Hong Kong Med J 2014 Aug;20(4):350.e3–4
DOI: 10.12809/hkmj134046
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Diffuse xanthomatous eruption
HF Cheng, MB, BS, MRCP (UK); William YM Tang, FRCP (Edin), FHKAM (Medicine); KC Lee, FRACPath, FHKAM (Pathology)
DERM 1 Skin Specialists Centre, Room 1102, Champion Building,
301-309 Nathan Road, Kowloon, Hong Kong
Corresponding author: Dr HF Cheng (chf@doctor.com)
A 37-year-old non-smoker with no history of drug
allergy and history of childhood asthma presented
with itchy rash over his back for 1 month, which
progressed to involve his limbs and both axillae,
in January 2013. The patient was not taking any
medication apart from health supplements. He did
not have any complaints of joint pain or fever. He was
seen by a general practitioner who managed the rash
as viral infection. Family history of hyperlipidaemia
was negative. On examination, the patient was an
obese man with body mass index of 32 kg/m2, blood
pressure of 152/89 mm Hg, and pulse rate of 100
beats/min. There were widespread, reddish-yellow
papular eruptions over both sides of the trunk and
limbs, sparing the face, scalp, oral cavity, and ears
(Fig 1). There were no scales, vesicles, pus formation,
or erosions. The size of the lesions ranged from to
0.1 cm to 0.4 cm (Fig 2). There was no corneal arcus,
regional lymphadenopathy, abdominal organomegaly
or arthropathy. A skin biopsy of the lesion showed
features of eruptive xanthoma (Figs 3 and 4). Fasting
blood examination showed markedly elevated levels
of total cholesterol (12.1 mmol/L), serum triglycerides (40.36 mmol/L), and plasma glucose (14.7 mmol/L).
Thus, he was urgently referred to an endocrinologist.
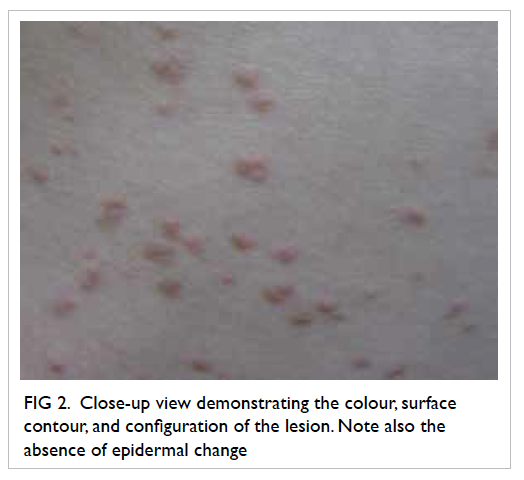
Figure 2. Close-up view demonstrating the colour, surface contour, and configuration of the lesion. Note also the absence of epidermal change
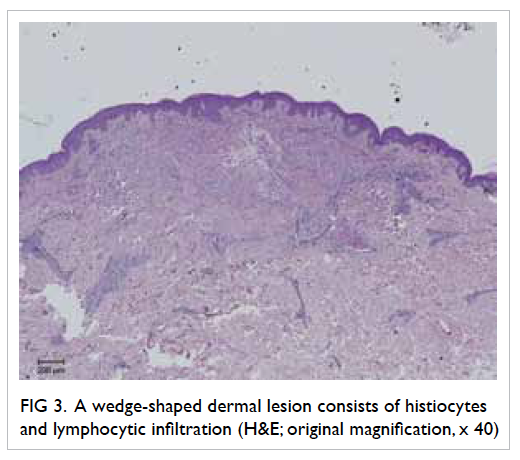
Figure 3. A wedge-shaped dermal lesion consists of histiocytes and lymphocytic infiltration (H&E; original magnification, x 40)
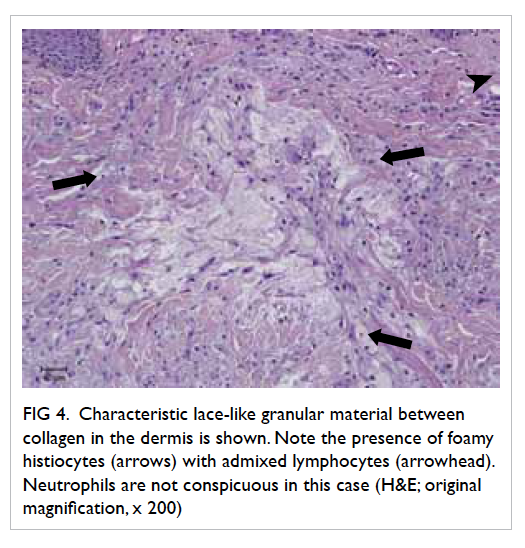
Figure 4. Characteristic lace-like granular material between collagen in the dermis is shown. Note the presence of foamy histiocytes (arrows) with admixed lymphocytes (arrowhead). Neutrophils are not conspicuous in this case (H&E; original magnification, x 200)
Discussion
Eruptive xanthoma is a benign lesion and patients
usually consult because of itchiness or for
cosmetic reasons. Morbidity arises from metabolic
complications such as acute pancreatitis or myocardial
infarction. The macroscopic lesions arise from
phagocytosis in the dermis of plasma lipoproteins
that leak from capillaries.1 Laboratory workup is
mandatory to exclude diabetes, nephrotic syndrome,
or hypothyroidism. Screening of family members is essential as genetic factors may contribute in the
development of the condition.2 Eruptive xanthoma
can occur in individuals with normal lipid levels.3
Under these circumstances, it is prudent to exclude
occult malignancy (eg lymphoproliferative disorders
and monoclonal paraproteinaemia) or infections (eg
human immunodeficiency virus infection).4 Solitary
lesions necessitate enquiry about previous local
trauma, dermatoses, or surgical operation for Köbner
phenomenon might have happened.
Differential diagnoses include eruptive
xanthogranuloma, xanthoma disseminatum,
and Langerhans cell histiocytosis (LCH).
Xanthogranuloma usually arises in the head-and-neck
regions of children. It is mostly a solitary,
small-sized papule or nodule. Ophthalmologic
evaluation is indicated if ocular involvement is
suspected. Histopathology shows collection of
lipidised histiocytes, inflammatory infiltrates, and
Touton giant cells in the dermis. Known as non-LCH, xanthoma disseminatum is a non-familial
histiocytic disorder. Mucocutaneous as well as
systemic involvement has been reported. It shares
similar histopathological features with eruptive
xanthogranuloma but eosinophils may be absent, and
Touton giant cells may be inconspicuous. Treatment, by far, is unsatisfactory. Langerhans cell histiocytosis
comprises a spectrum of disorders with varied clinical
manifestations including cutaneous involvement.
Confirmation of diagnosis rests on histopathology.
Within the lesion is dense infiltration by abnormal
Langerhans cells which are characterised by their
folded nuclei. Presence of a mixed inflammatory
infiltrate with eosinophils in the background forms
the classical picture of LCH. The Langerhans cells
in LCH differ from the typical Langerhans cells by
the lack of dendritic cell processes, and this feature
is best demonstrated by CD1a immunostaining. All
these differential diagnoses lack the characteristic
deposits of lace-like material between collagen seen
in eruptive xanthoma.
Gradual resolution of the cutaneous lesions is
usually expected upon normalisation of lipid level in
patients with eruptive xanthoma. En-bloc surgical
excision or carbon dioxide laser vaporisation is equally
practical, depending on the extent of the disease. The
use of carbon dioxide laser has been reported in a skin
phototype VI patient with xanthoma disseminatum
with cosmetically acceptable post-inflammatory
hyperpigmentation.5 Finally, referral to a physician
is needed in patients with concomitant metabolic
syndrome.
References
1. Massengale WT, Nesbitt LT Jr. Xanthomas. In: Bolognia
JL, Jorizzo JL, Rapini RP, editors. Dermatology. Vol 2. 2nd
ed. London, England: Mosby Elsevier; 2008: 1411-9.
2. Pickens S, Farber G, Mosadegh M. Eruptive xanthoma: a
case report. Cutis 2012;89:141-4.
3. Williford PM, White WL, Jorizzo JL, Greer K. The
spectrum of normolipemic plane xanthoma. Am J
Dermatopathol 1993;15:572-5. CrossRef
4. Ramsay HM, Garraido MC, Smith AG. Normolipaemic
xanthomas in association with human immunodeficiency
virus infection. Br J Dermatol 2000;142:571-3. CrossRef
5. Carpo BG, Grevelink SV, Brady S, Gellis S, Grevelink JM.
Treatment of cutaneous lesions of xanthoma disseminatum
with a CO2 laser. Dermatol Surg 1999;25:751-4. CrossRef


