Hong Kong Med J 2014;20:265.e1–2 | Number 3, June 2014
DOI: 10.12809/hkmj133987
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Amelanotic melanoma masquerading as a pyogenic
granuloma: caution warranted
Noah LW So, MB, BS; CF Chan, MB, BS, FHKAM
(Orthopaedic Surgery); Kenneth WY Ho, MB, BS, FHKAM (Orthopaedic
Surgery); YL Lam, MB, ChB, FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and
Traumatology, Queen Mary Hospital, 102 Pokfulam Road, Hong Kong
Corresponding author: Dr Noah LW So (noahlwso@gmail.com)
Case
In April 2012, a 69-year-old Chinese woman
complained of a non-healing raised lesion over the lateral aspect
of her left fifth toe which had developed 2 years earlier. It
appeared to have started as a minor abrasion after wearing
ill-fitting shoes. A painless swelling then developed over that
site with occasional friction-induced bleeding. She attended
several podiatry treatment sessions and tried applying topical
medications such as silver nitrate. The lesion did not resolve,
and increased in size and eventually developed into a pink nodule.
Apart from hypercholesterolaemia, the patient was an otherwise
healthy non-smoker and non-drinker who enjoyed sunbathing on the
beach in her youth, often spending half a day under the sun.
On physical examination, a 1 cm x 1 cm
round and dull red nodule with superficial ulceration was noted on
the lateral aspect of the left fifth toe. There were no signs of
infection and no contact bleeding was evident (Fig).
Given the history of minor trauma, tendency to bleed with minor
friction and the appearance of the lesion, pyogenic granuloma was
the main differential diagnosis. Owing to failure of repeated
conservative treatment, excision of the lesion was performed.
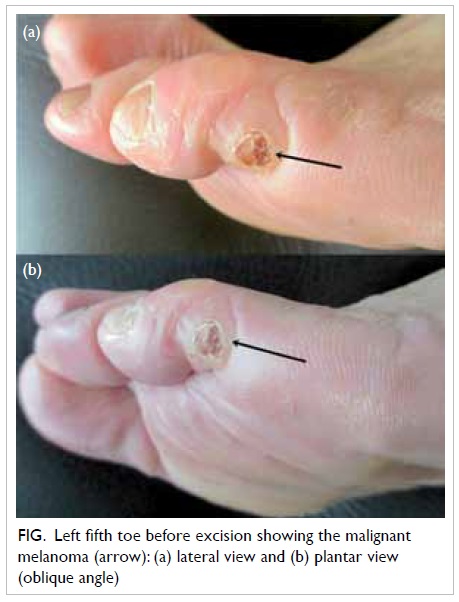
Figure. Left fifth toe before excision showing the malignant melanoma (arrow): (a) lateral view and (b) plantar view (oblique angle)
Histology revealed it to be a malignant
melanoma; no melanin pigment was detected but the tumour cells
were positive for melanocytic markers. A staging positron emission
tomography–computed tomography showed no metastasis. A wide
resection involving ray amputation of the 4th and 5th toes was
performed to ensure a clear resection margin.
Discussion
Amelanotic melanoma is reported to account
for about 1.8% to 8.1% of all melanomas.1
Cheung et al2 defined
amelanotic melanoma as being unsuspected clinically and with
melanin in less than 5% of the tumour cells. Because the diagnosis
was not suspected clinically, he noted that excisional biopsies
were seldom performed, and that if undertaken, transection of the
melanoma was common. In their database of 1170 patients, McClain
et al3 found that red
melanomas accounted for 3.9% of all such malignancies and up to
70% of those that were amelanotic. Regarding prognosis, their
review found no significant difference between red amelanotic
melanomas and pigmented melanomas in terms of disease-free
survival, overall survival, metastasis, and recurrence. In other
words, the mortality of red amelanotic melanomas appeared
comparable to that of pigmented melanoma.
In our patient, the most notable risk
factor for developing melanoma was prolonged sunlight exposure but
such a history may be missed if the diagnosis is not suspected.
Amelanotic melanomas appear clinically indistinguishable from
pyogenic granulomas. We therefore caution all our readers to the
possibility of amelanotic melanoma presenting as seemingly benign
red lesions. Whilst uncommon in China (age-standardised incidence
of 0.2 per 100 000 population and year),4
melanomas are highly malignant; both observation without
investigation and excision without undertaking histology can delay
the diagnosis with potentially disastrous consequences. The
mnemonic ‘ABCD’ summarises features suggesting melanoma:
Asymmetry, irregular Border, uneven Colour, Diameter of >6 mm.4 The mnemonic RRR (Red,
Raised lesion, Recent change3)
is proposed additionally for the diagnosis of red amelanotic
melanomas. We recommend that for such red lesions of uncertain
nature, referral to specialists experienced in managing melanomas
is warranted.
References
1. Koch SE, Lange JR. Amelanotic
melanoma: the great masquerader. J Am Acad Dermatol 2000;42:731-4. CrossRef
2. Cheung WL, Patel RR, Leonard A,
Firoz B, Meehan SA. Amelanotic melanoma: a detailed morphologic
analysis with clinicopathologic correlation of 75 cases. J Cutan
Pathol 2012;39;33-9. CrossRef
3. McClain SE, Mayo KB, Shada AL,
Smolkin ME, Patterson JW, Slingluff CL Jr. Amelanotic melanomas
presenting as red skin lesions: a diagnostic challenge with
potentially lethal consequences. Int J Dermatol 2012;51:420-6. CrossRef
4. LeBoit PE, Burg G, Weedon D,
Sarasin A, editors. Pathology and genetics of skin tumours (IARC
WHO Classification of Tumours). Lyon: IARC Press; 2006.

