Hong Kong Med J 2025;31:Epub 24 Jan 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PERSPECTIVE
Incorporating the cardiovascular-kidney-metabolic
health framework into the local healthcare system: a position statement from the Hong Kong College of Physicians
CH Lee, MB, BS, MD1; G Tan, MBChB2; Sydney CW Tang, MB, BS, MD3 #; YW Ng, MBChB4 #; Michael KY Lee, MB, BS5 #; Johnny WM Chan, MB, BS6 #; TM Chan, MB, BS, DSc7 #
1 Division of Endocrinology and Metabolism, Department of Medicine, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Queen Mary Hospital, Hong Kong SAR, China
2 Division of Cardiology, Department of Medicine and Therapeutics, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
3 Division of Nephrology, Department of Medicine, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Queen Mary Hospital, Hong Kong SAR, China
4 Division of Endocrinology, Department of Medicine, Queen Elizabeth Hospital, Hong Kong SAR, China
5 Division of Cardiology, Department of Medicine, Queen Elizabeth Hospital, Hong Kong SAR, China
6 Division of Respiratory Medicine, Department of Medicine, Queen Elizabeth Hospital, Hong Kong SAR, China
7 Division of Nephrology, Department of Medicine, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
# Steering Committee of the Hong Kong College of Physicians position statement
Corresponding authors: Prof Sydney CW Tang (scwtang@hku.hk), Prof TM Chan (dtmchan@hku.hk)
Introduction
What is cardiovascular-kidney-metabolic
syndrome?
Cardiovascular-kidney-metabolic (CKM) syndrome
is a new entity that emphasises interconnections
among atherosclerotic cardiovascular disease
(ASCVD), atrial fibrillation (AF), heart failure
(HF), chronic kidney disease (CKD), excess
adiposity, metabolic syndrome, and diabetes.1 It is
categorised into five stages (Table 1), reflecting the
progressive nature of the pathophysiology behind
this multifaceted syndrome and the increasing risk
of adverse cardiovascular outcomes associated with
higher CKM stages.2 3 4 5 6 The CKM health framework
incorporates screening, staging, and management
for early identification of potential CKM-related
events.7 8
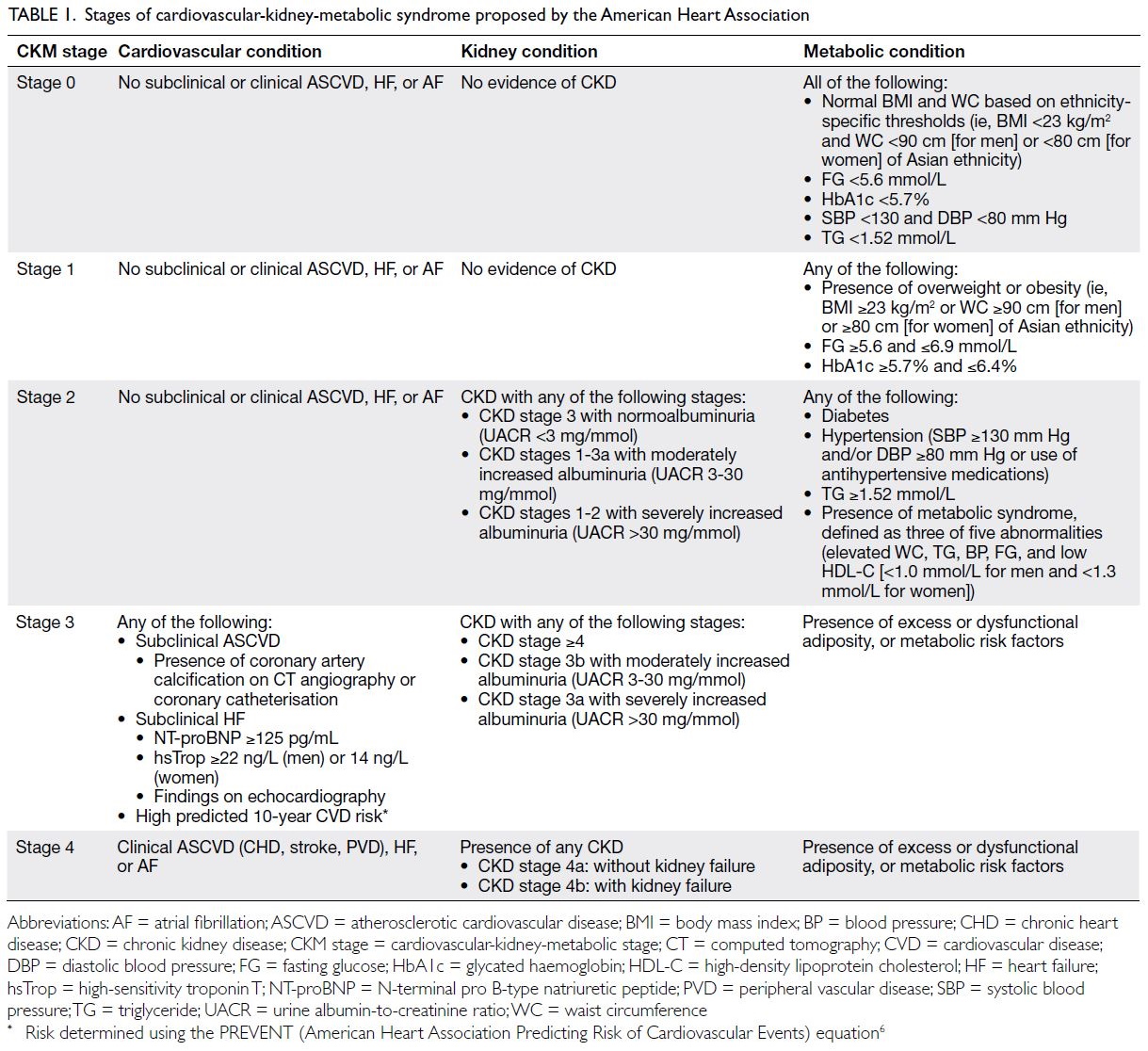
Table 1. Stages of cardiovascular-kidney-metabolic syndrome proposed by the American Heart Association
Adaptation of the CKM model is influenced by
access, financing, and care delivery. A multispecialty
working group of the Hong Kong College of
Physicians (HKCP) developed this Position
Statement concerning incorporation of the CKM
health framework into the local healthcare system,
taking into consideration local healthcare needs,
existing resources and limitations, as well as future
healthcare directions and initiatives in Hong Kong.
Patient care challenges in real-world settings
The CKM concept aims to identify individuals at risk for suboptimal CKM health to enable
timely intervention and slow disease progression.
Optimal care delivery remains challenging despite
improvements in local health literacy. A recent
local population health survey revealed that many
individuals were unaware of overweight or obesity
status, as well as hypertension, diabetes, and elevated
cholesterol.9
The ageing local population (~21% of
individuals are aged ≥65 years10) further strains
healthcare resources due to increasing numbers
of patients with CKM risks, as well as end-organ
damage. A lack of public awareness about CKM
health and limitations in primary healthcare
constitute barriers to implementing the CKM health
framework.
The Hospital Authority has largely focused on
specialist care, while our primary healthcare system
is comparatively underdeveloped.11 Public health expenditures reflect this focus.12 The Health Bureau’s
Primary Healthcare Blueprint (2022) and the 3-year
Chronic Disease Co-Care (CDCC) Pilot Scheme
are promising initiatives, but their integration with
specialist care remains unclear.
Screening
Screening asymptomatic individuals for metabolic
risk factors (eg, overweight/obesity, central adiposity,
dysglycaemia, hypertension, and dyslipidaemia) is
a key component of the CKM health framework. For adults aged ≥21 years, this includes annual
measurements of body mass index (BMI) and waist
circumference, along with periodic assessments
of blood pressure (BP), lipid levels, and glycaemic
status. Screening intervals depend on CKM stage:
every 3-5 years for CKM stage 0 (healthy and lean),
every 2-3 years for CKM stage 1 (overweight/obese
or prediabetes), and annually for CKM stage 2
(diabetes, hypertension, or hypertriglyceridaemia).1
These recommendations align with the American
Diabetes Association’s guidance that asymptomatic
adults aged ≥35 years, or overweight/obese adults
with risk factors—such as physical inactivity, family
history of diabetes, hypertension, high triglyceride levels, or polycystic ovarian syndrome—undergo
screening for prediabetes or diabetes every 3
years if no abnormalities are detected.13 The need
for triglyceride screening remains unclear, and
discussions continue regarding BMI thresholds for
overweight/obesity in Asian populations.14
The CDCC Pilot Scheme, launched by the
Hong Kong SAR Government in November 2023,
offers subsidised screening in the private sector for
residents aged ≥45 years without known diabetes or
hypertension.15 Initial assessments include BP and
glycated haemoglobin), with follow-up tests (lipid
profile, estimated glomerular filtration rate [eGFR],
urinalysis) if hypertension or diabetes is detected. Blood pressure thresholds for hypertension vary
across guidelines.16 17 The HKCP previously endorsed
defining hypertension as BP ≥140/90 mmHg18;
the CKM framework utilises a lower threshold
of 130/80 mmHg based on recent evidence.
Home BP monitoring and standardised office BP
measurements are both acceptable. Early detection of
CKM risk factors aligns with the Primary Healthcare
Blueprint,19 which promotes chronic disease
prevention through a family-centric, community-based
primary care system. A key concept, “family
doctor for all,” aims to enhance public access to care,
including screening and diagnosis of prediabetes,
early diabetes, and hypertension via coordination
with family doctors in the Primary Care Register.
Timely screening and intervention can reduce
complications such as CKD, cardiovascular disease
(CVD), and hospitalisations.
Roles of physician specialists and primary
care doctors in the cardiovascular-kidney-metabolic
health framework
The increasing incidence of kidney failure and
growing healthcare burden of CKD, which now
affects 10% of the global population, have made
CKD an international health priority. Nephrologists
play a central role in managing individuals across
CKM stages. Chronic kidney disease substantially
increases risks of cardiovascular morbidity and
mortality; many patients, especially those aged ≥75
years, die of CVD before exhibiting kidney failure
or requiring dialysis.20 Among dialysis patients
in Hong Kong, CVD and stroke caused 30.3% of
deaths in 2022.21 Diabetes or hypertension was the
primary diagnosis for 63% of patients initiating
kidney replacement therapy. Early CKD detection,
particularly in at-risk individuals, allows preventive
measures during asymptomatic stages. Primary care
doctors are needed to identify and manage these
individuals.
Cardiovascular risk factors, including CKD,
often remain unrecognised until disease becomes
clinically apparent. The CKM staging system
prioritises early detection of cardiovascular risk
factors, recommending eGFR and urine albumin-to-creatinine
ratio assessments for at-risk individuals,
such as those with hypertriglyceridaemia, metabolic
syndrome, diabetes, hypertension (stage ≥2), or
clinical CVD. Indeed, evaluation of albuminuria
should also be considered in CKM stage 1,
characterised by obesity or dysfunctional adiposity,
which manifests as prediabetes—both risk factors
for CKD.22 23 These recommendations aim to
improve kidney health awareness and promote
CKD screening among primary care doctors, family
physicians, and specialists, who are often the first to
encounter patients in early stages of CKM.
The Predicting Risk of CVD Events (PREVENT) equation from the American Heart
Association is recommended to assess 10-year CVD
risk in asymptomatic individuals without ASCVD
or HF. This tool estimates overall CVD risk and
guides preventive therapy initiation.6 Caution is
needed because the equation may overestimate risk
in individuals of Asian descent.24 25 The PREVENT
equation is preferred over the Pooled Cohort
Equations26 in the CKM framework27 because it
includes CKM-specific factors that constitute novel
CVD risk factors. Although the social deprivation
index is specific to the United States, the inclusion
of socioeconomic background during CVD risk
estimation is relevant in Hong Kong. The risk score
can be calculated using the online tool provided by
the American Heart Association.28 The PREVENT
equation, designed for primary prevention in
individuals aged 30-79 years without coronary heart
disease, stroke, or HF, helps tailor patient-centred
preventive therapies according to guidelines.26 29
Coronary artery calcium (CAC) testing is
recommended for further CVD risk stratification and
statin use guidance during primary prevention.26 27
However, routine CAC testing is not advised in
Hong Kong for CKM screening or staging due to
concerns about increased downstream testing and
the lack of a structured follow-up programme. When
CAC results are available, even for asymptomatic
individuals, they should inform CKM staging and
guide therapies following established guidelines.26 27 29
The CKM framework proposes testing for
B-type natriuretic peptide (BNP),27 N-terminal
pro-BNP, or high-sensitivity troponin in at-risk
individuals to detect subclinical HF.27 Although two
randomised studies demonstrated the utility of this
approach for guiding renin-angiotensin-aldosterone
system-modifying agent therapy,30 31 routine cardiac
biomarker testing in asymptomatic individuals is
not recommended within Hong Kong. Angiotensin-converting
enzyme inhibitors (ACEi) are already
recommended as first-line therapy, particularly for
patients with diabetes,32 and local cost-effectiveness
data are unavailable. Furthermore, it can be
challenging to interpret BNP, N-terminal pro-BNP,
and troponin levels in moderate to advanced CKD
(a component of CKM syndrome) due to renal
excretion of these biomarkers. When available,
cardiac biomarker data should be considered
for management of HF medications with proven
benefits, even in asymptomatic individuals.33
Prevention of complications
The CKM health framework prioritises identifying
and treating CKM risk factors during the preclinical
phase to prevent clinical ASCVD, AF, HF, and
kidney failure. Locally, patients with hypertension
and diabetes in General Out-patient Clinics undergo
regular screening for complications through the RAMP (Risk Assessment and Management
Programs) for Hypertension and Diabetes,
respectively.34 35 Patients with diabetes in public
hospital clinics also undergo regular complications
screening, including cardiovascular risk assessments,
urine albumin-to-creatinine ratio testing, and, in
some centres, vascular Doppler studies.34 35 In the
private sector, the Health Bureau of Hong Kong has
established Reference Frameworks36 37 for diabetes
and hypertension care, highlighting the importance
of regular diabetic complications screening.
The incidences of CKD, metabolic diseases,
and obesity are rising, even in younger individuals;
greater emphasis on CKD prevention is needed,
particularly regarding screening methods and
timing. The CKM framework recommends CKD
screening before age 21 among individuals with
risk factors such as obesity, hypertriglyceridaemia,
diabetes, or hypertension. Although not widely
adopted locally, the HKCP supports earlier CKD
detection to improve kidney survival and quality
of life.38 Screening gaps exist for albuminuria in
high-risk groups, including overweight or obese
individuals and those with clinical CVD.
Because most patients in early stages of CKM
are asymptomatic, primary care and family doctors
play a central role in ensuring regular follow-up.
This role includes monitoring glycaemic status, lipid
profiles, and BP, along with surveillance for CKM
complications, such as CKD progression or clinical
CVD.
Clinical management: an interdisciplinary
care model in Hong Kong
The HKCP supports the guideline-directed
management approach in the CKM health
framework, although anthropometric thresholds
for interventions slightly differ due to population
variations. The BMI threshold for metabolic and
bariatric surgery was recently updated to ≥27.5 kg/m2
for Asian populations.39 This threshold also applies
the use of glucagon-like peptide-1 receptor agonists
(GLP1RAs) for obesity treatment in patients with
type 2 diabetes, aligning with the World Health
Organization’s recommended BMI action point
for high-risk individuals in Asian populations.40 If
pharmacotherapy cost constraints are addressed,
the threshold could be lowered to ≥25 kg/m2, as
indicated in some Asian guidelines.41 In Hong
Kong, access to newer CKM pharmacotherapies is
limited. Among GLP1RAs approved for managing
obesity in individuals without diabetes, only daily
liraglutide is currently available, whereas weekly
semaglutide is not. Icosapent ethyl, an omega-3
fatty acid treatment for hypertriglyceridaemia,
is unavailable in the public sector. The CKM
framework recommends initiating cardioprotective antidiabetic agents regardless of glycaemic control,
even before metformin in individuals with glycated
haemoglobin level <7.5%. However, affordability and
patient preferences may impact implementation.
Glycaemic control optimisation remains essential
because early and effective control improves
cardiorenal outcomes and reduces mortality.42
Notably, statin pharmacokinetics differ between
Chinese and Western populations43 44; rosuvastatin
dosages should not exceed 20 mg daily in Chinese
individuals due to rhabdomyolysis risk.
In CKM stage 4 (established CVD), recurrent
cardiovascular event risk is high, but many patients fail
to achieve the recommended low-density lipoprotein
cholesterol target of <1.8 mmol/L.45 Identification
of high-risk individuals and intensification of
lipid-lowering therapy with high-intensity statins,
ezetimibe, and proprotein convertase subtilisin/kexin type 9 inhibitors are needed to achieve
therapeutic goals.26 In patients with HF, particularly
those exhibiting reduced left ventricular ejection
fraction, guideline-directed medical therapy
(GDMT) classes—beta-blockers, angiotensin
receptor blockers (ARBs)/neprilysin inhibitors,
sodium-glucose co-transporter 2 inhibitors, and
mineralocorticoid receptor antagonists—should
be initiated and titrated appropriately.33 Among
patients with AF exhibiting CKM syndrome and
stroke risk factors, anticoagulation is advised.46 Co-morbidities
such as severe obesity and CKD should
be carefully considered because they may influence
direct oral anticoagulant efficacy.
Patients across all CKD and CVD stages47
should be evaluated for kidney-protective therapies,
many of which also provide cardiovascular benefits.
These include ACEi or ARBs, sodium-glucose
co-transporter 2 inhibitors, GLP1RAs, and the
nonsteroidal mineralocorticoid receptor antagonist
finerenone, as appropriate. Most patients should
receive an ACEi or ARB at the maximum tolerated
dose, with additional agents introduced based on
individual needs and tolerability. Goals include
optimising BP, reducing albuminuria, stabilising
eGFR, and lowering cardiovascular risk. Some
therapies may cause short-term haemodynamic
effects on kidney function or adverse effects, leading
to premature discontinuation. The CKM framework
emphasises initiation and maintenance of these
therapies. The HKCP supports their timely uptake
and continued use by specialists and primary care
physicians.
Implementation of the CKM health
framework in Hong Kong faces challenges, including
discrepancies in drug formularies between primary
care and specialty clinics and inadequate coordination
between these services. Patients are sometimes
referred to specialty clinics solely for medications
unavailable in primary care. Such referral increases waiting times at overburdened specialty clinics and
delays GDMT initiation. Follow-up intervals may
be extended due to heavy patient loads, impacting
treatment adherence and monitoring. The CDCC
Pilot Scheme provides targeted subsidies to support
the diagnosis and management of chronic diseases,
particularly hypertension and diabetes, in the
private sector. This co-care model aims to benefit
patients across various CKM stages and mitigate
complications.
Conclusions and the way forward
Cardiovascular-kidney-metabolic syndrome has
substantial implications for patients and society.
The HKCP emphasises the need for collaborative
interdisciplinary care within the CKM healthcare
framework, integrating primary care, specialist
care, and medical subspecialties to prevent
complications and protect organs. Although GDMT
ensures evidence-based care, clinicians must tailor
management to the unique characteristics of each
patient, addressing gaps in trial data and local
applicability. Conditions such as hyperglycaemia, dyslipidaemia, obesity, kidney insufficiency, and
hypertension should not be viewed as “risk factors”
but as chronic conditions requiring early intervention
to prevent CVD and CKD. Kidney health is central
to CKM syndrome, given the high prevalence of
kidney failure among patients with diabetes or CVD.
Considering the strengths and limitations
of the local healthcare system (Table 2), multiple
actions are needed to mitigate the increasing impact
of CKM syndrome. The public and healthcare
professionals must be educated regarding its
adverse effects and access to effective interventions.
Integrated care across primary and specialist
services is essential, supported by healthcare policy
focusing on organ protection to ensure coordination,
minimise duplication, and optimise resource use. A
collaborative care model involving all stakeholders
and providers is essential. The HKCP hopes
this position statement will raise awareness and
prompt timely strategies to address the growing
challenges of CKM syndrome, ultimately improving
cardiovascular, metabolic, and kidney health in the
community.
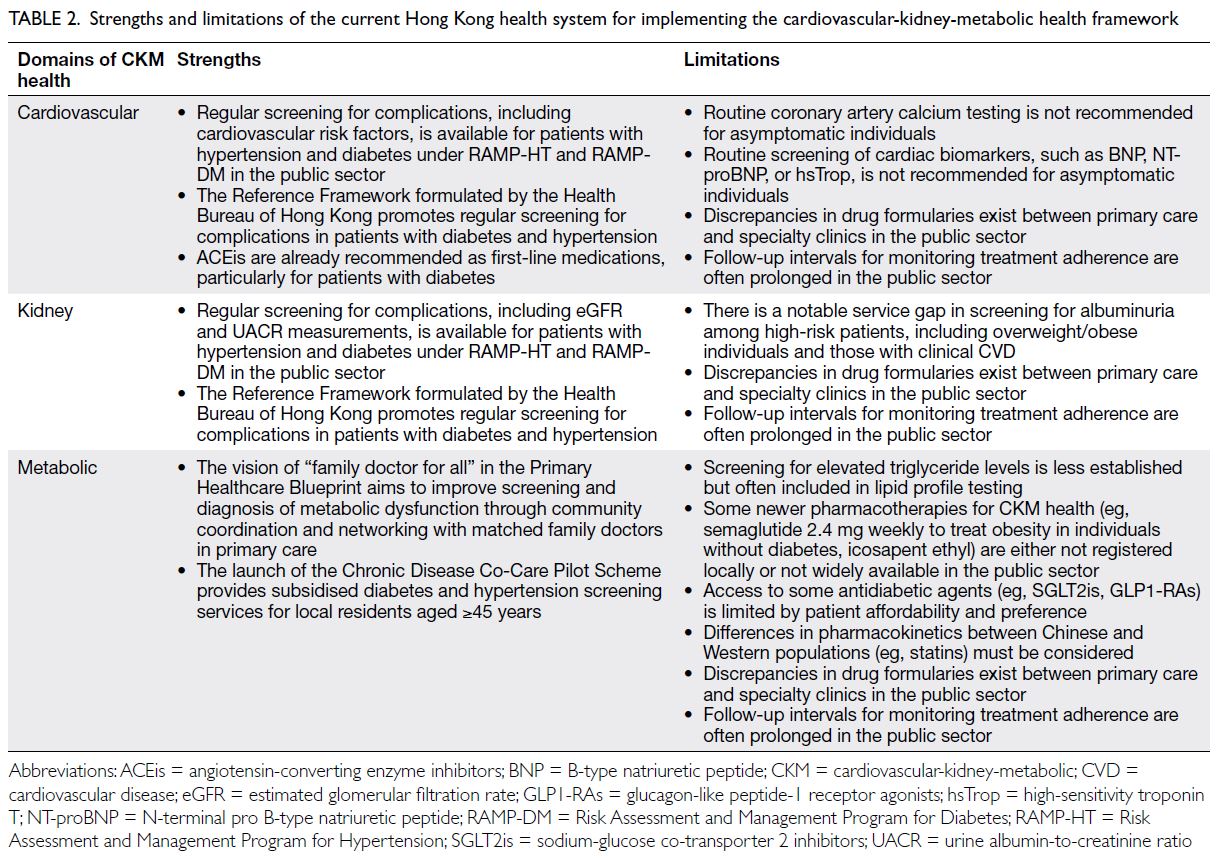
Table 2. Strengths and limitations of the current Hong Kong health system for implementing the cardiovascular-kidney-metabolic health framework
Author contributions
Concept or design: SCW Tang and TM Chan.
Acquisition of data: CHL, G Tan and SCW Tang.
Analysis or interpretation of data: CHL, G Tan, SCW Tang and TM Chan.
Drafting of the manuscript: CHL, G Tan and SCW Tang.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: CHL, G Tan and SCW Tang.
Analysis or interpretation of data: CHL, G Tan, SCW Tang and TM Chan.
Drafting of the manuscript: CHL, G Tan and SCW Tang.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
CH Lee has received advisory board and lecture honoraria
from AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly,
Gilead, GSK, Novo Nordisk, and Sanofi Aventis. SCW Tang
has reported consulting fees from Boehringer Ingelheim,
Novartis, and Travere Therapeutics, as well as speaker fees
from AstraZeneca, Baxter, Bayer, Boehringer Ingelheim/Eli Lilly, GSK, and Novartis. The other co-authors have no
competing interests relevant to this manuscript.
Funding/support
This position statement was not supported by any specific
grant from any funding agency in the public, commercial, or
not-for-profit sectors.
References
1. Ndumele CE, Rangaswami J, Chow SL, et al. Cardiovascularkidney-
metabolic health: a presidential advisory from the
American Heart Association. Circulation 2023;148:1606-35. Crossref
2. Fox CS, Matsushita K, Woodward M, et al. Associations
of kidney disease measures with mortality and end-stage
renal disease in individuals with and without diabetes: a
meta-analysis. Lancet 2012;380:1662-73. Crossref
3. Global Burden of Metabolic Risk Factors for Chronic
Diseases Collaboration (BMI Mediated Effects); Lu Y,
Hajifathalian K, et al. Metabolic mediators of the effects
of body-mass index, overweight, and obesity on coronary
heart disease and stroke: a pooled analysis of 97 prospective
cohorts with 1.8 million participants. Lancet 2014;383:970-83. Crossref
4. Shah AD, Langenberg C, Rapsomaniki E, et al. Type 2
diabetes and incidence of cardiovascular diseases: a cohort
study in 1.9 million people. Lancet Diabetes Endocrinol
2015;3:105-13. Crossref
5. Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and
cardiovascular disease: a scientific statement from the
American Heart Association. Circulation 2021;143:e984-1010. Crossref
6. Khan SS, Coresh J, Pencina MJ, et al. Novel prediction
equations for absolute risk assessment of total
cardiovascular disease incorporating cardiovascular-kidney-metabolic health: a scientific statement from the
American Heart Association. Circulation. 2023;148:1982-2004. Crossref
7. Nuffield Department of Population Health Renal Studies
Group; SGLT2 inhibitor Meta-Analysis Cardio-Renal
Trialists’ Consortium. Impact of diabetes on the effects
of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled
trials. Lancet 2022;400:1788-801. Crossref
8. Sattar N, Lee MM, Kristensen SL, et al. Cardiovascular,
mortality, and kidney outcomes with GLP-1 receptor
agonists in patients with type 2 diabetes: a systematic
review and meta-analysis of randomised trials. Lancet
Diabetes Endocrinol 2021;9:653-62. Crossref
9. Centre for Health Protection, Department of Health,
HKSAR Government. Report of Population Health Survey
2020-22. Available from: https://www.chp.gov.hk/files/pdf/dh_phs_2020-22_part_2_report_eng_rectified.pdf. Accessed 19 Apr 2023.
10. Health Bureau, Hong Kong SAR Government. Statistics:
major health related statistics of Hong Kong. Available
from: https://www.healthbureau.gov.hk/statistics/en/health_statistics.htm. Accessed 20 Dec 2024.
11. Pang FC, Lai SS. Establishment of the primary healthcare
commission. Hong Kong Med J 2023;29:6-7. Crossref
12. Health Bureau, Hong Kong SAR Government. Hong
Kong’s domestic health accounts 2019/20. Available from: . Accessed 23 Dec 2022.
13. American Diabetes Association Professional Practice
Committee. 2. Diagnosis and classification of diabetes:
standards of care in diabetes-2024. Diabetes Care
2024;47(Suppl 1):S20-42. Crossref
14. Bajaj SS, Zhong A, Zhang AL, Stanford FC. Body mass
index thresholds for Asians: a race correction in need of
correction? Ann Intern Med 2024;177:1127-9. Crossref
15. Health Bureau, Hong Kong SAR Government. Chronic
Disease Co-Care (CDCC) Pilot Scheme. Available from: https://www.primaryhealthcare.gov.hk/cdcc/en/. Accessed 25 Sep 2023.
16. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/
AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/
NMA/PCNA Guideline for the Prevention, Detection,
Evaluation, and Management of High Blood Pressure in
Adults: Executive Summary: A Report of the American
College of Cardiology/American Heart Association Task
Force on Clinical Practice Guidelines. J Am Coll Cardiol
2018;71:2199-269. Crossref
17. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH
Guidelines for the management of arterial hypertension.
Eur Heart J 2018;39:3021-104. Crossref
18. Chan KK, Szeto CC, Lum CC, et al. Hong Kong College of
Physicians Position Statement and Recommendations on
the 2017 American College of Cardiology/American Heart
Association and 2018 European Society of Cardiology/European Society of Hypertension Guidelines for the
Management of Arterial Hypertension. Hong Kong Med J
2020;26:432-7. Crossref
19. Health Bureau, Hong Kong SAR Government. The Primary
Healthcare Blueprint. Available from: https://www.primaryhealthcare.gov.hk/bp/en/index.html. Accessed 25 Sep 2023.
20. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY.
Chronic kidney disease and the risks of death,
cardiovascular events, and hospitalization. N Engl J Med
2004;351:1296-305. Crossref
21. Chan JY, Cheng YL, Yuen SK, et al. The Hong Kong Renal
Registry: a recent update. Hong Kong Med J 2024;30:332-6. Crossref
22. Tang SC, Wong AK, Mak SK. Clinical practice guidelines
for the provision of renal service in Hong Kong: general
nephrology. Nephrology (Carlton) 2019;24 Suppl 1:9-26. Crossref
23. Kar D, El-Wazir A, Delanerolle G, et al. Predictors and
determinants of albuminuria in people with prediabetes
and diabetes based on smoking status: A cross-sectional
study using the UK Biobank data. EClinicalMedicine
2022;51:101544. Crossref
24. Liu X, Shen P, Zhang D, et al. Evaluation of atherosclerotic
cardiovascular risk prediction models in China: results
from the CHERRY study. JACC Asia 2022;2:33-43. Crossref
25. Rodriguez F, Chung S, Blum MR, Coulet A, Basu S,
Palaniappan LP. Atherosclerotic cardiovascular disease
risk prediction in disaggregated Asian and Hispanic
subgroups using electronic health records. J Am Heart
Assoc 2019;8:e011874. Crossref
26. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/
AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/
NLA/PCNA Guideline on the management of blood
cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice
guidelines. J Am Coll Cardiol 2019;73:e285-350. Crossref
27. Ndumele CE, Neeland IJ, Tuttle KR, et al. A synopsis of
the evidence for the science and clinical management of
cardiovascular-kidney-metabolic (CKM) syndrome: a
scientific statement from the American Heart Association.
Circulation 2023;148:1636-64. Crossref
28. American Heart Association. The American Heart
Association PREVENTTM Online Calculator. Available from: https://professional.heart.org/en/guidelines-and-statements/prevent-calculator. Accessed 11 Jan 2024.
29. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular
disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice
guidelines. J Am Coll Cardiol 2019;74:e177-232. Crossref
30. Huelsmann M, Neuhold S, Resl M, et al. PONTIAC
(NT-proBNP selected prevention of cardiac events in a
population of diabetic patients without a history of cardiac
disease): a prospective randomized controlled trial. J Am
Coll Cardiol 2013;62:1365-72. Crossref
31. Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic
peptide-based screening and collaborative care for
heart failure: the STOP-HF randomized trial. JAMA
2013;310:66-74. Crossref
32. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection,
Evaluation, and Management of High Blood Pressure in
Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical
Practice Guidelines. J Am Coll Cardiol 2018;71:e127-248. Crossref
33. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart
Failure: Executive Summary: A Report of the American
College of Cardiology/American Heart Association Joint
Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022;79:1757-80. Crossref
34. Ng IH, Cheung KK, Yau TT, Chow E, Ozaki R, Chan JC.
Evolution of diabetes care in Hong Kong: from the Hong
Kong Diabetes Register to JADE-PEARL Program to
RAMP and PEP Program. Endocrinol Metab (Seoul)
2018;33:17-32. Crossref
35. Yu EY, Wan EY, Mak IL, et al. Assessment of Hypertension
Complications and Health Service use 5 years after
implementation of a multicomponent intervention. JAMA
Netw Open 2023;6:e2315064. Crossref
36. Primary Healthcare Commission, Health Bureau, Hong
Kong SAR Government. Diabetes Care. Available from:
https://www.healthbureau.gov.hk/pho/rfs/english/reference_framework/diabetes_care.html. Accessed 3 Apr
2024.
37. Primary Healthcare Commission, Health Bureau, Hong
Kong SAR Government. Hypertension Care. Available
from: https://www.healthbureau.gov.hk/phcc/rfs/english/reference_framework/hypertension_care.html. Accessed 3 Apr 2024.
38. Kula AJ, Prince DK, Katz R, Bansal N. Mortality burden
and life-years lost across the age spectrum for adults living
with CKD. Kidney360 2023;4:615-21. Crossref
39. Eisenberg D, Shikora SA, Aarts E, et al. 2022 American
Society for Metabolic and Bariatric Surgery (ASMBS) and
International Federation for the Surgery of Obesity and
Metabolic Disorders (IFSO): indications for metabolic and
bariatric surgery. Surg Obes Relat Dis 2022;18:1345-56. Crossref
40. WHO Expert Consultation. Appropriate body-mass index
for Asian populations and its implications for policy and
intervention strategies. Lancet 2004;363:157-63. Crossref
41. Lui DT, Ako J, Dalal J, et al. Obesity in the Asia-Pacific
region: current perspectives. J Asian Pac Soc Cardiol
2024;3:e21. Crossref
42. Khunti K, Zaccardi F, Amod A, et al. Glycaemic control is
still central in the hierarchy of priorities in type 2 diabetes
management. Diabetologia 2025;68:17-28. Crossref
43. Naito R, Miyauchi K, Daida H. Racial differences in the
cholesterol-lowering effect of statin. J Atheroscler Thromb
2017;24:19-25. Crossref
44. Tomlinson B, Chan P, Liu ZM. Statin responses in Chinese
patients. J Atheroscler Thromb 2018;25:199-202. Crossref
45. Sun H, Lai A, Tan GM, Yan B. Therapeutic gaps in low-density
lipoprotein cholesterol management have narrowed
over time but remain wide: a wide study of 40,141 acute
coronary syndrome patients from 2016 to 2021. Eur Heart
J 2023;44 (Suppl 2):ehad655-2800. Crossref
46. Writing Committee Members; Joglar JA, Chung MK,
et al. 2023 ACC/AHA/ACCP/HRS Guideline for the
Diagnosis and Management of Atrial Fibrillation: A
Report of the American College of Cardiology/American
Heart Association Joint Committee on Clinical Practice
Guidelines. J Am Coll Cardiol 2024;83:109-279. Crossref
47. Kidney Disease: Improving Global Outcomes CKD Work
Group. KDIGO 2024 clinical practice guideline for the
evaluation and management of chronic kidney disease.
Kidney Int 2024;105:S117-314. Crossref

