© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
Are your kidneys OK? Detect early to protect kidney health
Joseph A Vassalotti, MD, PhD1,2 #; Anna Francis, MD, PhD3 #; Augusto Cesar Soares Dos Santos Jr, MD, PhD4,5; Ricardo Correa-Rotter, MD, PhD6; Dina Abdellatif, MD, PhD7; Li-Li Hsiao, MD, PhD8; Stefanos Roumeliotis, MD, PhD9; Agnes Haris, MD, PhD10; Latha A Kumaraswami, MD, PhD11; Siu-Fai Lui, MD, PhD12 Alessandro Balducci, MD, PhD13; Vassilios Liakopoulos, MD, PhD8; for the World Kidney Day Joint Steering Committee
1 Mount Sinai Hospital, Department of Medicine-Renal Medicine, New York, New York, United States
2 National Kidney Foundation, Inc, New York, New York, United States
3 Queensland Children’s Hospital, Department of Nephrology, South Brisbane, Queensland, Australia
4 Faculdade Ciencias Medicas de Minas Gerais, Brazil
5 Hospital das Clinicas, Ebserh, Universidade Federal de Minas Gerais, Brazil
6 Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico
7 Department of Nephrology, Cairo University Hospital, Cairo, Egypt
8 Renal Division, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts, United States
9 Second Department of Nephrology, American Hellenic Educational Progressive Association (AHEPA) University Hospital Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece
10 Nephrology Department, Péterfy Hospital, Budapest, Hungary
11 Tamilnad Kidney Research (TANKER) Foundation, Chennai, India
12 Division of Health System, Policy and Management, The Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China
13 Italian Kidney Foundation, Rome, Italy
# Equal contribution
Corresponding author: Dr Stefanos Roumeliotis (st_roumeliotis@hotmail.com)
Abstract
Early identification of kidney disease can protect
kidney health, prevent disease progression and
related complications, reduce cardiovascular risk,
and decrease mortality. We must ask, “Are your
kidneys OK?” by using serum creatinine to estimate
kidney function and urine albumin to assess for
kidney and endothelial damage. Evaluation of the
causes and risk factors for chronic kidney disease
includes testing for diabetes and measuring blood
pressure and body mass index. This World Kidney
Day, we assert that case-finding in high-risk
populations—or even population-level screening—can decrease the global burden of kidney disease. Early-stage chronic kidney disease is asymptomatic,
simple to test for, and recent paradigm-shifting
treatments (eg, sodium-glucose co-transporter-2
inhibitors) dramatically improve outcomes and
strengthen the cost–benefit case for screening or
case-finding programmes. Despite these factors,
numerous barriers exist, including resource
allocation, healthcare funding, infrastructure, and
healthcare professional and public awareness of
kidney disease. Coordinated efforts by major kidney
non-governmental organisations to prioritise the
kidney health agenda for governments—and to align
early detection efforts with existing programmes—will maximise efficiencies.
Introduction
Timely treatment is the primary strategy to protect
kidney health, prevent disease progression and
related complications, reduce cardiovascular
risk, and prevent premature kidney-related and
cardiovascular mortality.1 2 3 International population
assessments show low awareness and detection
of kidney disease, along with substantial gaps in
treatment.2 People with kidney failure universally
express a preference for having been diagnosed earlier
in their disease trajectory, which would allow more time for educational, lifestyle, and pharmacological
interventions.4 Therefore, increasing knowledge and
implementing sustainable solutions for the early
detection of kidney disease to protect kidney health
are public health priorities.2 3
Epidemiology and complications of kidney
disease
Chronic kidney disease (CKD) is prevalent, affecting
10% of the global population—over 700 million
people.5 Nearly 80% of people with CKD live in low-income countries (LICs) and lower-middle-income
countries (LMICs), and approximately one-third of
the known affected population resides in China and
India alone.5 6 The prevalence of CKD increased by
33% between 1990 and 2017.5 This rising trend is
driven by population growth, ageing, and the obesity
epidemic, which contribute to higher rates of two
major CKD risk factors: type 2 diabetes mellitus
(T2DM) and hypertension. Additionally, risk factors
beyond cardiometabolic conditions add to the
growing burden of kidney disease. These include
social deprivation, pregnancy-related acute kidney
injury, preterm birth, and escalating environmental
threats such as infections, toxins, climate change,
and air pollution.5 7 These threats disproportionately
affect people in LICs and LMICs.8
Undetected and untreated CKD is more likely
to progress to kidney failure and cause premature
morbidity and mortality. Globally, more people
died in 2019 of cardiovascular disease attributed to
reduced kidney function (1.7 million people) than
the number who died of kidney disease alone (1.4
million).5 Chronic kidney disease is expected to
become the fifth most common cause of years of life
lost by 2040, surpassing T2DM, Alzheimer’s disease,
and road injuries.9 The rising mortality associated
with kidney disease is particularly remarkable
compared with other non-communicable diseases—such as cardiovascular disease, stroke, and
respiratory illness—which are projected to exhibit
declining mortality rates.8 Even in its early stages,
CKD is associated with multi-system morbidity that
diminishes quality of life. Notably, mild cognitive
impairment is linked to early-stage CKD; early
detection and treatment could slow cognitive
decline and reduce the risk of dementia.10 Chronic
kidney disease in children has profound additional
consequences, threatening growth and cognitive
development, with lifelong health and quality of life
implications.11 12 The number of people requiring
kidney failure replacement therapy—dialysis or
transplantation—is anticipated to more than
double from 2010 to 2030, reaching 5.4 million.13 14
Kidney failure replacement therapy, particularly
haemodialysis, remains unavailable or unaffordable
for many in LICs and LMICs, contributing to
millions of deaths annually. Although LICs and
LMICs comprise 48% of the global population,
they represent only 7% of the treated kidney failure
population.15
Who is at risk of kidney disease?
Testing individuals at high risk for kidney disease
(case-finding) minimises potential harms and false-positive
results compared with general population
screening, which should only be considered in high-income
countries (HICs). Testing limited to those
at increased risk of CKD would still encompass a large proportion of the global population. Moreover,
targeted case-finding in patients at high risk of
CKD is not optimally performed, even within
HICs. Approximately one in three people globally
have diabetes and/or hypertension. There is a
bidirectional relationship between cardiovascular
disease and CKD—each increases the risk of the
other. Both the American Heart Association and the
European Society of Cardiology recommend testing
individuals with cardiovascular disease for CKD as
part of routine cardiovascular assessments.1 16
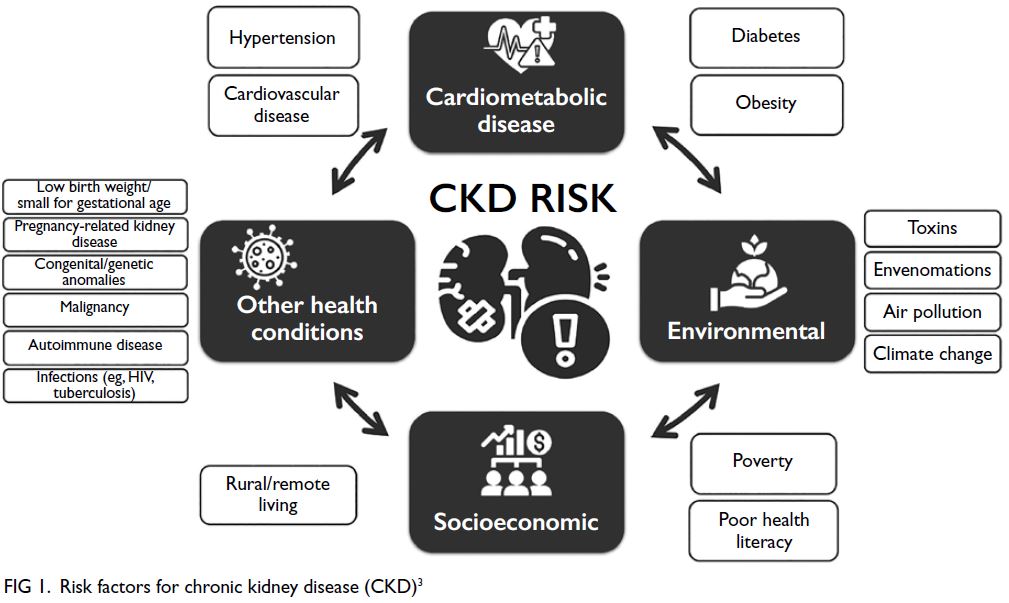
Other CKD risk factors include a family
history of kidney disease (eg, APOL1-mediated
kidney disease, which is common among individuals
of West African ancestry), prior acute kidney injury,
pregnancy-related kidney conditions (eg, pre-eclampsia),
malignancy, autoimmune disorders (such
as systemic lupus erythematosus and vasculitis),
low birth weight or preterm birth, obstructive
uropathy, recurrent kidney stones, and congenital
anomalies of the kidney and urinary tract (Fig 1).3
Social determinants of health strongly influence
CKD risk, both at individual and national levels.
In LICs and LMICs, heat stress among agricultural
workers is thought to contribute to CKD of
unknown aetiology—an increasingly recognised and
major global cause of kidney disease.17 Additionally,
envenomations, environmental toxins, traditional
medicines, and infections (such as hepatitis B or C,
HIV, and parasitic diseases) warrant attention as risk
factors, particularly in endemic regions.18 19
How can we check kidney health?
Conceptually, there are three levels of CKD
prevention. Primary prevention aims to reduce
the incidence of CKD by treating risk factors;
secondary prevention focuses on slowing disease
progression and reducing complications in those
with diagnosed CKD; and tertiary prevention
seeks to improve outcomes in people with kidney
failure by enhancing management, such as through
improved vaccination coverage and optimised
dialysis delivery.20 Primary and secondary prevention
strategies can incorporate the eight golden rules
for promoting kidney health: maintaining a healthy
diet, ensuring adequate hydration, engaging in
physical activity, monitoring and controlling blood
pressure, monitoring and controlling blood glucose
levels, avoiding nicotine, avoiding regular use of
non-steroidal anti-inflammatory drugs, and targeted
testing for those with risk factors.21 Five of these
rules are identical to Life’s Essential 8—guidelines
for maintaining cardiovascular health—which also
include achieving a healthy weight, getting adequate
sleep, and managing lipid levels.22 Early detection
efforts are a form of secondary prevention that
involves protecting kidney health and reducing
cardiovascular risk.
Are your kidneys OK?
Globally, early detection of CKD remains rare,
inconsistent, and less likely in LICs or LMICs.
Currently, only three countries have a national
programme for actively testing at-risk populations
for CKD, and a further 17 countries perform such
testing during routine healthcare encounters.23 Even in
HICs, albuminuria is not assessed in more than half
of individuals with T2DM and/or hypertension.24 25 26
Startlingly, a diagnosis of CKD is often absent even
among those with documented reduced kidney
function. A study conducted in HICs showed that
62% to 96% of individuals with laboratory evidence of
CKD stage G3 had no recorded diagnosis of CKD.27
We recommend that healthcare professionals
perform the following tests for all risk groups to
assess kidney health (Fig 2 28):
a) Blood pressure measurement: Hypertension is
the most prevalent risk factor for kidney disease
worldwide.3 29 30
b) Body mass index: Obesity is epidemiologically associated with CKD risk, both indirectly (via T2DM and hypertension) and directly, as an independent risk factor. Visceral adiposity contributes to monocyte-driven microinflammation and increased cardiometabolic kidney risk.3 29 30
c) Testing for diabetes: Assessment with glycosylated haemoglobin, fasting blood glucose, or random glucose should be part of kidney health screening because T2DM is a common risk factor.3 29 30
d) Evaluation of kidney function: Serum creatinine should be used to estimated glomerular filtration rate (eGFR) in all healthcare settings.3 Glomerular filtration rate should be calculated using a validated, race-free equation appropriate for the specific country or region and age-group.3 In general, eGFR <60 mL/min/1.73 m2 is considered the threshold for CKD in adults and children; a threshold of <90 mL/min/1.73 m2 can be regarded as ‘low’ in children and adolescents over the age of 2 years.3 A limitation of creatinine-based eGFR is its sensitivity to nutritional status and muscle mass, which can lead to overestimation in states of malnutrition or frailty.3 28 Thus, the use of both serum creatinine and cystatin C provides a more accurate estimate of eGFR in most clinical contexts. However, the feasibility of cystatin C testing is mainly limited to HICs because of assay availability and cost relative to creatinine testing.3 28 31
e) Testing for kidney damage (albuminuria): In both adults and children, a first morning urine sample is preferred for assessing albuminuria.3 In adults, the quantitative urinary albumin–creatinine ratio (uACR) is the most sensitive and preferred test.3 Analytical standardisation of urinary albumin is currently underway, which should eventually support global standardisation of uACR testing.32 In children, both the protein–creatinine ratio and uACR should be tested to identify tubular proteinuria.3 Semiquantitative albuminuria testing provides flexibility for point-of-care or home-based testing.33 To be considered useful, semiquantitative or qualitative screening tests should correctly identify >85% of individuals with a quantitative uACR of ≥30 mg/g.34 In resource-limited settings, urine dipstick testing may be used, with a threshold of +2 proteinuria or greater to reduce false positives and guide repeat confirmatory testing.35
b) Body mass index: Obesity is epidemiologically associated with CKD risk, both indirectly (via T2DM and hypertension) and directly, as an independent risk factor. Visceral adiposity contributes to monocyte-driven microinflammation and increased cardiometabolic kidney risk.3 29 30
c) Testing for diabetes: Assessment with glycosylated haemoglobin, fasting blood glucose, or random glucose should be part of kidney health screening because T2DM is a common risk factor.3 29 30
d) Evaluation of kidney function: Serum creatinine should be used to estimated glomerular filtration rate (eGFR) in all healthcare settings.3 Glomerular filtration rate should be calculated using a validated, race-free equation appropriate for the specific country or region and age-group.3 In general, eGFR <60 mL/min/1.73 m2 is considered the threshold for CKD in adults and children; a threshold of <90 mL/min/1.73 m2 can be regarded as ‘low’ in children and adolescents over the age of 2 years.3 A limitation of creatinine-based eGFR is its sensitivity to nutritional status and muscle mass, which can lead to overestimation in states of malnutrition or frailty.3 28 Thus, the use of both serum creatinine and cystatin C provides a more accurate estimate of eGFR in most clinical contexts. However, the feasibility of cystatin C testing is mainly limited to HICs because of assay availability and cost relative to creatinine testing.3 28 31
e) Testing for kidney damage (albuminuria): In both adults and children, a first morning urine sample is preferred for assessing albuminuria.3 In adults, the quantitative urinary albumin–creatinine ratio (uACR) is the most sensitive and preferred test.3 Analytical standardisation of urinary albumin is currently underway, which should eventually support global standardisation of uACR testing.32 In children, both the protein–creatinine ratio and uACR should be tested to identify tubular proteinuria.3 Semiquantitative albuminuria testing provides flexibility for point-of-care or home-based testing.33 To be considered useful, semiquantitative or qualitative screening tests should correctly identify >85% of individuals with a quantitative uACR of ≥30 mg/g.34 In resource-limited settings, urine dipstick testing may be used, with a threshold of +2 proteinuria or greater to reduce false positives and guide repeat confirmatory testing.35
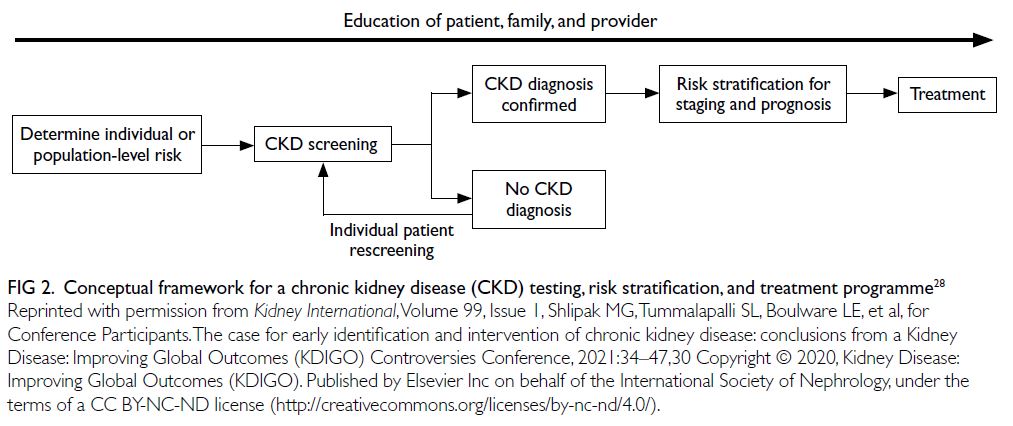
Figure 2. Conceptual framework for a chronic kidney disease (CKD) testing, risk stratification, and treatment programme28
In specific populations, the following
considerations may apply:
f) Testing for haematuria: Haematuria is often
overlooked in recent clinical practice guidelines,
despite its importance as a risk factor (particularly
for individuals at risk of glomerular disease, such
as immunoglobulin A nephropathy).36
g) Baseline imaging: Imaging should be performed in individuals presenting with signs or symptoms of structural abnormalities (eg, pain and haematuria) to identify kidney masses, cysts, stones, hydronephrosis, or urinary retention. Antenatal ultrasound can detect hydronephrosis and other congenital anomalies of the kidney and urinary tract.
h) Genetic testing: With increasing access to genetic diagnostics, family cascade testing for CKD is indicated where there is a known hereditary risk of kidney disease.37
i) Occupational health screening: Individuals with occupational risk of developing kidney disease should be offered kidney function testing as part of workplace health programmes.
j) Post-donation surveillance: Kidney donors should be included in long-term follow-up programmes to monitor kidney health after donation.38
g) Baseline imaging: Imaging should be performed in individuals presenting with signs or symptoms of structural abnormalities (eg, pain and haematuria) to identify kidney masses, cysts, stones, hydronephrosis, or urinary retention. Antenatal ultrasound can detect hydronephrosis and other congenital anomalies of the kidney and urinary tract.
h) Genetic testing: With increasing access to genetic diagnostics, family cascade testing for CKD is indicated where there is a known hereditary risk of kidney disease.37
i) Occupational health screening: Individuals with occupational risk of developing kidney disease should be offered kidney function testing as part of workplace health programmes.
j) Post-donation surveillance: Kidney donors should be included in long-term follow-up programmes to monitor kidney health after donation.38
Potential benefits of early detection
Screening for CKD aligns well with many
of the World Health Organization (WHO)’s
Wilson–Jungner principles.39 Early-stage CKD
is asymptomatic; effective interventions—including lifestyle modification, interdisciplinary
care, and pharmacological treatments—are well
established.2 3 28 35 Several WHO Essential Medicines
that improve CKD outcomes should be widely available, including angiotensin-converting enzyme
inhibitors, angiotensin receptor blockers, statins,
and SGLT2is (sodium-glucose co-transporter-2
inhibitors).2 40 Sodium glucose co-transporter-2
inhibitors alone are estimated to decrease the risk
of CKD progression by 37% in individuals with and
without diabetes.41 For a 50-year-old individual with
albuminuria and non-diabetic CKD, this treatment
could extend their healthy kidney function period
from 9.6 to 17 years.42 These essential medicines
slow progression to more advanced CKD stages
and reduce cardiovascular hospitalisations,
offering near-term cost-effectiveness—especially
vital for LICs. Where available and affordable,
the range of paradigm-shifting medications to
slow CKD progression includes glucagon-like
peptide-1 receptor antagonists, non-steroidal
mineralocorticoid receptor antagonists, endothelin
receptor antagonists, and specific disease-modifying
drugs (eg, complement-inhibitors); these treatments
herald an exciting new era for nephrology.
Considering the substantial healthcare costs
associated with CKD—particularly those related
to hospitalisation and kidney failure—effective
preventive measures offer clear economic benefits
for both HICs and LICs. Chronic kidney disease
imposes enormous financial burdens on individuals,
their families, healthcare systems, and governments
worldwide. In the United States, CKD costs Medicare
over US$85 billion annually.13 In many HICs and
middle-income countries, 2% to 4% of national
health budgets are allocated to kidney failure care
alone. In Europe, healthcare costs related to CKD
exceed those associated with cancer or diabetes.43
Reducing the global burden of kidney care would also
yield important environmental benefits, including
reductions in water usage and plastic waste,
especially from dialysis.44 On an individual level,
CKD costs are frequently catastrophic, particularly
in LICs and LMICs, where the individuals often bear the majority of healthcare expenses. Only 13%
of LICs and 19% of LMICs provide kidney failure
replacement therapy coverage for adults.15 Each
year, CKD causes an estimated 188 million people
in LICs and LMICs to incur catastrophic healthcare
expenditures.45
The most widely cited and studied incremental
cost effectiveness ratio threshold for assessing
screening interventions is US$<50 000 per quality-adjusted
life year.46 When CKD prevalence is high,
population-wide screening strategies may be
considered in HICs.33 47 For example, in the United
States, a recent Markov simulation model assessed
population-wide CKD screening in adults aged 35
to 75 years with albuminuria. The model included
treatment with SGLT2is, in addition to standard
care with ACE inhibitors or angiotensin receptor
blockers. The analysis indicated that such a screening
approach would be cost-effective.47 Additionally,
an evaluation of home-based, semiquantitative
albuminuria screening in the general population in
the Netherlands showed that it was cost-effective.33
Case finding—targeting higher-risk groups for CKD
detection—offers a more efficient and cost-effective
approach than mass or general population screening.
It reduces costs and potential harms while increasing
the true positive rate of screening tests.3 35 46 An
alternative incremental cost-effectiveness ratio
threshold, proposed by the WHO, suggests using
a benchmark of less than 1 to 3 times the gross
domestic product per capita per quality-adjusted
life year to evaluate cost-effectiveness in LICs and
LMICs.46 The recommended tests for detecting
kidney disease are low-cost and minimally invasive,
making them feasible across diverse healthcare
settings. Basic tests, such as eGFR and uACR, are
widely available. In contexts where quantitative
testing for proteinuria is unavailable or unaffordable,
the use of urine dipstick testing can substantially
reduce costs.31
When coupled with effective interventions,
early identification of individuals with kidney
disease would yield benefits for patients, healthcare
systems, governments, and national economies.45
Health and quality-of-life gains for individuals
would lead to greater productivity—especially for
younger people with more working years ahead—while improving developmental and educational
outcomes in children and young adults. Individuals
would also be less likely to face catastrophic
healthcare expenses. Governments and healthcare
systems would benefit from reduced CKD-related
expenditures and lower cardiovascular disease costs.
Economies would benefit from increased workforce
participation. These benefits are especially crucial
for lower-income countries, where the burden of
CKD is greatest but the capacity to fund kidney care
is most limited.
Challenges and solutions for implementation
Structural barriers to widespread CKD identification
and treatment include high costs, limited test
reliability, and lack of health information systems
to monitor CKD burden. These challenges are
compounded by a lack of relevant government
and healthcare policy, low levels of CKD-related
knowledge and implementation among healthcare
professionals, and limited public awareness of CKD
and low perceived risk among the general population.
Solutions for implementing effective interventions
include integrating CKD identification into existing
screening programmes, educating both the public
and primary care professionals, and leveraging
joint advocacy efforts from non-governmental
organisations to focus health policy agendas
on kidney disease. Any proposed solution must
carefully balance the potential benefits and harms
of screening and case-finding initiatives. Ethical
considerations encompass resource availability
(such as trained healthcare workers and access to
medicines), affordability of testing and treatment,
and the psychological impact of false positives or
negatives, including potential anxiety for patients
and their families.48
Successful screening and case-finding
programmes require adequate workforce capacity,
robust health information systems, reliable testing
equipment, and equitable access to medical
care, essential medicines, vaccines, and medical
technologies. Primary care plays a pivotal role in
protecting kidney health, particularly in LICs and
LMICs. The limited global nephrology workforce,
with a median prevalence of only 11.8 nephrologists
per million population, and an 80-fold disparity
between LICs and HICs, is inadequate to detect and
manage the vast majority of CKD.23 As with other
chronic diseases, primary care clinicians and frontline
health workers are essential for the early detection and
management of CKD.49 Testing must be affordable,
simple, and practical. In resource-limited settings,
point-of-care creatinine testing and urine dipsticks
are especially useful.31 Educational efforts targeting
primary care clinicians are crucial to integrating CKD
detection into routine clinical practice, despite time
and resource constraints.50 51 52 Additionally, automated
clinical decision support systems can leverage
electronic health records to identify individuals with
CKD or those at high risk, then prompt clinicians
with appropriate actions (Fig 228).
Currently, few countries have CKD registries,
limiting the ability to accurately quantify disease
burden and advocate for resources. Knowledge of
the CKD burden is essential for prioritising kidney
health and developing strategies that progressively
expand to encompass the full spectrum of kidney care.53 A global survey revealed only one-quarter
of countries (41/162) had a national CKD strategy,
and fewer than one-third (48/162) recognised
CKD as a public health priority.23 Recognition by
the WHO that CKD is a major contributor to non-communicable
disease mortality would be a crucial
step forward. It would help raise awareness, enhance
local surveillance and monitoring, support the
implementation of clinical practice guidelines, and
improve allocation of healthcare resources.2
Programmes for the early detection of CKD
will require extensive coordination and active
engagement from a wide range of stakeholders,
including governments, healthcare systems,
and insurers. International and national kidney
organisations—such as the International Society
of Nephrology—are already advocating to the
WHO and individual governments for greater
prioritisation of kidney disease. We must continue
this work through collaborative efforts to streamline
the planning and implementation of early detection
programmes. Integration with existing community
interventions (eg, cardiovascular disease prevention
initiatives) in both LICs and HICs can decrease costs
and maximise efficiency by building on established
infrastructures. Such programmes must be adapted
to local contexts and can be delivered in a variety of
settings, including general practice clinics, hospitals,
regional or national healthcare facilities, and rural
outreach initiatives. Depending on local regulations
and available resources, screening and case-finding
can also occur outside conventional medical
environments, for example, in town halls, churches,
or markets. Community volunteers can also assist
with these outreach and screening efforts.
In conjunction with changes in clinical
practice to promote earlier detection of CKD, we
must also focus on increasing public awareness of
kidney disease risk and promoting health education. Such campaigns should be aimed at both the general
public and patients, with the goal of fostering
greater awareness and self-empowerment. General
population awareness of CKD is poor: nine of ten
people with the condition are unaware that they are
affected.54 Furthermore, kidney disease is missing
from mainstream media. One analysis of lay press
coverage showed that kidney disease was discussed
11 times less frequently than would be expected based
on its actual contribution to mortality.55 A number
of national and international organisations have
developed public-facing quizzes to help individuals
assess their risk of kidney disease. These initiatives are
supported by regional studies showing that socially
vulnerable patients with hypertension often do not
understand their kidney health risks.21 56 57 58 Online
and direct education for healthcare professionals
can also help improve consumer health literacy.
Awareness leads to increased patient activation,
engagement, and shared decision-making. However,
education around CKD must be nuanced—balancing
the need for detection and risk stratification with the
importance of informing and empowering, rather
than frightening, individuals about the timing and
extent of potential interventions (Box).4 58 Striking
this balance will be critical for optimising self-efficacy
and encouraging active involvement from
patients, families and caregivers.
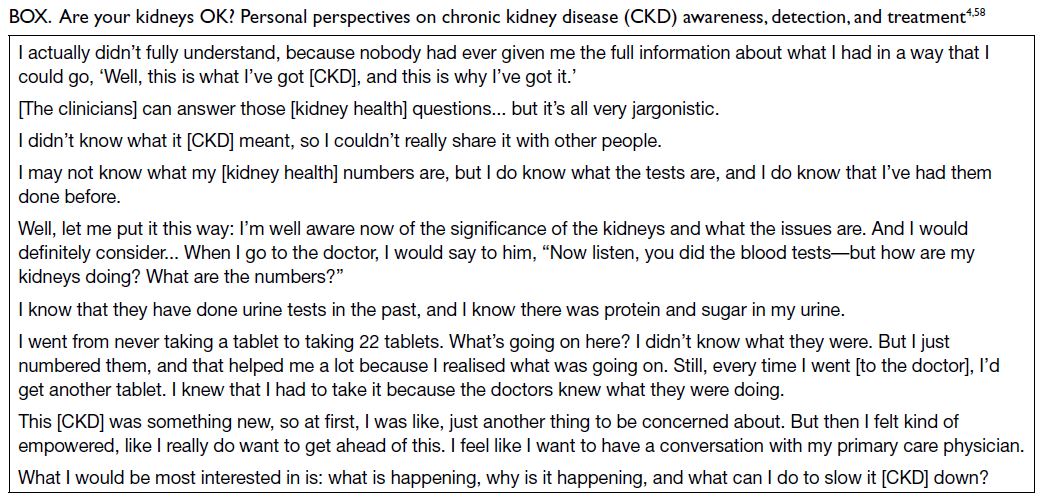
Box. Are your kidneys OK? Personal perspectives on chronic kidney disease (CKD) awareness, detection, and treatment4 58
Conclusion: a call to action
We call on all healthcare professionals to assess
the kidney health of patients at risk of CKD.
Concurrently, we must partner with public health
organisations to raise awareness among the general
population about the risk of kidney disease and
empower at-risk individuals to proactively seek
kidney health checks. To make meaningful progress,
collaboration with healthcare systems, governments,
and the WHO is essential to prioritise kidney disease and develop effective, efficient early detection
programmes. Only through these efforts can we
ensure that the paradigm-shifting benefits of lifestyle
changes and pharmacological treatments are fully
realised, leading to better kidney and overall health
outcomes for people around the world.
Author contributions
All authors contributed equally to the conception, preparation,
and editing of the manuscript. All authors approved the final
version for publication and take responsibility for its accuracy
and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank members of the World Kidney Day Joint
Steering Committee, including Valerie A Luyckx, Marcello
Tonelli, Ifeoma Ulasi, Vivekanand Jha, Marina Wainstein,
Siddiq Anwar, Daniel O’Hara, Elliot K Tannor, Jorge Cerda,
Elena Cervantes, and María Carlota González Bedat, for their
invaluable feedback on this article.
Declaration
This article was published in Kidney International
(Vassalotti JA, Francis A, Soares Dos Santos AC Jr, et al.
Are your kidneys Ok? Detect early to protect kidney health.
Kidney International. 2025;107(3):370-377. https://dx.doi.org/10.1016/j.kint.2024.12.006) and reprinted concurrently
in several journals. The articles cover identical concepts and
wording, but vary in minor stylistic and spelling changes,
detail, and length of manuscript in keeping with each journal’s
style. Any of these versions may be used in citing this article.
Funding/support
This editorial received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Ndumele CE, Neeland IJ, Tuttle KR, et al. A synopsis of
the evidence for the science and clinical management of
cardiovascular-kidney-metabolic (CKM) syndrome: a
scientific statement from the American Heart Association.
Circulation 2023;148:1636-64. Crossref
2. Luyckx VA, Tuttle KR, Abdellatif D, et al. Mind the gap in
kidney care: translating what we know into what we do.
Kidney Int 2024;105:406-17. Crossref
3. Stevens PE, Ahmed SB, Carrero JJ, et al. KDIGO 2024
Clinical Practice Guideline for the evaluation and
management of chronic kidney disease. Kidney Int
2024;105:S117-314. Crossref
4. Guha C, Lopez-Vargas P, Ju A, et al. Patient needs
and priorities for patient navigator programmes in
chronic kidney disease: a workshop report. BMJ Open
2020;10:e040617. Crossref
5. GBD Chronic Kidney Disease Collaboration. Global,
regional, and national burden of chronic kidney disease,
1990-2017: a systematic analysis for the Global Burden of
Disease Study 2017. Lancet 2020;395:709-33. Crossref
6. Cojuc-Konigsberg G, Guijosa A, Moscona-Nissan A, et al. Representation of low- and middle-income countries in CKD drug trials: a systematic review. Am J Kidney Dis
2025;85:55-66.e1. Crossref
7. Hsiao LL, Shah KM, Liew A, et al. Kidney health for
all: preparedness for the unexpected in supporting the
vulnerable. Kidney Int 2023;103:436-43. Crossref
8. Francis A, Harhay MN, Ong AC, et al. Chronic kidney
disease and the global public health agenda: an international
consensus. Nat Rev Nephrol 2024;20:473-85. Crossref
9. Foreman KJ, Marquez N, Dolgert A, et al. Forecasting
life expectancy, years of life lost, and all-cause and cause-specific
mortality for 250 causes of death: reference and
alternative scenarios for 2016-40 for 195 countries and
territories. Lancet 2018;392:2052-90. Crossref
10. Viggiano D, Wagner CA, Martino G, et al. Mechanisms
of cognitive dysfunction in CKD. Nat Rev Nephrol
2020;16:452-69. Crossref
11. Chen K, Didsbury M, van Zwieten A, et al. Neurocognitive and educational outcomes in children and adolescents with CKD: a systematic review and meta-analysis. Clin J Am Soc Nephrol 2018;13:387-97. Crossref
12. Francis A, Didsbury MS, van Zwieten A, et al. Quality of life of children and adolescents with chronic kidney disease: a cross-sectional study. Arch Dis Child 2019;104:134-40. Crossref
13. United States Renal Data System. 2023 USRDS Annual Data Report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2023.
14. Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 2015;385:1975-82. Crossref
15. Bello AK, Levin A, Tonelli M, et al. Assessment of global kidney health care status. JAMA 2017;317:1864-81. Crossref
16. Ortiz A, Wanner C, Gansevoort R; ERA Council. Chronic kidney disease as cardiovascular risk factor in routine clinical practice: a position statement by the Council of the European Renal Association. Nephrol Dial Transplant 2023;38:527-31. Crossref
17. Johnson RJ, Wesseling C, Newman LS. Chronic kidney disease of unknown cause in agricultural communities. N Engl J Med 2019;380:1843-52. Crossref
18. McCulloch M, Luyckx VA, Cullis B, et al. Challenges of access to kidney care for children in low-resource settings. Nat Rev Nephrol 2021;17:33-45. Crossref
19. Stanifer JW, Muiru A, Jafar TH, Patel UD. Chronic kidney disease in low- and middle-income countries. Nephrol Dial Transplant 2016;31:868-74. Crossref
20. Levey AS, Schoolwerth AC, Burrows NR, et al. Comprehensive public health strategies for preventing the development, progression, and complications of CKD: report of an expert panel convened by the Centers for Disease Control and Prevention. Am J Kidney Dis 2009;53:522-35. Crossref
21. Internation Society of Nephrology. World Kidney Day 2025. Available from: https://www.worldkidneyday.org/about-kidney-health/. Accessed 11 Jan 2025.
22. Lloyd-Jones DM, Allen NB, Anderson CA, et al. Life's Essential 8: updating and enhancing the American Heart Association's Construct of Cardiovascular Health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18-43. Crossref
23. Bello AK, Okpechi IG, Levin A, et al. An update on the global disparities in kidney disease burden and care across world countries and regions. Lancet Glob Health 2024;12:e382-95. Crossref
24. Ferrè S, Storfer-Isser A, Kinderknecht K, et al. Fulfillment and validity of the kidney health evaluation measure for people with diabetes. Mayo Clin Proc Innov Qual Outcomes 2023;7:382-91. Crossref
25. Alfego D, Ennis J, Gillespie B, et al. Chronic kidney disease testing among at-risk adults in the U.S. remains low: real-world evidence from a national laboratory database. Diabetes Care 2021;44:2025-32. Crossref
26. Stempniewicz N, Vassalotti JA, Cuddeback JK, et al. Chronic kidney disease testing among primary care patients with type 2 diabetes across 24 U.S. health care organizations. Diabetes Care 2021;44:2000-9. Crossref
27. Kushner PR, DeMeis J, Stevens P, Gjurovic AM, Malvolti E, Tangri N. Patient and clinician perspectives: to create a better future for chronic kidney disease, we need to talk about our kidneys. Adv Ther 2024;41:1318-24. Crossref
28. Shlipak MG, Tummalapalli SL, Boulware LE, et al. The case for early identification and intervention of chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int 2021;99:34-47. Crossref
29. Farrell DR, Vassalotti JA. Screening, identifying, and treating chronic kidney disease: why, who, when, how, and what? BMC Nephrol 2024;25:34. Crossref
30. Tuttle KR. CKD screening for better kidney health: why? who? how? when? Nephrol Dial Transplant 2024;39:1537-9. Crossref
31. Tummalapalli SL, Shlipak MG, Damster S, et al. Availability and affordability of kidney health laboratory tests around the globe. Am J Nephrol 2020;51:959-65. Crossref
32. Seegmiller JC, Bachmann LM. Urine albumin measurements in clinical diagnostics. Clin Chem 2024;70:382-91. Crossref
33. van Mil D, Kieneker LM, Heerspink HJ, Gansevoort RT. Screening for chronic kidney disease: change of perspective and novel developments. Curr Opin Nephrol Hypertens 2024;33:583-92. Crossref
34. Sacks DB, Arnold M, Bakris GL, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem 2023;69:808-68. Crossref
35. Tonelli M, Dickinson JA. Early detection of CKD: implications for low-income, middle-income, and high-income countries. J Am Soc Nephrol 2020;31:1931-40. Crossref
36. Moreno JA, Martín-Cleary C, Gutiérrez E, et al. Haematuria: the forgotten CKD factor? Nephrol Dial Transplant 2012;27:28-34. Crossref
37. Franceschini N, Feldman DL, Berg JS, et al. Advancing genetic testing in kidney diseases: report from a National Kidney Foundation Working Group. Am J Kidney Dis 2024;84:751-66. Crossref
38. Mjøen G, Hallan S, Hartmann A, et al. Long-term risks for kidney donors. Kidney Int 2014;86:162-7. Crossref
39. Wilson JM, Jungner G, World Health Organization. Public
Health Papers. Principles and practice of screening for
disease. World Health Organization, 1968. Available from:
https://apps.who.int/iris/handle/10665/37650. Accessed 11 Apr 2025.
40. Francis A, Abdul Hafidz MI, Ekrikpo UE, et al. Barriers to accessing essential medicines for kidney disease in low- and lower middle-income countries. Kidney Int 2022;102:969-73. Crossref
41. Baigent C, Emberson J, Haynes R, et al. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. Lancet 2022;400:1788-801. Crossref
42. Vart P, Vaduganathan M, Jongs N, et al. Estimated lifetime benefit of combined RAAS and SGLT2 inhibitor therapy in patients with albuminuric CKD without diabetes. Clin J Am Soc Nephrol 2022;17:1754-62. Crossref
43. Vanholder R, Annemans L, Brown E, et al. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat Rev Nephrol 2017;13:393-409. Crossref
44. Berman-Parks N, Berman-Parks I, Gómez-Ruíz IA, Ardavin-Ituarte JM, Piccoli GB. Combining patient care and environmental protection: a pilot program recycling polyvinyl chloride from automated peritoneal dialysis waste. Kidney Int Rep 2024;9:1908-11. Crossref
45. Essue BM, Laba M, Knaul F, et al. Economic burden of chronic ill health and injuries for households in low- and middle-income countries. In: Jamison DT, Gelband H, Horton S, editors. Disease Control Priorities: Improving Health and Reducing Poverty. Washington (DC): The International Bank for Reconstruction and Development/The World Bank; 2017. Crossref
46. Yeo SC, Wang H, Ang YG, Lim CK, Ooi XY. Cost-effectiveness of screening for chronic kidney disease in the general adult population: a systematic review. Clin Kidney J 2024;17:sfad137. Crossref
47. Cusick MM, Tisdale RL, Chertow GM, Owens DK, Goldhaber-Fiebert JD. Population-wide screening for chronic kidney disease: a cost-effectiveness analysis. Ann Intern Med 2023;176:788-97. Crossref
48. Yadla M, John P, Fong VK, Anandh U. Ethical issues related to early screening programs in low resource settings. Kidney Int Rep 2024;9:2315-9. Crossref
49. Szczech LA, Stewart RC, Su HL, et al. Primary care detection of chronic kidney disease in adults with type-2 diabetes: the ADD-CKD Study (awareness, detection and drug therapy in type 2 diabetes and chronic kidney disease). PLoS One 2014;9:e110535. Crossref
50. Vassalotti JA, Centor R, Turner BJ, et al. Practical approach to detection and management of chronic kidney disease for the primary care clinician. Am J Med 2016;129:153-62.e7. Crossref
51. Thavarajah S, Knicely DH, Choi MJ. CKD for primary care practitioners: can we cut to the chase without too many shortcuts? Am J Kidney Dis 2016;67:826-9. Crossref
52. Vassalotti JA, Boucree SC. Integrating CKD into US primary care: bridging the knowledge and implementation gaps. Kidney Int Rep 2022;7:389-96. Crossref
53. Luyckx VA, Moosa MR. Priority setting as an ethical imperative in managing global dialysis access and improving kidney care. Semin Nephrol 2021;41:230-41. Crossref
54. US Centers for Disease Control and Prevention. Chronic
kidney disease in the United States, 2023. Available from:
https://www.cdc.gov/kidney-disease/php/data-research/index.html. Accessed 11 Jan 2025.
55. Dattani S, Spooner F, Ritchie H, Roser M. Causes of death.
2023. Available from: https://ourworldindata.org/causes-of-death. Accessed 11 Jan 2025.
56. Boulware LE, Carson KA, Troll MU, Powe NR, Cooper LA. Perceived susceptibility to chronic kidney disease among high-risk patients seen in primary care practices. J Gen Intern Med 2009;24:1123-9. Crossref
57. National Kidney Foundation. Kidney Quiz 2024. Available
from: https://www.kidney.org/kidney-quiz/. Accessed 11 Jan 2025. Crossref
58. Tuot DS, Crowley ST, Katz LA, et al. Usability testing of the kidney score platform to enhance communication about kidney disease in primary care settings: qualitative think-aloud study. JMIR Form Res 2022;6:e40001. Crossref