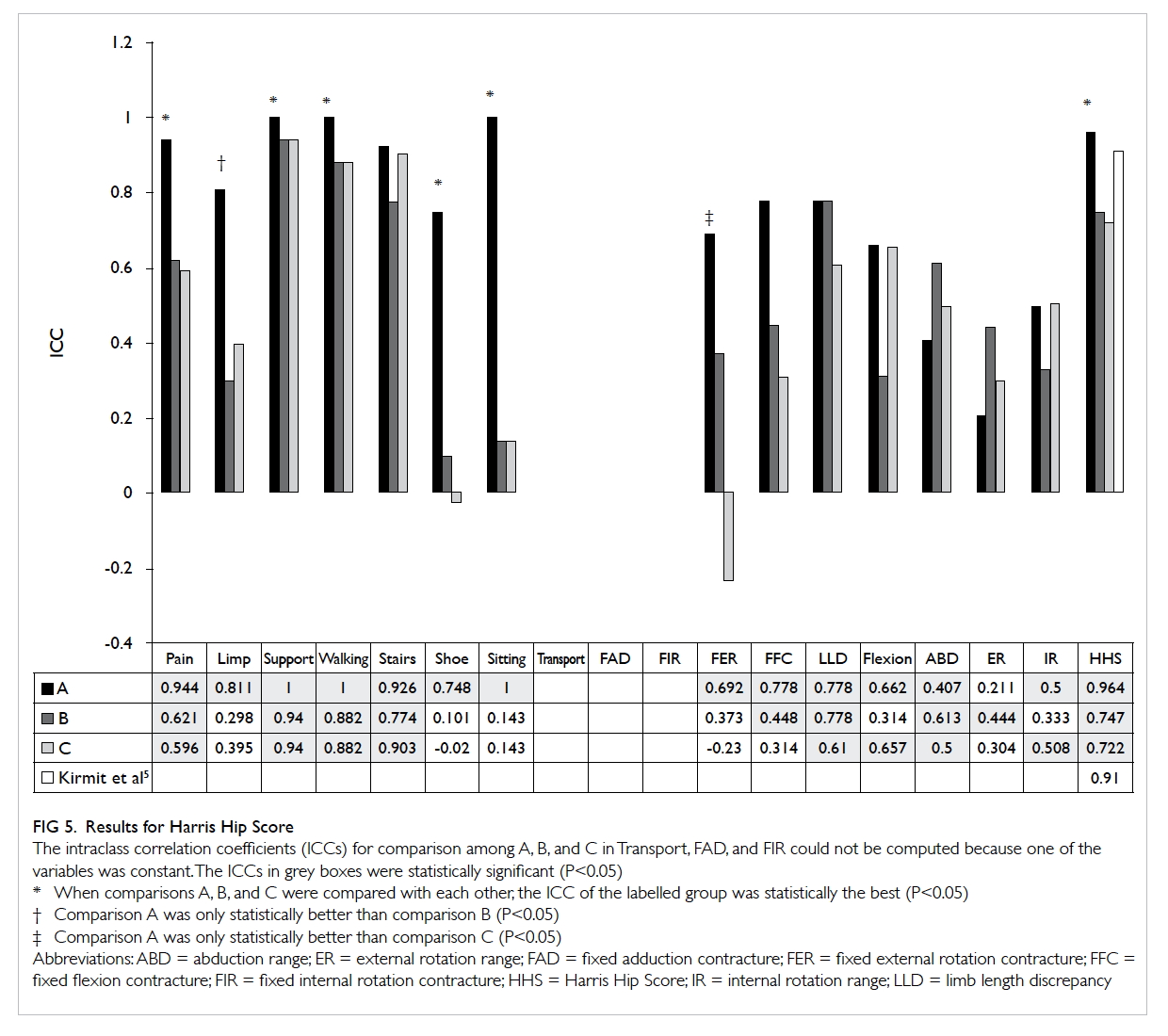
The result for KSKS is shown in Figure 4. The mean
ICCs were 0.912 (range, 0.660-0.987), 0.866 (range,
0.735-0.974), and 0.851 (range, 0.599-0.996)
for comparisons A, B and C, respectively. The
lowest ICC among all the components in KSKS was
that of mediolateral stability (0.599-0.797). When
comparing with those of Bach et al,4 the ICCs of
FS and all its components for comparison A were
significantly better. This was also the case for ICCs
of three of the five computable components of KS
and that of KS.
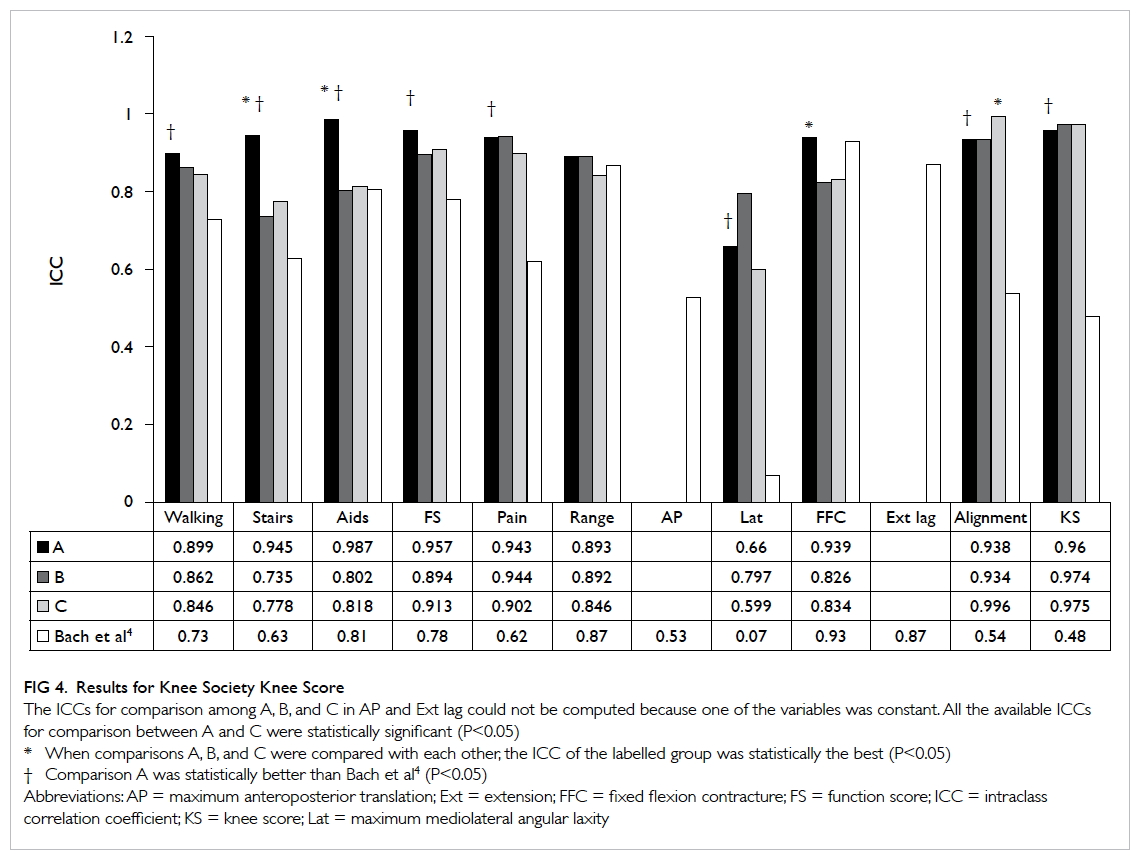
Figure 4. Results for Knee Society Knee Score
The ICCs for comparison among A, B, and C in AP and Ext lag could not be computed because one of the variables was constant. All the available ICCs for comparison between A and C were statistically significant (P<0.05)
The result for HHS is shown in Figure 5.
The mean ICCs were 0.761 (range, 0.211-1) for
comparison A, 0.521 (range, 0.101-0.940) for
comparison B, and 0.481 (range, -0.231 to 0.940) for
comparison C. The ICCs for charting total HHS were
0.964, 0.747, and 0.722 for comparisons A, B and C,
respectively. When the ICC of comparison A (0.964)
was compared with that in the study by Kirmit et al5
(0.91), the difference was found to be statistically insignificant (P=0.124).
Discussion
In the current study, the well-trained APN
could independently handle 94.7% of the stable
postoperative cases in TJR after the initial learning
phase. She could successfully diagnose six cases
of prosthesis-related complications out of all the
523 patients she handled. One patient who was
asymptomatic at the ACAC follow-up presented
with sudden onset of right knee effusion, and showed
catastrophic wear of polyethylene. Nurse-led clinic
in TJR was, therefore, safe. It was well accepted by
patients with a 100% satisfaction rate. As the APN
grew more confident and gained more experience,
she also became more efficient. This, together with
improvement in workflow in taking radiographs, led
to progressive shortening of patient waiting time
from 26 minutes in the initial phase (December
2012) to 14 minutes in March 2014. It could greatly
relieve the burden of the specialist clinic. Within
2 years, 523 patient attendances were handled by
the APN. About five to seven cases were seen in
each session of this clinic. Moreover, more detailed
patient education, which is not possible in the busy
specialist clinic, can be provided to patients who
may have forgotten the details given several years
ago before the operation.
Bach et al4 studied the inter-observer correlation
of four commonly used TKR outcome scores—Hungerford score, Hospital for Special Surgery
score, Knee Society score, and Bristol score. Two
experienced orthopaedic surgeons independently
assessed 118 TKRs in 92 patients. The correlation
coefficient for mediolateral knee stability was the
lowest among all the components of all scoring
systems (0-0.38). This was due to the difficulty in
physical examination and proper measurement with
goniometer at the same time. For all the comparisons
in this study, we encountered the same difficulty
and found the same finding of lowest correlation
coefficient for mediolateral stability (0.599-0.797)
among all the components in KSKS. Kirmit et al5
evaluated the inter-observer reliability of five different
hip scores including HHS. Three physiotherapists
assessed 48 hips with osteoarthritis in 35 patients.
The correlation coefficients ranged from 0.82 to 0.91
for HHS, which was comparable to the result in
our study (0.722-0.964). With proper training of the
APN by the AC in this hospital, she could achieve
better or equally good correlation with the AC
as compared with an orthopaedic specialist and
international standard for charting KSKS and HHS.
In order to match the evolution of the health
care environments and patient care needs, the roles
and responsibilities of APNs have been reshaping.6
They have active and important places in taking
care of patients from various specialties. Their
contribution by running nurse-led clinics has been
shown to be tremendous in and outside Hong Kong.
They add value to patient care and complement
specialist clinics.3 7 8 9 Over 80% of their work are
independent of or interdependent with physicians
and involve skills such as adjusting medications, and
initiating therapies and diagnostic tests according to
protocols.3 10 To further advance professionalisation of nursing practice, Newey et al11 reported the training
of nurse practitioners to provide initial assessment in
clinics, perform carpal tunnel release, and manage
these patients in postoperative follow-up.
Shiu et al12 pointed out four boundaries
and six hindering factors for expanding advanced
nursing practice in nurse-led clinics. The
former included community-hospital, wellness-illness, public-private, and professional-practice
boundaries. The latter included stakeholder and
public awareness of advanced nursing practice role
in nurse-led clinics, provision of advanced specialty
education programmes, organisational support,
multidisciplinary collaboration, and changing
health care context and provision. When ACAC was
commenced, professional-practice boundary was the
first and the most important hurdle. The APN was
directly coached by an AC about various aspects in
TJR. The TKR and THR questionnaires and workflow
protocol were devised to facilitate the patient care
process. She was authorised to order standard
radiographs according to the region of interest,
and make referral to physiotherapy, occupational
therapy, prosthetics and orthotics, and the general
orthopaedic clinic. However, nurse prescription was
not possible and doctor prescription was necessary
in 25% of the cases. Getting help from doctors was
also required in a few cases for writing referral
letters to medical departments, applying for car park
permits for the disabled, applying for public housing,
and signing disability allowance forms. In order to
solve these remaining problems, there should be
appropriate legislation to redefine the professional
code of nursing practice, and organisational support
to offer a clear policy for nurse prescribing.12
Stakeholder and public awareness should be aroused
to allow inter-departmental referral and granting
public certification.
The second hurdle was the provision of
advanced specialty education programmes.
Currently, there is no programme or course in
universities and Hospital Authority teaching nurses
about TJR. Direct coaching was chosen as the training
method, and continuous education was provided to
broaden her exposure. This may be less than ideal and
a complete curriculum was not present. If the nurse-led
clinic were to be promoted and accepted as the
method to deal with the escalating workload from
various joint replacement centres, the Co-ordinating
Committee (COC), which is one of the Hospital
Authority Head Office committees for clinical
service, in orthopaedics and traumatology has to
collaborate with COC in nursing to formulate a good
training programme for nurses with special interest
in TJR. Knowledge of pharmacology is
also necessary for nurse prescription. The nursing
schools in various universities should revise the
curriculum to make nurse-led orthopaedic clinics
feasible and safe.
Conclusion
The success of nurse-led postoperative clinic in
TJR is multifactorial including the experience
and dedication of the APN, support of the trainer
specialist and department, a good working guideline
and protocol, and support of other health care
professionals. Its running is not perfect yet because
the specialty nurse cannot prescribe medications
and she is not community-recognised to sign
legal documents. However, such a clinic should
be established in Hong Kong to align with the
development of joint replacement centres in Hospital
Authority. Apart from the preoperative assessment
clinic and postoperative follow-up clinic, the trained
specialist nurse can also play important roles in
other stages of patient care. This requires further
exploration and collaboration with other health care
professionals.
Acknowledgements
We thank Ms Amy MY Cheng and Winnie YC Lam
for valuable inputs when setting up the nurse-led
clinic.
References
1. Wong FK. Health care reform and the transformation of
nursing in Hong Kong. J Adv Nurs 1998;28:473-82. CrossRef
2. Hospital Authority Annual Plan 2008-2009. Available from: http://www.ha.org.hk/visitor/ha_visitor_index.asp?Parent_ID=100&Content_ID=300&Dimension=100&Lang=ENG.
Accessed Aug 2010.
3. Wong FK, Chung LC. Establishing a definition for a nurse-led
clinic: structure, process, and outcome. J Adv Nurs
2006;53:358-69. CrossRef
4. Bach CM, Nogler M, Steingruber IE, et al. Scoring
systems in total knee arthroplasty. Clin Orthop Relat Res
2002;399:184-96. CrossRef
5. Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen
Z. The reliability of hip scoring systems for total hip
arthroplasty candidates: assessment by physical therapists.
Clin Rehabil 2005;19:659-61. CrossRef
6. Bonsall K, Cheater FM. What is the impact of advanced
primary care nursing roles on patients, nurses and
their colleagues? A literature review. Int J Nurs Stud
2008;45:1090-102. CrossRef
7. Larsson I, Bergman S, Fridlund B, Arvidsson B. Patients’
experiences of nurse-led rheumatology clinic in Sweden: a
qualitative study. Nurs Health Sci 2012;14:501-7. CrossRef
8. Slight C, Marsden J, Raynel S. The impact of a glaucoma
nurse specialist role on glaucoma waiting lists. Nurs Prax
N Z 2009;25:38-47.
9. Kirkwood BJ, Pesudovs K, Latimer P, Coster DJ. The
efficacy of a nurse-led preoperative cataract assessment
and postoperative care clinic. Med J Aust 2006;184:278-81.
10. Ng SL, Tse YB, Ho KL, Yiu MK. Efficacy of a Urology
Nurse-led Clinic in Queen Mary Hospital of Hong Kong.
Proceedings of the 11th Asian Congress of Urology of the
Urological Association of Asia; 2012 Aug 22-26; Pattaya,
Thailand. Int J Urol 2012;19(Suppl
1):432 abstract no. OP2512-07.
11. Newey M, Clarke M, Green T, Kershaw C, Pathak P. Nurse-led
management of carpal tunnel syndrome: an audit of
outcomes and impact on waiting times. Ann R Coll Surg
Engl 2006;88:399-401. CrossRef
12. Shiu AT, Lee DT, Chau JP. Exploring the scope of expanding
advanced nursing practice in nurse-led clinics: a multiple-case
study. J Adv Nurs 2012;68:1780-92. CrossRef