Hong Kong Med J 2025 Feb;31(1):65–7 | Epub 11 Feb 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
First experience using a wireless oesophageal pH
monitoring system in children in Hong Kong: three case reports
Adrian CH Fung, MB, BS, FRCSEd (Paed); Kenneth KY Wong, PhD, FRCSEd (Paed)
Department of Surgery, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof Kenneth KY Wong (kkywong@hku.hk)
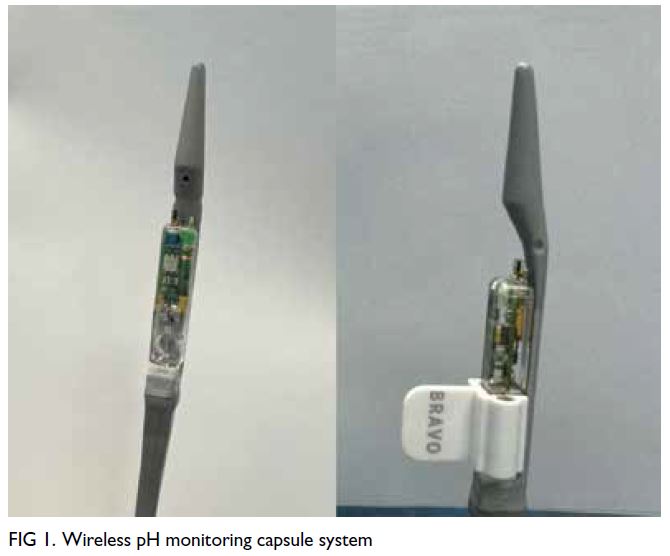
Twenty-four–hour pH monitoring is indicated for
evaluation of gastroesophageal reflux symptoms in
children, as well as part of a preoperative work-up
for those who require long-term nasogastric tube
feeding or a gastrostomy. Its use is nonetheless
restricted by the need to keep a nasal catheter in
place for at least 24 hours. This can cause great
discomfort and may be poorly tolerated by children,
especially those with behavioural issues. Wireless pH
monitoring can improve patient satisfaction and the
overall sensitivity of diagnosing gastroesophageal
reflux (Fig 1). Despite its rising popularity among
adults, its use has been limited in children. This
report documents the first experience in Hong Kong
of a wireless oesophageal pH monitoring system in
children with gastrointestinal symptoms and feeding
problems.
Case presentations
Case 1
A 9-year-old girl with good previous health and normal development presented to a surgical clinic
in March 2023 with recurrent epigastric pain and
heartburn. She was prescribed a proton pump
inhibitor without symptom improvement. As her
parents were keen to determine the cause of her
symptoms, upper endoscopy and a pH study were
offered. With consideration of patient comfort and
the sensitivity of the test, wireless oesophageal pH
monitoring was arranged. Endoscopy under general
anaesthetic revealed mild antral gastritis but was
otherwise unremarkable. An antral biopsy confirmed
mild gastritis without Helicobacter pylori. The
oesophagogastric junction (OGJ) was measured as
34 cm from the incisor, and a wireless pH monitoring
capsule (Bravo; Medtronic Inc, Minneapolis [MN],
United States) was inserted at 30 cm under direct
endoscopic visualisation (Fig 2a). Post-insertion
endoscopy confirmed secure placement at a
satisfactory position (Fig 2b). An X-ray after the
procedure further confirmed the good position of
the capsule (Fig 2c). pH monitoring lasted 96 hours,
with a DeMeester score of 6.8. The girl initially
complained of mild chest discomfort and a globus
sensation during swallowing on the first 2 days post
procedure but this resolved spontaneously after 4
days. The capsule passed spontaneously within 3
weeks of the procedure. The diagnosis of gastritis
was made after excluding gastroesophageal reflux by
pH monitoring; the patient was prescribed a short
course of a proton pump inhibitor that resolved the
symptoms.
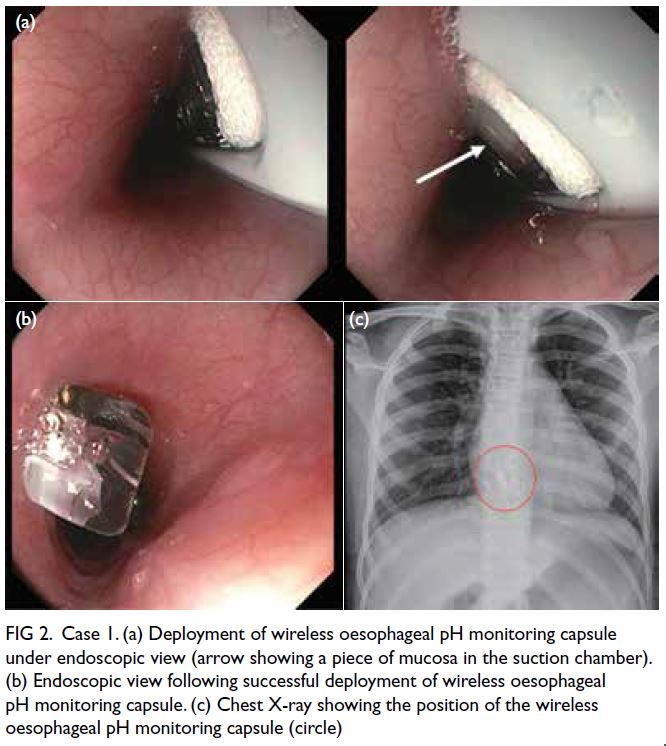
Figure 2. Case 1. (a) Deployment of wireless oesophageal pH monitoring capsule under endoscopic view (arrow showing a piece of mucosa in the suction chamber). (b) Endoscopic view following successful deployment of wireless oesophageal pH monitoring capsule. (c) Chest X-ray showing the position of the wireless oesophageal pH monitoring capsule (circle)
Case 2
A 6-year-old girl with known glucose phosphate
isomerase deficiency, cerebral ataxia and mild
intellectual impairment presented to the same surgical
clinic in January 2023. She had feeding problems
with failure to thrive and needed supplemental milk
feeding via a nasogastric tube. Given her medical
background and neurodevelopment, she could not
tolerate nasogastric tube insertion during her regular
revision and required frequent sedation during the
procedure. Owing to the anticipated requirement
for long-term tube feeding, her parents were advised
of the need for gastrostomy tube insertion and a preoperative pH study. As both the patient and
parents could not accept a conventional 24-hour pH
study, a wireless oesophageal pH monitoring system
was inserted under monitored anaesthetic care. The
upper endoscopy was unremarkable with no sign of
oesophagitis or gastritis. Bravo was inserted at 25 cm
from the incisor (ie, 5 cm from the OGJ). Monitoring
continued for 96 hours, with a DeMeester score of
0.7. The capsule passed without any complications
within 3 weeks of the procedure. The patient was
well and there were no adverse events during the
study period. In view of the negative pH study, an
anti-reflux procedure was deemed unnecessary and
subsequently only a laparoscopic gastrostomy was
performed.
Case 3
A 16-year-old boy with recurrent postprandial
heartburn and vomiting presented to the same
surgical clinic in March 2024. Medical treatment with
proton pump inhibitors elicited no improvement
and he was referred for work-up for an anti-reflux
procedure. At the time of referral, as capsule pH
monitoring was not available locally, a catheter-based
24-hour pH-impedance probe was attempted.
Nonetheless the patient could not tolerate the
procedure with repeated vomiting and failure of catheter insertion. Given the parents’ wish to have
a definitive diagnosis prior to initiating an anti-reflux
procedure, pH study was rearranged with the
wireless oesophageal pH monitoring system under
monitored anaesthesia care. The procedure was
well tolerated and the patient was able to complete
a 96-hour pH study. The overall DeMeester score
was 16.1. During the study period, Day 2 was the
patient’s worst day, with acid exposure time at 5.9%
and DeMeester score at 22.1. There was significant
improvement following resumption of a proton
pump inhibitor on Day 3 with acid exposure time at
1% and DeMeester score at 3.5. With the diagnosis
of significant gastroesophageal reflux disease
confirmed, the parents agreed to proceed with
laparoscopic fundoplication.
Discussion
According to the joint updated guidelines of the North
American Society for Pediatric Gastroenterology,
Hepatology and Nutrition and the European Society
for Paediatric Gastroenterology, Hepatology and
Nutrition in 2018,1 24-hour pH monitoring is
indicated in children with persistent symptoms of
gastroesophageal reflux disease despite proton pump
inhibitor treatment. The aim is to correlate persistent
troublesome symptoms with acid gastroesophageal
reflux events, clarifying the role of acid reflux
and determining the efficacy of acid suppression
therapy.1 Twenty-four–hour pH monitoring is
also recommended as pre-gastrostomy work-up in
children to guide patient selection for a concomitant
anti-reflux procedure.2 Nonetheless conventional
transnasal catheter pH monitoring, although still
widely used, is frequently criticised for causing great
patient discomfort, limiting the patient’s mobility
during the test and, more importantly, being neither
tolerable nor inducing compliance by children with
neurodevelopmental and behavioural issues,3 as
illustrated by Case 2. Not only is the quality of life of
patients jeopardised, the unpleasant experience may
also restrict reflux-provoking activities, limiting the
accuracy and sensitivity of the test and yielding false
lower values, as illustrated by Case 3.
To overcome these difficulties, the wireless
oesophageal pH monitoring system uses a capsule
attached to the mucosal wall of the oesophagus for
pH monitoring (Fig 1). It consists of a 6.0×6.3×26.0
mm3 capsule-based device, equipped with an
internal battery and a pH electrode. The device
is attached to the distal wall of the oesophagus,
approximately 4 to 6 cm from the OGJ, under direct
endoscopic visualisation.3 4 It transmits pH data to
a mobile phone–sized recorder via radio telemetry,
thus obviating the need for a transnasal pH probe.
The capsule enables data to be recorded for at
least 48 hours and up to 96 hours, with minimal
patient discomfort. The capsule detaches from the oesophageal mucosa and is expelled in stools, with
spontaneous sloughing of the oesophageal mucosa
and uneventful healing, usually over 3 to 7 days.
Its clinical use in children has been established
in the United Kingdom and the United States,
demonstrating a high success rate, with better
tolerance than standard transnasal pH monitoring in
children with behavioural issues and an improvement
in the detection rate of gastroesophageal reflux
disease by 16% through extended recording time.3 4
As illustrated by Case 3, not only is the procedure
tolerated, the successful extension of study for
a duration of 96 hours may result in a higher
diagnostic yield and provision of more information,
eg, effect of pump on and off (whether patient
was on proton pump inhibitor).5 Currently, the
wireless pH monitoring system is intended to be
used in adults and children from 4 years of age but
is contraindicated in those with bleeding diathesis,
strictures, severe oesophagitis, varices, obstructions,
pacemakers or implantable cardiac defibrillators.
In situations where the wireless pH capsule needs
to be removed, for instance in patients with severe
discomfort or failure of spontaneous passage, cold
snare and hot snare (when cold snare is not sufficient)
can be applied to safely remove the capsule with only
thin superficial oesophageal mucosal tissue.6
To the best of our knowledge, our centre is the
first to introduce and report the use of the wireless
oesophageal pH monitoring system in children in
Hong Kong. The procedure was smooth, with no
equipment or technical failure, and all patients could
be discharged on the same day of the procedure. Since
Case 1 was the first patient at our centre to receive the
device, a chest X-ray was taken to double confirm its
position. Nonetheless a post-procedure chest X-ray
is not routine for the paediatric population since the
device position can be confirmed with endoscopy, as
in the adult population. All patients tolerated the pH
study well except for the complaint of a self-limiting
globus sensation in one patient (Case 1). All parents
reported no difficulty in utilising the mobile pH
recording system. All capsules were expelled from
the patients within 3 weeks of the procedure without
any complication.
Wireless oesophageal pH monitoring cannot
easily diagnose some conditions such as functional
belching and rumination syndrome due to the
lack of impedance monitoring. Nonetheless these
cases highlight that it is well tolerated and feasible
in evaluating gastroesophageal reflux symptoms
in children and provides a sensible alternative to
standard transnasal pH monitoring. In addition,
it may result in a higher diagnostic yield and more comprehensive clinical information. As clinicians,
we are obliged to keep track of technological
advancements and strive to provide holistic
and optimal care for children, improve patient
satisfaction and shorten their hospital stay.
Author contributions
Both authors contributed to the concept or design, acquisition
of data, analysis or interpretation of data, drafting of the
manuscript and critical revision of the manuscript for
important intellectual content. Both authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
As an editor of the journal, KKY Wong was not involved in the peer review process. The other author has disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patients were treated in accordance with the Declaration of Helsinki. Verbal consent was obtained from the patients for the publication of the case reports.
References
1. Rosen R, Vandenplas Y, Singendonk M, et al. Pediatric
Gastroesophageal Reflux Clinical Practice Guidelines:
Joint Recommendations of the North American Society
for Pediatric Gastroenterology, Hepatology, and Nutrition
and the European Society for Pediatric Gastroenterology,
Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr
2018;66:516-54. Crossref
2. Fung AC, Ooi YN, Hui HM, Mok MK, Chung PH, Wong KK.
Prophylactic anti-reflux procedure for children undergoing
laparoscopic gastrostomy: rethinking of the routine
practice. World J Surg 2024;48:739-45. Crossref
3. Rodriguez L, Morley-Fletcher A, Winter H, Timothy B.
Evaluation of gastroesophageal reflux disease in children
on the autism spectrum: a study evaluating the tolerance
and utility of the BRAVO wireless pH monitoring. J Pediatr
Gastroenterol Nutr 2022;75:450-4. Crossref
4. Rao NM, Campbell DI, Rao P. Two years’ experience of
using the Bravo wireless oesophageal pH monitoring
system at a single UK tertiary centre. Acta Paediatr
2017;106:312-5. Crossref
5. Zeki SS, Miah I, Visaggi P, et al. Extended wireless pH
monitoring significantly increases gastroesophageal reflux
disease diagnoses in patients with a normal pH impedance
study. J Neurogastroenterol Motil 2023;29:335-42. Crossref
6. de Hoyos A, Esparza EA, Loredo ML. Cold and hot snare
endoscopic techniques for removal of the Bravo pH
monitoring capsule. Digestion 2009;79:14-6. Crossref