Hong Kong Med J 2025 Feb;31(1):72–3.e1–3 | Epub 6 Feb 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Duplication of the portal vein and the implications for procedural planning
OL Chan, MB, BS, FRCR1; YS Lee, FRCR, FHKAM (Radiology)1; CH Ho, FRCR, FHKAM (Radiology)1; CC Lee, FRCS, FHKAM (Surgery)2; CC Cheung, FRCS, FHKAM (Surgery)2
1 Department of Radiology and Nuclear Medicine, Tuen Mun Hospital, Hong Kong SAR, China
2 Department of Surgery, Tuen Mun Hospital, Hong Kong SAR, China
Corresponding author: Dr OL Chan (col950@ha.org.hk)
A 72-year-old man with recurrent hepatitis B virus–related hepatocellular carcinoma was referred for
right portal vein embolisation (PVE) prior to right
hepatectomy. He had Child-Pugh class A cirrhosis,
with calculated indocyanine green–R15 of 8%. Portal
embolisation was indicated due to the presence of
multiple co-morbidities and marginal future liver
remnant volume of 35%.
Preprocedural computed tomography
revealed duplication of the portal vein (DPV) [Fig 1]. The anatomy and feasibility of the procedure was
discussed with hepatic surgeons. Right PVE was
successfully performed with n-butyl cyanoacrylate
glue. Left hepatic lobe hypertrophy from 430 cm3
to 560 cm3 was achieved. The patient subsequently
underwent an uneventful right hepatectomy.
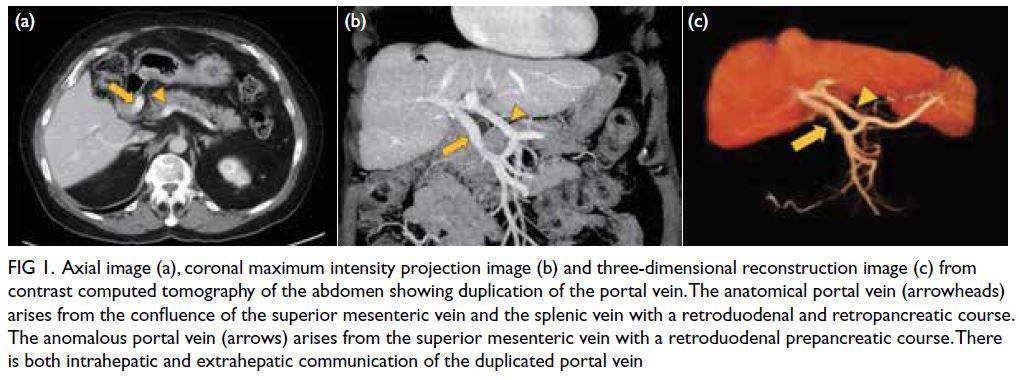
Figure 1. Axial image (a), coronal maximum intensity projection image (b) and three-dimensional reconstruction image (c) from contrast computed tomography of the abdomen showing duplication of the portal vein. The anatomical portal vein (arrowheads) arises from the confluence of the superior mesenteric vein and the splenic vein with a retroduodenal and retropancreatic course. The anomalous portal vein (arrows) arises from the superior mesenteric vein with a retroduodenal prepancreatic course. There is both intrahepatic and extrahepatic communication of the duplicated portal vein
Portal vein embolisation is a commonly
adopted strategy to induce future liver remnant
hypertrophy prior to hepatectomy. Knowledge of
the portal venous anatomy and its variants is vital for
treatment planning. Duplication of the portal vein is
a rare congenital anomaly that has been described
only in case reports. It is related to the spectrum of
vitelline vein regression anomaly with pathogenesis
believed to be failed regression of the left cranial
part of the vitelline vein (Fig 2a-e).1 A variation of
DPV has been reported; some authors describe two
portal veins arising separately without extrahepatic
communications,2 while some describe an additional
portal vein arising anomalously from either the
superior mesenteric vein or the splenic vein (Fig 2f-i).3 The latter was evident in our patient (Fig 1).
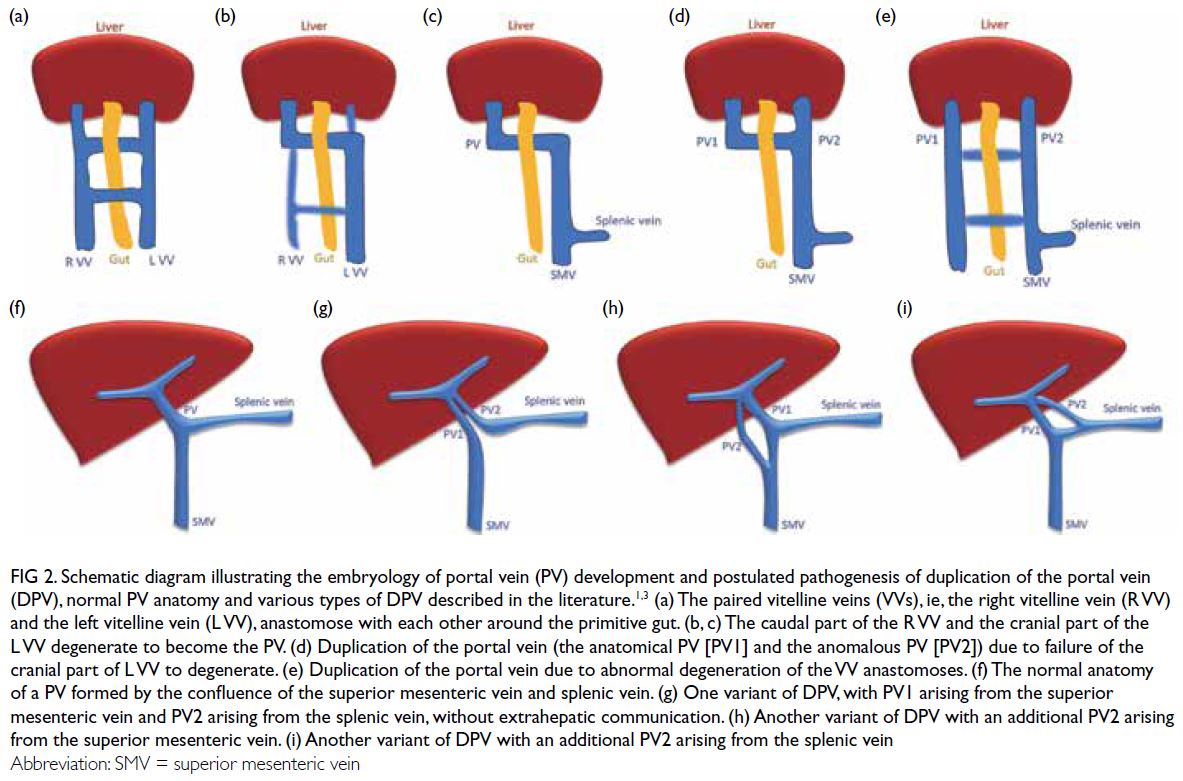
Figure 2. Schematic diagram illustrating the embryology of portal vein (PV) development and postulated pathogenesis of duplication of the portal vein (DPV), normal PV anatomy and various types of DPV described in the literature.1,3 (a) The paired vitelline veins (VVs), ie, the right vitelline vein (R VV) and the left vitelline vein (L VV), anastomose with each other around the primitive gut. (b, c) The caudal part of the R VV and the cranial part of the L VV degenerate to become the PV. (d) Duplication of the portal vein (the anatomical PV [PV1] and the anomalous PV [PV2]) due to failure of the cranial part of L VV to degenerate. (e) Duplication of the portal vein due to abnormal degeneration of the VV anastomoses. (f) The normal anatomy of a PV formed by the confluence of the superior mesenteric vein and splenic vein. (g) One variant of DPV, with PV1 arising from the superior mesenteric vein and PV2 arising from the splenic vein, without extrahepatic communication. (h) Another variant of DPV with an additional PV2 arising from the superior mesenteric vein. (i) Another variant of DPV with an additional PV2 arising from the splenic vein
Another anomaly with double channel portal
vein is portal vein fenestration in which there
is a small fenestration at the mid portion of the
main portal vein.4 The exact pathogenesis and its
relationship with portal vein duplication remains
unknown.
In the presence of DPV, there was altered flow
dynamic with preferential opacification of the right
or left portal vein branches depending on different
catheter tip positions (Fig 3). There was preferential
flow towards the left portal branches at the
intrahepatic communication at the hepatic hilum,
giving a narrow safety margin for embolisation to
prevent non-target embolisation of the left portal
vein that could jeopardise the future liver remnant.
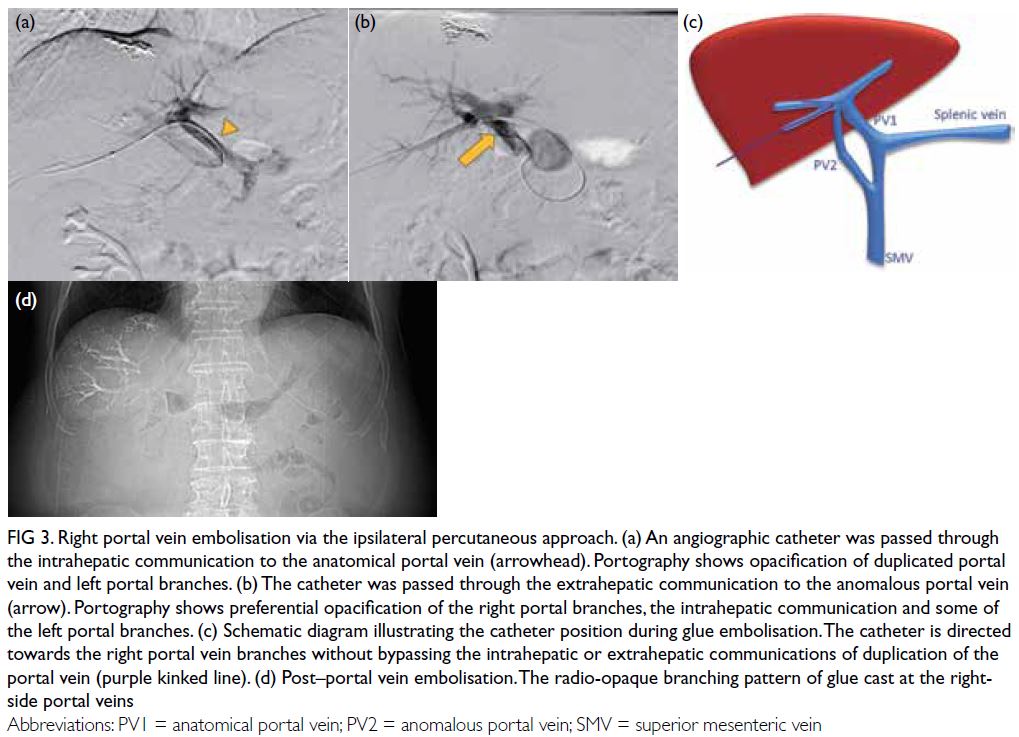
Figure 3. Right portal vein embolisation via the ipsilateral percutaneous approach. (a) An angiographic catheter was passed through the intrahepatic communication to the anatomical portal vein (arrowhead). Portography shows opacification of duplicated portal vein and left portal branches. (b) The catheter was passed through the extrahepatic communication to the anomalous portal vein (arrow). Portography shows preferential opacification of the right portal branches, the intrahepatic communication and some of the left portal branches. (c) Schematic diagram illustrating the catheter position during glue embolisation. The catheter is directed towards the right portal vein branches without bypassing the intrahepatic or extrahepatic communications of duplication of the portal vein (purple kinked line). (d) Post–portal vein embolisation. The radio-opaque branching pattern of glue cast at the right-side portal veins
Our patient successfully underwent PVE
without complication. The degree of hypertrophy
was similar to that reported in local cohorts.5
Surgeons discussed whether the anomalous portal
vein could be embolised to improve the efficacy
of PVE but there was also a risk of jeopardising
venous return from small branches of the superior
mesenteric vein that may worsen liver function.
During hepatectomy, DPV was confirmed (Fig 4). It did not affect surgical planning and the patient
underwent right hepatectomy uneventfully.
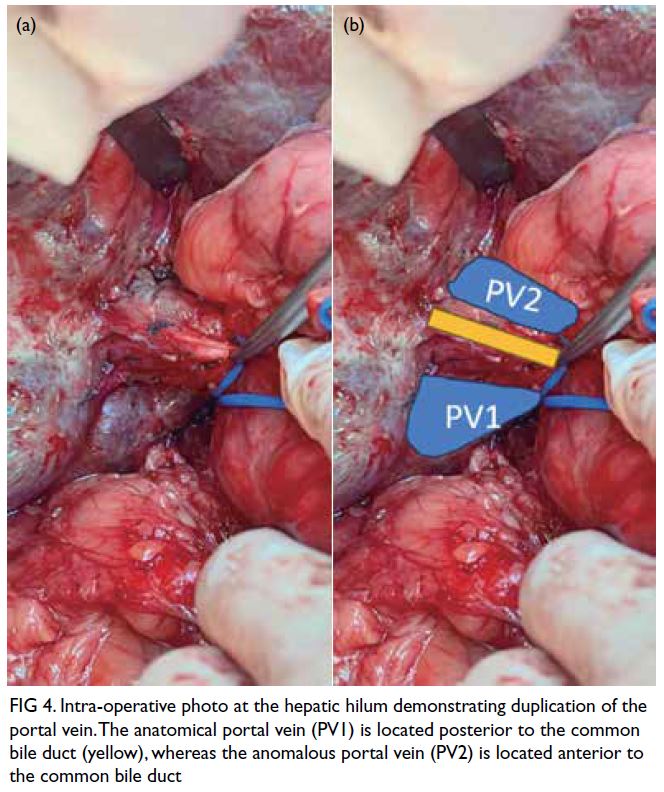
Figure 4. Intra-operative photo at the hepatic hilum demonstrating duplication of the portal vein. The anatomical portal vein (PV1) is located posterior to the common bile duct (yellow), whereas the anomalous portal vein (PV2) is located anterior to the common bile duct
Duplication of the portal vein is a rare
congenital anomaly. Because of the possible altered
flow dynamics, it is important to identify this
anomaly on preprocedural imaging and arrange
multidisciplinary team discussion to plan PVE and
ensure a safe and effective procedure.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: OL Chan, YS Lee.
Drafting of the manuscript: OL Chan, YS Lee.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: OL Chan, YS Lee.
Drafting of the manuscript: OL Chan, YS Lee.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Central Institutional Review
Board of Hospital Authority, Hong Kong (Ref No.: CIRB-2023-064-1). Written informed consent was obtained from
the patient for publication of this article.
References
1. Qin Y, Wen H, Liang M, et al. A new classification of
congenital abnormalities of UPVS: sonographic appearances,
screening strategy and clinical significance. Insights Imaging
2021;12:125. Crossref
2. Dighe M, Vaidya S. Case report. Duplication of the portal
vein: a rare congenital anomaly. Br J Radiol 2009;82:e32-4. Crossref
3. Kitagawa S. Anomalous duplication of the portal vein
with prepancreatic postduodenal portal vein. J Rural Med
2022;17:259-61. Crossref
4. Balradja I, Har B, Rastogi R, Agarwal S, Gupta S. Portal
vein fenestration: a case report of an unusual portal vein
developmental anomaly. Korean J Transplant 2022;36:298-301. Crossref
5. Yu KC, Wong SS, Wong YC, et al. Procedure time, efficacy,
and safety of portal vein embolisation using a sheathless
needle-only technique compared with traditional technique.
Hong Kong J Radiol 2022;25:35-44. Crossref

