Hong Kong Med J 2025 Feb;31(1):9–11 | Epub 7 Feb 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
Clinical errors and mistakes: civil or criminal
liability?
Albert Lee, MD, LLM1,2,3,4; Monique A Anawis, MD5; JD, Roy G Beran, MD, FRACP6,7,8; Tracy Cheung, LLB, PCLL9,10; Calvin Ho, LLM, JSD2,11; Hwan Kim, LLM, CPCU12
1 Emeritus Professor, The Jockey Club School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Centre for Medical Ethics and Law, Faculties of Law and Medicine, The University of Hong Kong, Hong Kong SAR, China
3 Adjunct Professor, International Centre for Future Health System, University of New South Wales, Sydney, Australia
4 Vice President (Asia), World Association for Medical Law, United States
5 Clinical Assistant Professor of Ophthalmology, Northwestern University Feinberg School of Medicine, Chicago, United States
6 Conjoint Professor, South Western Sydney Clinical School, University of New South Wales, Sydney, Australia
7 Conjoint Professor, Western Sydney University, Sydney, Australia
8 Professor, Griffith University, Gold Coast, Australia
9 Consultant, Wanda Tong & Co, Hong Kong SAR, China
10 Lecturer, School of Law, City University of Hong Kong, Hong Kong SAR, China
11 Associate Professor, Faculty of Law, Monash University, Melbourne, Australia
12 Senior Vice President, Healthcare Division (Asia Pacific), Allied World Assurance Company
Corresponding author: Dr Albert Lee (alee@cuhk.edu.hk); Ms Tracy Cheung (tracycheung@bosc.com.hk)
Civil liability of doctors arises when there is a
clinically negligent act or omission resulting in harm
as a consequence of a doctor not meeting the standard
of care as expected from reasonable medical practice
or failure to warn.1 Do clinical errors and mistakes
necessarily equate to negligence? The essential
elements required to establish negligence, are: (1)
the existence of a duty of care owed to the patient;
(2) a breach of duty as determined by standard of
care; (3) the patient has experienced harm; and (4) a
causal connection, between the defendant’s careless
act and the resulting damage incurred with the
damage considered foreseeable and not too remote.2
In Hatcher v Black,3 Lord Denning explained a case
that a woman P, who suffered side-effects from
an operation on her throat and sued the surgeon
concerned. Denning J stated that:
“…on the road or in a factory there ought not to be any accidents if everyone used proper care, but in a hospital there was always a risk. It would be disastrous to the community if a doctor examining a patient or operating at the table, instead of getting on with his work, were forever looking over his shoulder to see if someone was coming up with a dagger. The jury should not find the defendant negligent simply because one of the risks inherent in an operation actually took place, or because in a matter of opinion he made an error of judgement. They should find him liable only if he had fallen short of the standard of medical care, so that he was deserving of censure…”
(The jury found in favour of the defendant).
“…on the road or in a factory there ought not to be any accidents if everyone used proper care, but in a hospital there was always a risk. It would be disastrous to the community if a doctor examining a patient or operating at the table, instead of getting on with his work, were forever looking over his shoulder to see if someone was coming up with a dagger. The jury should not find the defendant negligent simply because one of the risks inherent in an operation actually took place, or because in a matter of opinion he made an error of judgement. They should find him liable only if he had fallen short of the standard of medical care, so that he was deserving of censure…”
(The jury found in favour of the defendant).
According to the Bolam test,4 “a doctor will not
be found negligent if he/she has acted in accordance
with a practice accepted as proper by a reasonable body of medical opinion”. It appears unreasonable or
of limited social value to impose a criminal sanction
on a medical practitioner for genuine clinical errors
and mistakes.
The majority of litigation, following alleged
medical malpractice, is brought under the tort of
negligence (civil claims) and the remedy sought is
monetary compensation. Criminalisation of medical
malpractice falls into the realm of retributive justice
which is a system of criminal justice focusing solely
on punishment, rather than deterrence or the
rehabilitation of offenders. The punishment should
be in proportion to the seriousness of the crime
committed.5 The negligent act should be culpable to
constitute a criminal act, such as gross negligence
manslaughter (GNM).6 This raises pertinent issues
and questions in health care, such as: Is criminal
prosecution really promoting patient safety and
safeguarding public interest? Should the focus be
on conduct rather than outcome? Should the use of
restorative justice, emphasising retribution, surpass
deterrence and rehabilitation?7
An expert panel conducted a pre-recorded
seminar, followed by an interactive panel, to analyse
GNM, in the healthcare setting, across different
common law jurisdictions (including Australia,
England, Hong Kong, Singapore and the United
States) in November 2021.8 A paper is under
preparation which reports the critical points of those
presentations, together with further analyses of cases
and literature in jurisdictions adopting common law,
to provide a better understanding of how clinical
negligence might lead to criminal proceedings.
This editorial aims to recap the English case of Bawa-Garba,9 to discuss the factors to be taken
into consideration for medical crime. There were a
number of high-profile criminal investigations and
prosecutions of healthcare professionals (HCPs)
in England, with no offence recorded in Scotland
and only 14 HCPs being charged with offences of
criminal negligence in Canada and just over 30
GNM prosecutions since 1830 in England.7
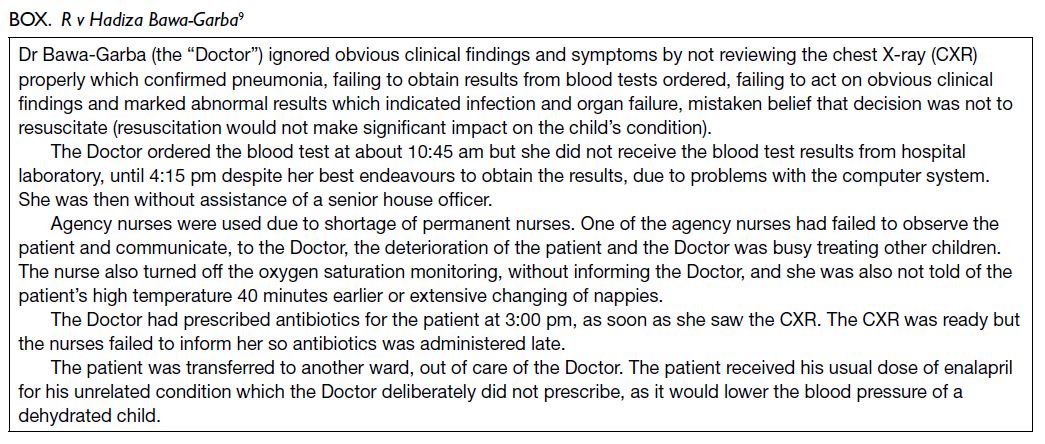
In the Garba case,9 the jury found the defendant
paediatrician’s conduct to be “truly exceptionally
bad” (meaning it was far below the standard of care
expected by a competent paediatrician and that it
amounted to the criminal offence of GNM). The
literature has raised criticisms of the findings for
failing to give due consideration to organisational
factors, such as system failure or lack of permanent
supporting staff.6 10 The Box summarises the
negligence of the defendant doctor and factors
contributing to her negligence.
The investigations and prosecutions regarding
Garba were perceived as arbitrary and inconsistent.11
This resulted in a rapid policy review, as described
in Gross Negligence Manslaughter in Healthcare in
2018.12 The panel was clear that HCPs could not be,
or be seen to be, above the law and should be held to
account where necessary. It was equally evident that
HCPs are working in the complexity of a modern
healthcare system, under a stressful environment
and this should also be taken into consideration when
deciding whether to pursue a GNM investigation.
Doctors who have made an erroneous or suboptimal
decision, without the intent to harm, acted in a
manner that arguably does not rise to the level of
criminal blameworthiness.13
A negligent doctor should not be held
criminally liable for a brief lapse of concentration or
an inadvertent error of judgement and it has been
argued that three factors: (1) awareness; (2) choice
(choose to run the risk); and (3) control (has the opportunity to act differently) should be present
for the establishment of the negligent conduct to be
considered culpable within the criminal context.13 An
error is trying to do the right thing but performing
same wrongly which does not reflect an intentional
deviation from accepted practices.14
Would Garba9 be ruled differently, with
consideration of culpability and violation of the three
factors of awareness, choice and control? Dr Bawa-Garba’s fitness to practise had been found to be
impaired causing her suspension from practising for
1 year by the tribunal. The General Medical Council
appealed, on the ground that the tribunal should
have ordered her to be erased from the register
and substituted the sanction of erasure for that
of suspension.15 The ruling led to a backlash from
doctors who believed that she should not have been
singled out for punishment because of the multiple
system failures which led to the boy’s death. Dr Bawa-Garba finally won an appeal against being struck off,
restoring the 1-year suspension.16 The judgement
states that the task of the tribunal was to decide
what sanction would “most appropriately meet the
overriding objective of protecting the public.”16 Taking
into account the particular circumstances of this
case and the aggravating and mitigating factors, the
Court of Appeal felt that erasure was not necessary
to meet the objectives of: protecting the public;
maintaining public confidence; and promoting and
upholding proper professional standards. The Court
considered that the expert tribunal was entitled to
form the view that a suspension order could meet
these statutory objectives.
Dr Bawa-Garba is now back at work and has
finished her specialist training.17 The main lessons
learned are: to analyse all circumstances; to assess
whether the negligent act is truly exceptionally bad;
and whether there were extenuating circumstances
that need to be taken into account.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: A Lee, T Cheung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: A Lee, T Cheung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Declaration
This editorial has been presented in the Gross Negligence
Manslaughter Seminar and Panel Discussion: Reflection from
different Jurisdictions adopting Common Law organised by
the Centre for Health Education and Health Promotion of The
Chinese University of Hong Kong and co-organised by the
Centre for Medical Ethics and Law of The University of Hong
Kong, New Medico-Legal Society of Hong Kong, American
College of Legal Medicine, the Australasian College of Legal
Medicine, and the Healthcare Division of Allied World
Assurance Company held in November 2021.
Funding/support
This editorial received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Disclaimer
The opinions expressed reflect the views of the authors not the institutions to which they are affiliated.
References
1. Lee A. Clinical liability in Hong Kong: revisiting duty and
standard of care. In: Raposo VL, Beran RG, editors. Medical
Liability in Asia and Australasia. Ius Gentium: Comparative
Perspectives on Law and Justice, vol 94. Singapore: Springer; 2022. Crossref
2. Jones M, Dugdale AM, Simpson M. Clerk & Lindsell on Torts. 23rd Edition, London: Sweet & Maxwell; 2020.
3. Bolam v Friern Hospital Management Committee. 1 WLR 582; 1957.
4. Hatcher v Black. The Times. 2 July 1954.
5. Meyer JF. Retributive Justice. Encyclopedia Britannica, 12 Sep 2014. Available from: https://www.britannica.com/topic/retributive-justice. Accessed 6 Jan 2024.
6. Lee A. Key elements of gross negligence manslaughter in
the clinical setting. Hong Kong Med J 2023;29:99-101. Crossref
7. Farrell AM, Alghrani A, Kazarian M. Gross negligence
manslaughter in healthcare: time for a restorative justice
approach? Med Law Rev 2020;28:526-48. Crossref
8. Anawis M, Beran RG, Cheung T, Ho C, Kim H, Lee A. Gross
Negligence Manslaughter Seminar and Panel Discussion:
Reflection from different Jurisdictions adopting Common
Law. November 2021. Available from: https://www.chep.cuhk.edu.hk/GNM/. Accessed 15 Jan 2024.
9. R v Hadiza Bawa-Garba. EWCA Crim 1841; 2016.
10. Cohen D. Back to blame: the Bawa-Garba case and the
patient safety agenda. BMJ 2017;359:j5534. Crossref
11. Lee DW, Tong KW. What constitutes negligence and gross
negligence manslaughter? In Chiu JS, Lee A, Tong KW,
editors. Healthcare Law and Ethics: Principles and Practices.
Hong Kong: City University of Hong Kong Press; 2023.
12. Department of Health and Social Care of the United
Kingdom. Gross Negligence Manslaughter in Healthcare.
The Report of a Rapid Policy Review. June 2018. Available
from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/717946/Williams_Report.pdf . Accessed 25 Jan 2025.
13. Robson M, Maskill J, Brookbanks W. Doctors are
aggrieved—should they be? Gross negligence manslaughter
and the culpable doctor. J Crim Law 2020;84:312-40. Crossref
14. Merry A, Brookbanks W. Violations. In: Merry and
McCall Smith’s Errors, Medicine and the Law. 2nd Edition.
Cambridge: Cambridge University Press; 2017: 141-82. Crossref
15. GMC v Dr Bawa-Garba. EWHC 76 (Admin); 2018.
16. Hadiza Bawa-Garba v GMC. EWCA Civ 18979; 2018.
17. Dyer C. Hadiza Bawa-Garba can return to practice under close supervision. BMJ 2019;365:l1702. Crossref