Hong Kong Med J 2014;20:156–7 | Number 2, April 2014
DOI: 10.12809/hkmj133946
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Malignant presternal goitre
TL Chow, FRCS (Edin), FHKAM (Surgery)1;
Wilson WY Kwan, MRCS1;
Joyce YH Hui, FRCR, FHKAM (Radiology)2
1 Department of Surgery, United Christian Hospital, Kwun Tong, Hong Kong
2 Department of Diagnostic Radiology and Organ Imaging, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr TL Chow (tamlinc@yahoo.com)
Abstract
Goitres usually enlarge and descend caudad into the
substernal space and are not palpable. We report on
a patient whose goitre spread downward but anterior
to the sternum. The thyroid mass was subsequently
removed and was proven to be a papillary thyroid
carcinoma. The mechanism by which a presternal
goitre develops is probably due to invasion and
erosion of the strap muscles and the cervical linea
alba. The clinical implication of this presentation is
complete extirpation of the presternal goitre with a
cuff of the strap muscles.
Introduction
When goitres enlarge, they can extend beyond the
boundary of the neck. Since the thyroid gland resides
beneath the pretracheal fascia and the strap muscles
and their attachments are connected to the top of
the manubrium, goitres usually migrate down into
the superior mediastinum. Substernal goitres can
occur in 8.4% patients undergoing thyroidectomy.1
We have treated a patient with a malignant
goitre, which spread exceptionally to the presternal
region. Herein we report this unusual presentation
of an extra-cervical extension of a thyroid mass and
stress its association with malignancy.
Case report
A 50-year-old man presented to our out-patient
clinic in January 2012 with an enlarging anterior
neck mass for the past 3 years. He experienced mild
pain which prompted him to seek medical advice. A
dumb-bell–shaped mass was found over his anterior
neck. The upper portion of the mass was about
4.5 cm in diameter and located at the suprasternal
region. The lower portion was 3.5 cm in diameter and
resided anterior to the sternum, about 3 cm from the
upper border of manubrium (Fig 1). The whole mass
migrated upward when patient swallowed which
signified its thyroid origin.
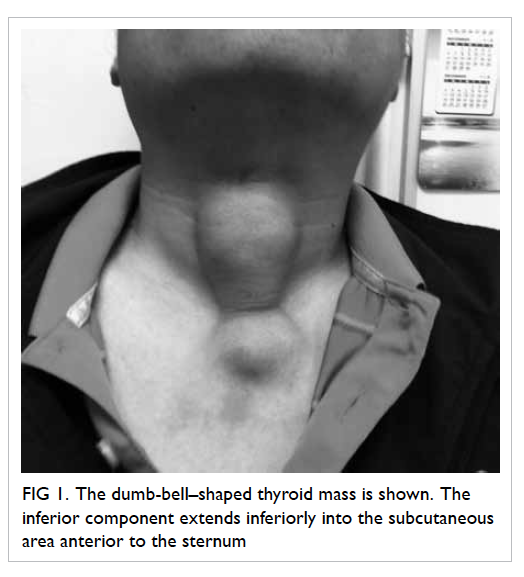
Figure 1. The dumb-bell–shaped thyroid mass is shown. The inferior component extends inferiorly into the subcutaneous area anterior to the sternum
Thyroid function test results were normal.
Computed tomography 4 weeks later showed an
isthmic thyroid mass (3.7 x 2.8 x 3.4 cm) containing
micro- and macro-calcifications. The lower
component of the dumb-bell–shaped mass was
anterior to the sternum (Fig 2), and there was no
substernal extension.
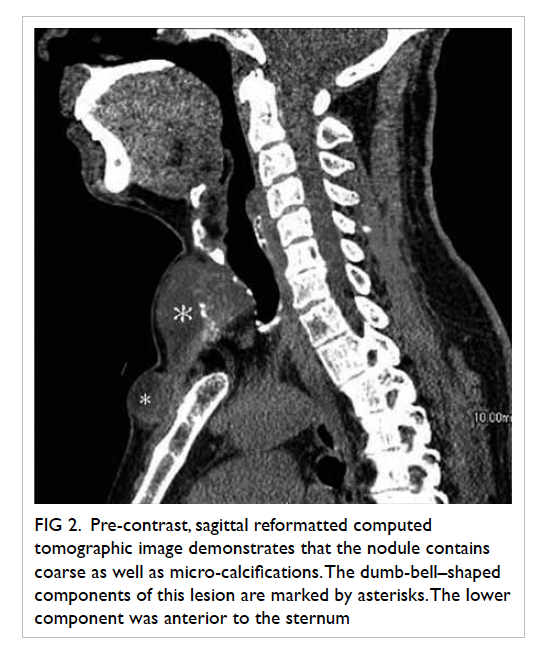
Figure 2. Pre-contrast, sagittal reformatted computed tomographic image demonstrates that the nodule contains coarse as well as micro-calcifications. The dumb-bell–shaped components of this lesion are marked by asterisks. The lower component was anterior to the sternum
The patient was very keen to undergo surgery,
but he declined fine-needle aspiration of the mass. Total thyroidectomy with a collar incision was
performed 3 weeks later. The 4.5 x 5 cm isthmic
thyroid mass passed through the midline fascia
(between the strap muscles) and reached the
presternal area. The muscle attachments of the
strap muscles were at their normal positions on
the manubrium. Total thyroidectomy including the
entire dumb-bell mass en bloc with surrounding
strap muscles and deep fascia was performed.
Histopathology revealed papillary thyroid
carcinoma in both the superior and inferior
components of the dumb-bell mass. The resection
margin was clear. Postoperative radioactive iodine
ablation 80mCi was given 5 months after the initial presentation (about 10 weeks after surgery). The
thyroglobulin level during thyroxine withdrawal
was <1.0 μg/L, and there was no evidence of tumour
recurrence.
Discussion
Substernal goitre is uncommon. Presternal goitre is
even rarer. We searched the literature in MEDLINE
and came across only two reported cases. The first
reported by Raman and Nair2 in 1999 was a papillary
thyroid carcinoma. The second described by Brilli
et al3 in 2007 was a benign nodular goitre. We
report this third case of a presternal goitre, which
was also a papillary thyroid carcinoma. Therefore,
if a thyroid mass spreads presternally, malignancy
should be suspected. In our patient, malignancy was
not suspected initially due to little knowledge about
presternal goitres at that time. Therefore, an intra-operative
frozen section was not obtained. We now
realise the high risk of malignancy for this entity, and
that preoperative fine-needle aspiration cytology or
intra-operative frozen section examination should
be performed in all such cases, and better informed
consent regarding surgery should be obtained. Moreover, the extent of operation can also be more
appropriately determined. In addition, preoperative
imaging yielding micro-calcification in the goitre as
well as presternal extension, or both should heighten
the possibility of an underlying papillary carcinoma.
The mechanism resulting in the more common
substernal goitre was speculated to the negative
intrathoracic pressure during inspiration and the
downward pull of gravity.4 By contrast, presternal
migration of a malignant thyroid mass (as in our
patient) was probably due to tumour erosion of
the cervical linea alba between the strap muscles.
Prompt investigation with imaging and fine-needle
aspiration therefore seems imperative to make
an accurate diagnosis and offer early therapy.
Such patients should be advised to undergo total
thyroidectomy. Notably, the thyroid masses should
be removed en bloc with the adjacent strap muscles
in order to achieve a clear resection margin.
Presternal goitre is rare and likely to represent
thyroid malignancy eroding the cervical linea alba
and strap muscles. Total thyroidectomy including a
cuff of strap muscles encircling the mass should be
performed to ensure complete tumour extirpation.
References
1. Chow TL, Chan TT, Suen DT, Chu DW, Lam SH. Surgical management of substernal goitre: local experience. Hong Kong Med J 2005;11:360-5.
2. Raman A, Nair A. Presternal extension of a malignant thyroid swelling. Aust N Z J Surg 1999;69:241-2. CrossRef
3. Brilli L, Guarino E, Ghezzi M, Carli AF, Occhini R, Pacini F. Multinodular goiter of unusual shape and location. Thyroid 2007;17:693-4. CrossRef
4. Singh B, Lucente FE, Shaha AR. Substernal goiter: a clinical review. Am J Otolaryngol 1994;15:409-16. CrossRef

