Hong Kong Med J 2014 Oct;20(5):437–43 | Epub 18 Jul 2014
DOI: 10.12809/hkmj144215
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE CME
Paediatric vesicoureteric reflux imaging: where
are we? Novel ultrasound-based voiding urosonography
KS Tse, FHKCR, FHKAM (Radiology); LS
Wong, PDDR, MAS (Sonography); HY Lau, FHKCR, FHKAM (Radiology); WS
Fok, MB, BS, FRCR; YH Chan, MB, ChB, FRCR; KW Tang, FHKCR, FHKAM
(Radiology); Susan CH Chan, FHKCR, FHKAM (Radiology)
Department of Radiology and Imaging, Queen
Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr KS Tse (sunnytse@ha.org.hk)
Abstract
Vesicoureteric reflux is an important
association of paediatric urinary tract infection. Fluoroscopic
micturating cystourethrography and radionuclide cystography have
been employed for detecting and grading vesicoureteric reflux.
However, both modalities involve ionising radiation, which can
pose significant radiation risk to growing children. They also
have a lower detection rate due to intermittent fluoroscopic
technique in micturating cystourethrography, and lower spatial
resolution in radionuclide cystography. Therefore, newer
radiation-free ultrasound-based contrast-enhanced voiding
urosonography has been developed in Europe for 15 years. This
article aimed to summarise the current literature and discuss
the first local pilot study in our institution on detection of
vesicoureteric reflux by contrast-enhanced voiding
urosonography. Contrast-enhanced voiding urosonography is a
valid alternative to micturating cystourethrography in assessing
vesicoureteric reflux, based on its superior diagnostic
performance, reliability, safety, feasibility, and radiation
safety for children. Therefore, it should be incorporated in the
guideline for investigating paediatric urinary tract infection.
Introduction
Urinary tract infection (UTI) is a common
emerging paediatric condition. It has a multifactorial aetiology,
with multiple host factors implicated in its pathogenesis.
Vesicoureteric reflux is considered one of the most important
associations of paediatric UTI. Vesicoureteric reflux refers to
the abnormal retrograde flow of urine from urinary bladder back
into the ureter or, even, to the kidney. It accounts for about 25%
to 40% of UTIs in children, with no significant difference in the
prevalence among boys and girls presenting with UTI, except in
infancy.1 A local
cross-sectional study2 demonstrated that vesicoureteric reflux was
prevalent in 30% of boys and 43% of girls presenting with
symptomatic UTI in infancy.
It is not only a developmental anomaly related to inadequate
length of intravesical submucosal ureter, but also a dysfunctional
problem in which many patients have associated bladder emptying
and bowel dysfunction.3 For
decades, it has been thought to be associated with reflux
nephropathy and renal scarring.4
Nevertheless, there are disputes about the role of vesicoureteric
reflux in the development of UTI,5
as well as the effectiveness of antibiotic prophylaxis in
preventing pyelonephritis and scarring.6
Nonetheless, it is recommended to exclude vesicoureteric reflux
in high-risk patients, including those with hydronephrosis, renal
scarring, or other findings that suggest high-grade vesicoureteric
reflux or obstructive uropathy on renal ultrasound, and in those
suffering from atypical UTI or complex clinical circumstances.7 Conventional reflux imaging modalities for
diagnosing the condition include micturating cystourethrography
(MCU)/voiding cystourethrography and radionuclide cystography
(RNC).
Micturating cystourethrography
Micturating cystourethrography has been the
gold standard of imaging for diagnosing and grading vesicoureteric
reflux. It is a fluoroscopic examination utilising radiographic
contrast medium and fluoroscopic (X-ray) screening. The procedure
involves bladder catheterization and intravesical administration
of radiographic contrast via the urinary catheter, followed by
fluoroscopic examination of the lower abdomen and pelvis. The
presence of opacification of the upper urinary tract with
radiographic contrast during bladder filling and voiding phases is
diagnostic of vesicoureteric reflux (Fig 1). A standardised international system
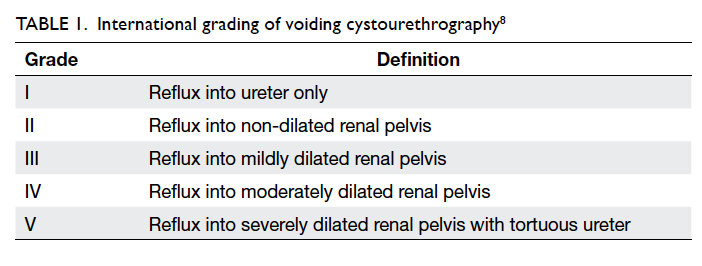
is used for grading the reflux as shown in Table 1.8
Occurrence of reflux during filling and voiding phases, which
represents low-pressure low-volume and high-pressure high-volume
conditions, respectively, has different prognostic implications.9
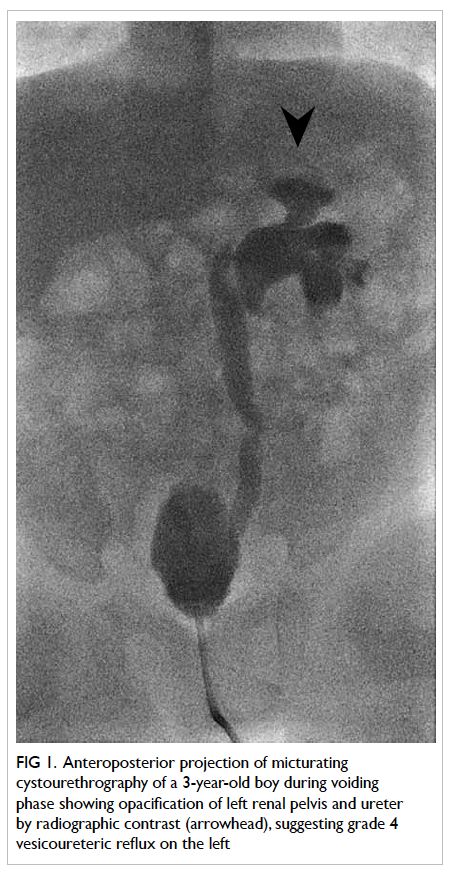
Figure 1. Anteroposterior projection of micturating cystourethrography of a 3-year-old boy during voiding phase showing opacification of left renal pelvis and ureter by radiographic contrast (arrowhead), suggesting grade 4 vesicoureteric reflux on the left
Micturating cystourethrography involves
fluoroscopy and, thus, exposure to ionising radiation. The
standard mean effective dose of MCU is approximately 0.4 to 0.9
mSv.10 To reduce radiation
exposure in both patients and operators, intermittent fluoroscopic
screening and last image hold on pulsed digital fluoroscopy are
employed. Nevertheless, children are more susceptible than adults
to the long-term hazards of radiation, because growing tissues in
children are more sensitive to radiation effects than the fully
mature tissues of adults. Furthermore, children have longer life
expectancy during which potential oncogenic effects of radiation
may be manifested.10
Recent literature shows a dramatic increase in medical radiation
burden to children arising from radiological examinations with the
expansion of medical imaging. In the United States, the number of computed
tomographic examinations doubled for children younger than 5 years
of age, and tripled for those aged 5 to 14 years between 1996 and
2005.11 It is postulated
that medical radiation can contribute to radiation-induced
cancers.10 Hence,
radiation exposure is a major drawback of MCU. Of note, as
vesicoureteric reflux is an intermittent phenomenon,12 it can sometimes be missed by intermittent
fluoroscopic screening techniques. The dilution of small amount of
radiographic contrast in the already-dilated collecting system,
and obscuration by overlying bowel shadow, also contribute to the
lower sensitivity of MCU.12
Radionuclide cystography
Direct RNC also involves bladder
catheterization and intravesical administration of
radiopharmaceuticals. It carries the advantages of continuous
examination of kidneys and bladder during filling phase, and lower
gonadal radiation dose.13
The estimated dose to the ovary is 0.005 to 0.01 mGy, and even
smaller dose to the testis.14
In general, it has comparable diagnostic performance with MCU,
with no significant difference in the detection rate.13 The mean direct cost of RNC, including the
cost of labour, as well as materials and consumables, is also
lower than that of MCU.15
However, owing to its lower spatial resolution and impaired
anatomical delineation, RNC is generally used for follow-up of
patients with known vesicoureteric reflux.14 It is not recommended as the first diagnostic
test for vesicoureteric reflux, particularly in boys due to its
limited efficacy in examining the urethral abnormality in detail.
Besides, RNC also involves ionising radiation to both children and
parents.
Novel technique: contrast-enhanced voiding
urosonography
Ultrasound-based reflux imaging has been
investigated in Europe for about 20 years.16 This modality obviates exposure of children
to ionising radiation and allows prolonged, continuous scanning.17 It is now called
‘contrast-enhanced voiding urosonography’ (ceVUS), previously
known as reflux sonography, echocystography, cystosonography, and
echo-enhanced cystography.18
19 20 The ceVUS is technically analogous to
conventional MCU, in that an ultrasound contrast agent is
administered intravesically via the urinary catheter, followed by
continuous, alternate examination of the kidneys, urinary bladder,
and retrovesical region during filling and voiding phases, as well
as the urethra via transperineal or interscrotal approach during
voiding phase. The diagnosis of vesicoureteric reflux is
determined by the presence of moving echogenic (bright)
microbubbles from ultrasound contrast in the upper urinary tract (Fig 2). Its five-tier grading system by
Darge and Troeger21 is
similar to the international reflux system, based on the presence
of reflux and dilatation of the collecting system. It allows
analogous correlation by the clinicians with the well-established
radiographic grading system. The diagnostic performance of ceVUS
was only improved since the introduction of stabilised ultrasound
contrast agent on intravesical application,20 as well as the advances in the ultrasound
techniques, namely, harmonic imaging.22
Levovist (Levovist Schering, Berlin, Germany) was the
first-generation stabilised ultrasound contrast composed of
palmitic-acid stabilised microbubbles employed in ceVUS.23 It was first introduced for intravenous use
in assessing cardiac shunts and defects in mid-1990s, and, later,
approved for intravesical application. Currently,
second-generation ultrasound contrast SonoVue (SonoVue, Bracco,
Italy) has several intrinsic advantages over Levovist.24 SonoVue is a stabilised aqueous suspension of
sulphur hexafluoride microbubbles with a phospholipid shell, which
resonate by asymmetric contraction and expansion, and strongly
increase the ultrasound backscatter allowing visualisation. It is
not readily soluble in water, and, hence, remains stable for up to
6 hours.25 In addition to
the improved intrinsic property of ultrasound contrast, tissue
harmonic imaging technique is now employed in ultrasound imaging.
Tissue harmonic imaging is based on the phenomenon of non-linear
distortion of an acoustic signal as the ultrasound wave insonates
and travels through the body tissues. It improves contrast and
spatial resolution, and reduces artefacts compared with
conventional grayscale ultrasound.26
Together with subtraction technique, contrast-specific harmonic
imaging mode further increases the conspicuity of the
microbubbles.
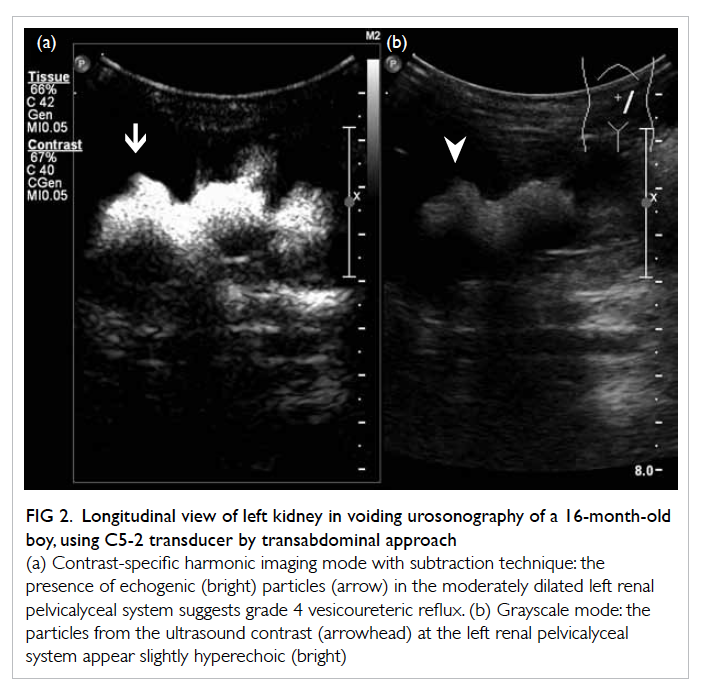
Figure 2. Longitudinal view of left kidney in voiding urosonography of a 16-month-old boy, using C5-2 transducer by transabdominal approach
With the application of newer-generation
ultrasound contrast agent and ultrasound techniques, ceVUS is
currently regarded as a valid, radiation-free imaging modality for
examining vesicoureteric reflux in Europe.27 In addition to the previous literature, the
first local pilot comparative study in Hong Kong by the authors
also supports ceVUS as a valid alternative to MCU in most clinical
indications, based on its high efficacy, reliability, high safety
profile and feasibility, and radiation safety for children.28
High diagnostic efficacy
The utilisation of stabilised ultrasound
contrast agent has revolutionised ultrasound-based reflux imaging,
by enabling prolonged sonographic examination of the upper urinary
tract. Darge29 has
confirmed the diagnostic performance of ceVUS by the
first-generation stabilised ultrasound contrast Levovist. Using
MCU as the reference method, the sensitivity of ceVUS ranged from
57% to 100%, and specificity from 85% to 100%. The diagnostic
accuracy, measuring the concordance of both positive and negative
cases, ranged from 78% to 96%. Approximately 10% of all reflux
units were diagnosed by MCU alone, and 9% were diagnosed by ceVUS
alone. However, the majority of reflux units missed on ceVUS were
of low grade, while most missed refluxes on MCU were of
medium-to-high grade.29
The intermittent nature of vesicoureteric reflux, together with
intermittent fluoroscopy, and dilution of radiographic contrast
were postulated to result in lower detection rate of high-grade
reflux on MCU. On the other hand, the lower detection rate of
low-grade reflux on ceVUS is attributed to the difficulty in
visualising retrovesical regions and non-dilated ureter related to
the acoustic shadow casted by the intravesical contrast.
Currently, the second-generation contrast
SonoVue-enhanced VUS has superior sensitivity ranging from 80% to
100%, and a specificity of 77% to 97% (Table 2).27
28 30 31 32 33 34
Diagnostic accuracy is similar to that of Levovist, at about 80%
to 98%.27 28 30 31 32 33 34 Moreover,
SonoVue-enhanced VUS has consistently higher reflux detection rate
than MCU. Data show that MCU misses 6% to 62% of all reflux units. In the study by Ključevšek et al,31
26 (62%) out of 42 reflux units were additionally identified by
ceVUS alone, but none by MCU alone. On the other hand, ceVUS
misses only 0% to 12% of all reflux units.27
28 30 31 32 33 34
Diagnostic accuracy is similar to that of Levovist, at about 80%
to 98%.27 28 30 31 32 33 34 Similarly, our pilot
study showed that ceVUS achieved 100% sensitivity and 85%
specificity, as well as 85% accuracy, in 31 patients (ie 62
kidney-ureter units). Higher detection rate was, once again,
achieved by ceVUS, where MCU had missed 64% of all reflux units (9
out of 14 reflux units), half of which were of high grade.28 Therefore, ceVUS is not only highly
concordant with MCU on reflux detection, but also more sensitive
than MCU.
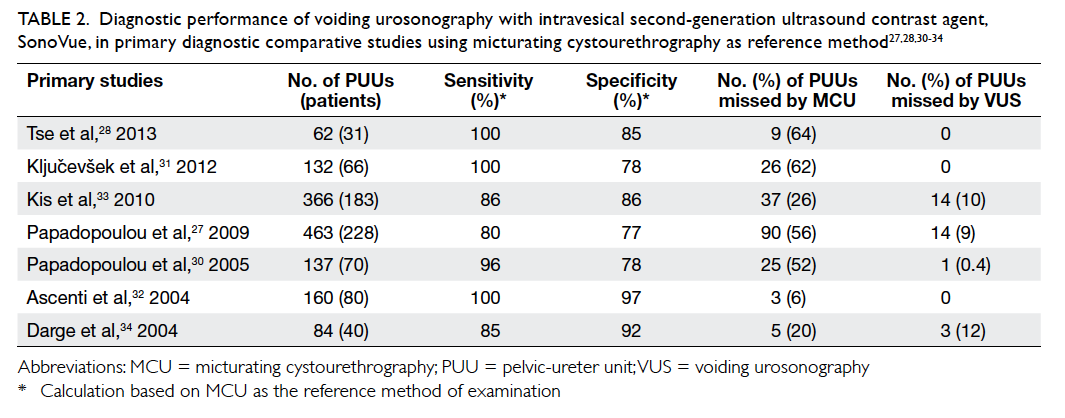
Table 2. Diagnostic performance of voiding urosonography with intravesical second-generation ultrasound contrast agent, SonoVue, in primary diagnostic comparative studies using micturating cystourethrography as reference method27 28 30 31 32 33 34
Reliability
Sonographic techniques entail specialised
scanning and interpretation skills, and are considered to be
operator-dependent. According to a recent review by Prasad and
Cheng,35 the techniques of
ceVUS remained operator-dependent and required highly skilled
sonographers. Hence, our pilot study had specifically examined the
reliability of ceVUS by independent review of the saved images and
cine video clips of all the ceVUS examinations by two operators
after study completion. Perfect inter-observer agreement was
achieved, with Cohen’s Kappa statistics of 1.0 (P<0.001).
Therefore, with harmonic imaging and modified ultrasound
techniques, ceVUS has good reliability in diagnosing
vesicoureteric reflux in children.
Safety profile and feasibility
Voiding urosonography involves intravesical
application of ultrasound contrast and continuous sonographic
examination. The ultrasound contrast is not administered
intravenously and, hence, systemic complications are extremely
rare. In a recent European territory-wide questionnaire-based
survey,36 there were no allergic reactions or systemic complications
related to SonoVue in 5079 paediatric ceVUS examinations performed
in 45 European centres.
Only few minor complications related to catheterization were
encountered. Our pilot study also confirmed the high safety
profile of SonoVue-enhanced VUS. No complications related to the
contrast agent, catheterization, or infection were noticed.28 Apart from high safety profile, technical
feasibility is another advantage of ceVUS. As mentioned earlier,
ceVUS is technically analogous with MCU, except that it involves
sonographic examination of the urinary tract instead of
fluoroscopy. In terms of manpower, a ceVUS examination requires a
radiologist and two sonographers, which is similar to that for
MCU. Therefore, the examination duration and manpower involved in
ceVUS are similar to that for MCU.28
Finally, the dosage of SonoVue in each ceVUS examination is 0.8 mL
to 1 mL, which is adequate for at least three cycles of filling
and voiding phases. Therefore, a vial of SonoVue can be shared
among several patients in each session, thus, allowing effective
usage of the contrast agent.28
Radiation protection
With the use of ultrasound examination in
ceVUS, many clinical indications of MCU can be performed by ceVUS.
The ceVUS had been incorporated in the joint guideline for
urological examination by the European Society of Urogenital
Radiology (ESUR) and European Society of Paediatric Radiology
(ESPR) in 2007.37 The
indications of ceVUS include follow-up examination of known
vesicoureteric reflux, investigation of UTI in girls, as well as
screening for familial history of vesicoureteric reflux and fetal
hydronephrosis. With the application of urethral imaging in ceVUS,
examination of the urethra is technically feasible (Fig
3). Duran et al38
revealed that diagnosis of urethral pathologies, such as posterior
urethral valve, diverticulum of prostatic utricle, and anterior
urethral stricture could be achieved by using interscrotal and
transperineal approaches in boys. The application of ceVUS has
extended to investigation of UTI in boys and urethral imaging in
genitogram in the ESUR and ESPR guideline 2012.39
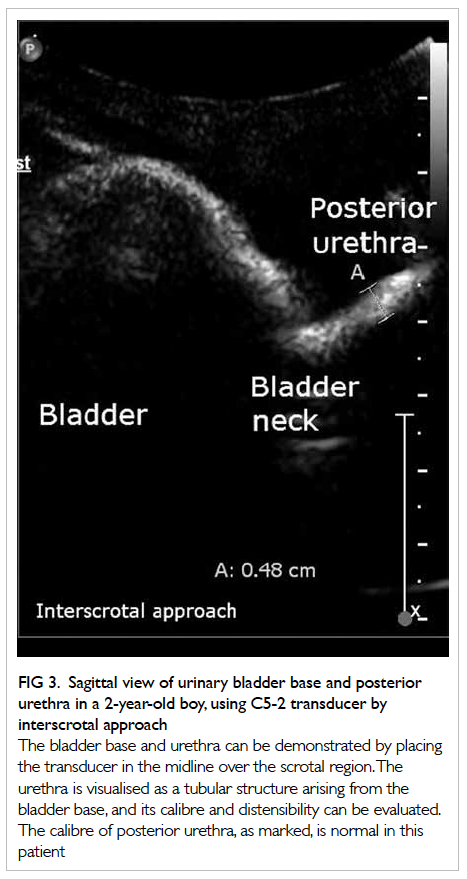
Figure 3. Sagittal view of urinary bladder base and posterior urethra in a 2-year-old boy, using C5-2 transducer by interscrotal approach
Micturating cystourethrography is by far
the most common fluoroscopic examination performed in children,
accounting for 40% of the examinations.40
In a recent study on radiation dose of paediatric MCU by Sulieman
et al,41 the mean entrance
surface dose for MCU with positive reflux was 1.45 mGy, and
negative reflux was 1.05 mGy. As gonads were inside the radiation
field during the examination, there was a higher organ equivalent
dose to ovaries (0.44 mSv) and testes (0.33 mSv) than to thyroid
(0.006 mSv). The estimated risks of malignancy of ovaries and
testes were 4.4 x 10-7 and 3.3 x 10-7,
respectively. Although the risks are small, cumulative radiation
exposure and radiation to developing gonads are inevitable in
patients with positive reflux who require repeat examinations
for follow-up. Taking 20% as the positive rate of MCU, a large
proportion of patients and parents are exposed to ionising
radiation for ruling out vesicoureteric reflux. As ceVUS can
provide most of the diagnostic information offered by MCU, it can
be a valid radiation-free alternative to MCU. According to
Giordano et al,42
radiation dose has significantly reduced since the application of
ceVUS in routine clinical practice.
Limitations of contrast-enhanced voiding
urosonography
As discussed in the previous section, the
acoustic shadowing produced by the high concentration of
ultrasound contrast can obscure the retrovesical region and, thus,
decrease the sensitivity of ceVUS in detecting grade I reflux.29 This is remedied by dilution of ultrasound
contrast by continuous saline infusion, and is best assessed
during the second cyclical examination.28
Besides, ceVUS has limitation in those examinations that require
detailed anatomical assessment, such as in evaluation of
recto-urethral fistula in distal loopogram in neonates with
anorectal malformation.28
However, the majority of indications of MCU, as mentioned in
previous sections, can also be performed by ceVUS.
Conclusion
In the era of heightened radiation
awareness and protection, radiation doses to infants and children
should be kept as low as reasonably achievable. Contrast-enhanced
voiding urosonography using intravesical ultrasound contrast agent
should be introduced as a valid alternative diagnostic modality
for detecting vesicoureteric reflux, based on its radiation-free,
highly efficacious, reliable, and safe characteristics43; MCU can be reserved for patients requiring
detailed anatomical assessment.
Declaration
No conflicts of interest were declared by
the authors.
References
1. Sargent MA. What is the normal
prevalence of vesicoureteric reflux? Pediatr Radiol
2000;30:587-93. CrossRef
2. Fong KW, Wong SN. Symptomatic
urinary tract infection in children: experience in a regional
hospital in Hong Kong. Hong Kong J Paediatr 2004;9:30-6.
3. Koff SA, Wagner TT, Jayanthi VR.
The relationship among dysfunctional elimination syndromes,
primary vesicoureteral reflux and urinary tract infections in
children. J Urol 1998;160:1019-22. CrossRef
4. Bailey RR. The relationship of
vesico-ureteric reflux to urinary tract infection and chronic
pyelonephritis—reflux nephropathy. Clin Nephrol 1973;1:132-41.
5. Ditchfield MR, De Campo JF, Cook
DJ, et al. Vesicoureteral reflux: an accurate predictor of acute
pyelonephritis in childhood urinary tract infection? Radiology
1994;190:413-5.
6. Pennesi M, Travan L, Peratoner
L, et al. North East Italy Prophylaxis in VUR study group. Is
antibiotics prophylaxis in children with vesicoureteral reflux
effective in preventing pyelonephritis and renal scars? A
randomized, controlled trial. Pediatrics 2008;121:e1489-94. CrossRef
7. Subcommittee on Urinary Tract
Infection, Steering Committee on Quality Improvement and
Management, Roberts KB. Urinary tract infection: clinical practice
guideline for the diagnosis and management of the initial UTI in
febrile infants and children 2 to 24 months. Pediatrics
2011;128:595-610. CrossRef
8. Lebowitz RL, Olbing H,
Parkkulainen KV, Smellie JM, Tamminen-Mobius TE. International
system of radiographic grading of vesicoureteric reflux.
International Reflux Study in Children. Pediatr Radiol
1985;15:105-9. CrossRef
9. Arsanjani A, Alagiri M.
Identification of filling versus voiding reflux as predictor of
clinical outcome. Urology 2007;70:351-4. CrossRef
10. Perisinakis K, Raissaki M,
Damilakis J, Stratakis J, Neratzoulakis J, Gourtsoyiannis N.
Fluoroscopy-controlled voiding cystourethrography in infants and
children: are the radiation risks trivial? Eur Radiol
2006;16:846-51. CrossRef
11. Miglioretti DL, Johnson E,
Williams A, et al. The use of computed tomography in pediatrics
and the associated radiation exposure and estimated cancer risk.
JAMA Pediatr 2013;167:700-7. CrossRef
12. Sukan A, Bayazit AK, Kibar M,
et al. Comparison of direct radionuclide cystography and voiding
direct cystography in the detection of vesicoureteral reflux. Ann
Nucl Med 2003;17:549-53. CrossRef
13. Unver T, Alpay H, Biyikli NK,
Ones T. Comparison of direct radionuclide cystography and voiding
cystourethrography in detecting vesicoureteral reflux. Pediatr Int
2006;48:287-91. CrossRef
14. Fettich J, Colarinha P,
Fischer S, et al. Guidelines for direct radionuclide cystography
in children. Eur J Nucl Med Mol Imaging 2003;30:39-44. CrossRef
15. Medina LS, Aquirre E, Altman
NR. Vesicoureteral reflux imaging in children: comparative cost
analysis. Acad Radiol 2003;10:139-44. CrossRef
16. Atala A, Wible JH, Share JC,
Carr MC, Retik AB, Mandell J. Sonography with sonicated albumin in
the detection of vesicoureteral reflux. J Urol 1993;150:756-8.
17. Valentini AL, De Gaetano AM,
Destito C, Marino V, Minordi LM, Marano P. The accuracy of voiding
urosonography in detecting vesico-ureteral reflux: a summary of
existing data. Eur J Pediatr 2002;161:380-4. CrossRef
18. Radmayr C, Klauser A, Pallwein
L, Zurnedden D, Bartsch G, Frauscher F. Contrast enhanced reflux
sonography in children: a comparison to standard radiological
imaging. J Urol 2002;167:1428-30. CrossRef
19. Escape I, Martinez J, Bastart
F, Solduga C, Sala P. Usefulness of echocystography in the study
of vesicoureteral reflux. J Ultrasound Med 2001;20:145-9.
20. Bosio M. Cystosonography with
echocontrast: a new imaging modality to detect vesicoureteric
reflux in children. Pediatr Radiol 1998;28:250-5. CrossRef
21. Darge K, Troeger J.
Vesicoureteral reflux grading in contrast-enhanced voiding
urosonography. Eur J Radiol 2002;43:122-8. CrossRef
22. Tranquart F, Grenier N, Eder
V, Pourcelot L. Clinical use of ultrasound tissue harmonic
imaging. Ultrasound Med Biol 1999;25:889-94. CrossRef
23. Fritzsch T, Schlief R.
Levovist. Drugs Fut 1995;20:1224-7.
24. Schneider M. SonoVue, a new
ultrasound contrast agent. Eur Radiol 1999;9 Suppl 3:347S-348S. CrossRef
25. Rossling G. Physico-chemical
properties of Levovist. Proceedings of the 2nd European Meeting on
Sonographic Diagnosis of Vesicoureteral Reflux; 2000 Mar;
Heidelberg, Germany.
26. Shapiro RS, Wagreich J,
Parsons RB, Stancato-Pasik A, Yeh HC, Lao R. Tissue harmonic
imaging sonography: evaluation of image quality compared with
conventional sonography. Am J Roentgenol 1998;171:1203-6. CrossRef
27. Papadopoulou F, Anthopoulou A,
Siomou E, Efremidis S, Tsamboulas C, Darge K. Harmonic voiding
urosonography with a second-generation contrast agent for the
diagnosis of vesicoureteral reflux. Pediatr Radiol 2009;39:239-44. CrossRef
28. Tse KS, Wong LS, Fan TW, et
al. New radiation-free era in reflux imaging for paediatric
urinary tract infection (UTI): voiding urosonography with
intravesical ultrasound contrast—first local pilot study. Paper
presented at 2013 Hospital Authority Convention; 2013 May 15-16;
Hong Kong.
29. Darge K. Voiding urosonography
with US contrast agents for the diagnosis of vesicoureteric reflux
in children. II. Comparison with radiological examinations.
Pediatr Radiol 2008;38:54-63; quiz 126-7. CrossRef
30. Papadopoulou F, Katzioti F,
Arkoumani E, et al. Voiding urosonography harmonic imaging with
2nd generation contrast agent for the diagnosis of reflux
[abstract]. Pediatr Radiol 2005;35:130S.
31. Ključevšek D, Battelino N,
Tomažič M, Kersnik Levart T. A comparison of echo-enhanced voiding
urosonography with X-ray voiding cystourethrography in the first
year of life. Acta Paediatr 2012;101:e235-9. CrossRef
32. Ascenti G, Zimbaro G,
Mazziotti S, et al. Harmonic US imaging of vesicoureteric reflux
in children: usefulness of a second generation US contrast agent.
Pediatr Radiol 2004;34:481-7. CrossRef
33. Kis E, Nyitrai A, Varkonyi I,
et al. Voiding urosonography with second-generation contrast agent
versus voiding cystourethrography. Pediatr Nephrol
2010;25:2289-93. CrossRef
34. Darge K, Beer M, Gordjani N,
Riedmiller H. Contrastenhanced voiding urosonography with the use
of a 2nd generation US contrast medium: preliminary results.
Pediatr Radiol 2004;34:97S.
35. Prasad MM, Cheng EY.
Radiographic evaluation of children with febrile urinary tract
infection: bottom-up, top-down, or none of the above? Adv Urol
2012;2012:716739.
36. Riccabona M. Application of a
second-generation US contrast agent in infants and children—a
European questionnaire-based survey. Pediatr Radiol 2012;42:1471-
80. CrossRef
37. Riccabona M, Avni FE, Blickman
JG, et al. Imaging recommendations in paediatric uroradiology:
minutes of the ESPR workgroup session on urinary tract infection,
fetal hydronephrosis, urinary tract ultrasonography and voiding
cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol
2008;38:138-45. CrossRef
38. Duran C, Valera A, Alguersuari
A, et al. Voiding urosonography: the study of the urethra is no
longer a limitation of the technique. Pediatr Radiol
2009;39:124-31. CrossRef
39. Riccabona M, Avni FE, Damasio
MB, et al. ESPR Uroradiology Task Force and ESUR Paediatric
Working Group—Imaging recommendations in paediatric
uroradiology, part V: childhood cystic kidney disease, childhood
renal transplantation and contrast-enhanced ultrasonography in
children. Pediatr Radiol 2012;42:1275-83. CrossRef
40. Schneider K, Kruger-Stollfuss
I, Ernst G, Kohn NM. Paediatric fluoroscopy—a survey of children’s
hospitals in Europe. I. Staffing, frequency of fluoroscopic
procedures and investigation technique. Pediatr Radiol
2001;31:238-46. CrossRef
41. Sulieman A, Theodorou K,
Vlychou M, et al. Radiation dose measurement and risk estimation
for paediatric patients undergoing micturating cystourethrography.
Br J Radiol 2007;80:731-7. CrossRef
42. Giordano M, Marzolla R, Puteo
F, Scianaro L, Caringella DA, Depalo T. Voiding urosonography as
first step in the diagnosis of vesicoureteral reflux in children:
a clinical experience. Pediatr Radiol 2007;37:674-7. CrossRef
43. Wong LS, Tse KS, Fan TW, et
al. Voiding urosonography with second-generation ultrasound
contrast versus micturating cystourethrography in the diagnosis of
vesicoureteric reflux. Eur J Pediatr 2014 Mar 23. Epub ahead of
print. CrossRef