Hong Kong Med J 2024;30:Epub 18 Nov 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PERSPECTIVE
Mask-associated changes in ocular surface parameters
Victor TT Chan, MB, ChB1,2,3; Ka Wai Kam, MB, BS, FCOphthHK1,2,3; Wilson WK Yip, MB, ChB, FCOphthHK1,2,3; Alvin Lerrmann Young, MB, BCh, BAO, FHKAM (Ophthalmology)1,2,3
1 Department of Ophthalmology and Visual Sciences, Prince of Wales Hospital, Hong Kong SAR, China
2 Department of Ophthalmology and Visual Sciences, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
3 Department of Ophthalmology and Visual Sciences, Alice Ho Miu Ling Nethersole Hospital, Hong Kong SAR, China
Corresponding author: Prof Alvin Lerrmann Young (youngla@ha.org.hk)
Dry eye disease (DED) is a common, multifactorial
condition characterised by a loss of homeostasis on
the ocular surface. Although DED can be broadly
classified into aqueous-deficient and evaporative
subtypes, multiple mechanisms contribute to its
initiation and persistence.
The severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2) pandemic had adverse
effects on the ocular surface, with dry eye being the
most common ocular symptom.1 As a public health
measure, universal masking effectively reduced the
spread of the pandemic. Due to the increased use
of face masks during the pandemic, corresponding
increases in ocular irritation and dry eye symptoms
were observed among individuals who regularly
wore face masks, including those who had no prior
diagnosis of DED.2 The association between dry eye
and face mask use was first reported by Moshirfar
et al2 in 2020, using the term ‘mask-associated dry
eye’ (MADE). Since then, there have been reports
of increased dry eye symptoms and ocular surface
instability among individuals with regular mask use.
Therefore, we aimed to evaluate and summarise the
changes in symptoms and ocular surface parameters
after mask use among healthy individuals and
individuals with preexisting DED.
We conducted a literature search in PubMed
and Embase on 14 November 2022, using the
search strategy of ‘(dry eye) AND (mask)’ and
‘(keratoconjunctivitis sicca) AND (mask)’. We then
performed a meta-analysis using RevMan software
version 5.4 (The Cochrane Collaboration, London,
United Kingdom) to identify any ocular surface
parameters evaluated in at least three studies.
We used means and standard deviations (SDs) to
calculate standardised mean differences (SMDs) with
95% confidence intervals (CIs). All meta-analyses
were carried out with random effects models, and
heterogeneity was assessed via the Higgins I2 test.
We identified 20 studies in Embase and 111
studies in PubMed, along with one additional study3
retrieved from the references of the identified
studies. Eighty-six records were excluded: duplicates (n=17), non-English publications (n=6), non-human
studies (n=1), case reports (n=2), letters (n=6),
and articles focused on irrelevant topics (n=54).
We then retrieved 46 articles for full text review,
with the exclusion of seven studies conducted
via questionnaire, 18 studies discussing DED not
related to mask use, three studies discussing other
mask-associated complications, and three studies
which did not include a control group (eg, non–mask-wearing condition) or did not exclude any
confounding conditions. Ultimately, we included
15 articles in our analysis: three prospective studies
with 79 healthy individuals and 133 individuals
with DED, and 12 cross-sectional studies with 1148
healthy individuals and 73 individuals with DED.3 4 5 6 7 8 9 10 11 12 13 14 15 16 17
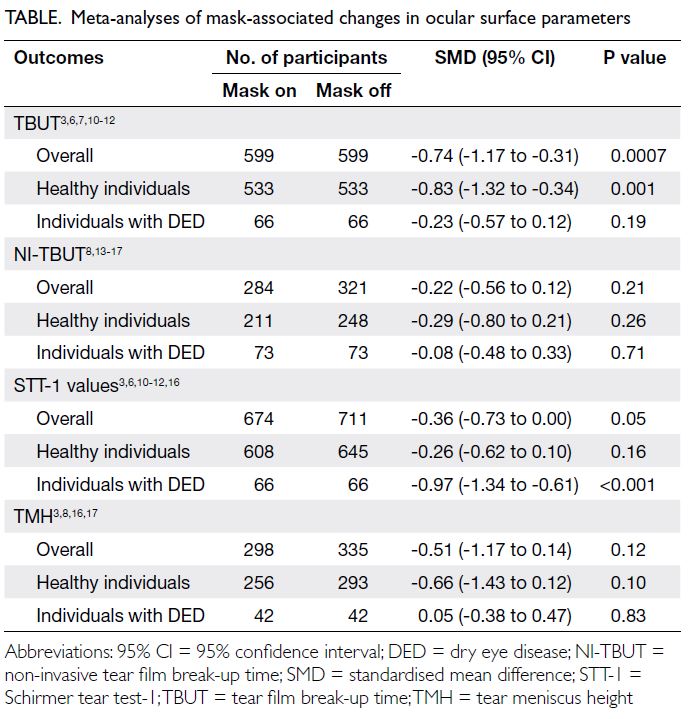
The Table summarised our meta-analyses of the
12 articles related to mask-associated changes in
ocular surface parameters.3 6 7 8 10 11 12 13 14 15 16 17 One article4 was
excluded from the meta-analyses as it did not report
the means and SDs of the parameters, while two
articles5 9 were not included as they only assessed the
Ocular Surface Disease Index (OSDI) score.
Effects on the Ocular Surface Disease Index score
Two prospective studies4 5 and four cross-sectional
studies6 7 8 9 assessed the effect of mask use on the OSDI
score. The OSDI score provides an assessment of a
range of ocular surface symptoms related to DED,
including their severity and functional impact during
the previous week. The score ranges from 0 to 100;
an individual’s status could be regarded as normal
(0-12 points), mild disease (13-22 points), moderate
disease (23-32 points), or severe disease (33-100
points). However, three of four cross-sectional
studies inappropriately used the OSDI score to
evaluate changes in ocular surface symptoms before
and after mask use on the same day,6 7 8 rendering their
results invalid. In the cross-sectional study by Krolo
et al,9 individuals who wore masks for 3 to 6 hours per
day demonstrated significantly higher OSDI scores
compared with the <3 hours per day group (15.3 [interquartile range=8.3-47.7] vs 8.3 [interquartile
range=0.0-35.1]; P=0.001). Similarly, the two
prospective studies, one including 67 individuals
with preexisting DED5 and the other including 17 healthy individuals,4 revealed significant increases in
OSDI score between the mask-wearing period and
pre–mask-wearing period (ie, 2019 and earlier).
Effects on tear film break-up time
Two prospective studies4 10 and five cross-sectional
studies3 6 7 11 12 assessed the effect of mask use on
tear film break-up time (TBUT). In the diagnosis
of dry eye, a cut-off value of <5 or 10 seconds was
adopted to define short TBUT. Although most
studies showed a significantly shorter TBUT during
periods of mask use,3 6 7 11 12 D’Souza et al4 reported
an increase in TBUT during the face-mask–wearing
period (ie, during the SARS-CoV-2 pandemic in
2020) compared with the pre–face-mask period
(ie, end of 2019) without providing mean and SD
values for TBUT. Additionally, Mastropasqua et al10 reported a reduction of TBUT only in individuals
with >6 hours of mask use per day, but not among
individuals with shorter durations of mask use.
Meta-analyses of the six studies with available
mean and SD values for TBUT3 6 7 10 11 12 showed an
SMD of -0.74 (95% CI=-1.17 to -0.31; P=0.0007)
after mask use compared with mask-off conditions.
Subgroup analyses of healthy individuals and
individuals with DED revealed SMDs of -0.83 (95% CI=-1.32 to -0.34; P=0.001) and -0.23 (95% CI=-0.57 to 0.12; P=0.19), respectively (Table).
Effects on non-invasive tear film break-up time
Six cross-sectional studies assessed the effect of mask use on non-invasive TBUT (NI-TBUT).8 13 14 15 16 17
Three studies reported a decrease in NI-TBUT with
mask use,13 14 15 whereas the remaining three studies
showed no significant difference.8 16 17
Because Alanazi et al13 reported median and
interquartile range values only, their study was
excluded from this meta-analysis. The remaining
five studies8 14 15 16 17 indicated no significant decrease
in NI-TBUT after mask use, with an SMD of -0.22
(95% CI=-0.56 to 0.12; P=0.21) [Table].
Effects on Schirmer tear test-1 values
Two prospective studies4 10 and five cross-sectional
studies3 6 11 12 16 assessed the Schirmer tear test-1
(STT-1) values. While three studies revealed a
decrease in STT-1 values with mask use,6 11 12 two
studies showed an increase.4 16 The remaining two
studies3 10 did not demonstrate any difference in
STT-1 values with mask use.
Although D’Souza et al4 measured STT-1
values in their study, they did not report mean
and SD values; thus, their study was excluded
from the meta-analysis. Among the remaining six
studies,3 6 10 11 12 16 the SMD was -0.36 (95% CI=-0.73
to 0.00; P=0.05). Subgroup analyses of healthy
individuals and individuals with DED revealed
SMDs of -0.26 (95% CI=-0.62 to 0.10; P=0.16) and
-0.97 (95% CI=-1.34 to -0.61; P<0.001), respectively (Table).
Effects on tear meniscus height
Four cross-sectional studies assessed tear meniscus
height (TMH)3 8 16 17; no prospective studies assessed
TMH. The study by Schargus et al17 included healthy
individuals and individuals with DED. Although
most studies showed a decrease in TMH with mask
use,3 8 16 one study could not replicate this finding.17
Meta-analysis of the four studies3 8 16 17 showed that
TMH was not altered by mask use (SMD=-0.51;
95% CI=-1.17 to 0.14; P=0.12). Subgroup analyses
of healthy individuals and individuals with DED
demonstrated SMDs of -0.66 (95% CI=-1.43 to 0.12;
P=0.10) and 0.05 (95% CI=-0.38 to 0.47; P=0.83),
respectively (Table).
Discussion
Our analyses showed that mask use was associated
with significant decreases in TBUT. These decreases
were more pronounced in healthy individuals than in individuals with DED. Conversely, subgroup
analyses of STT-1 values showed larger decreases
in aqueous production among individuals with
preexisting DED. These findings suggest a distinct
effect of mask use on individuals with an impaired ocular surface.
Intriguingly, mask use was not associated
with any changes in NI-TBUT or TMH. Although
decreases in NI-TBUT were observed in healthy
individuals and individuals with dry eye, the
inconsistent data collection (ie, use of different
machines) likely contributed to the lack of statistically
significant results. Tear meniscus height can be
considered a surrogate for aqueous tear production;
however, variations in TMH measurement exist (ie,
by slit lamp or anterior segment optical coherence
tomography). These variations could have introduced
substantial imprecision, leading to a lack of statistical
significance.
A possible mechanism for MADE involves
the use of a poorly fitting mask and subsequent
misdirection of exhaled air from the upper
portion of the mask towards the ocular surface,
causing increased airflow and accelerated tear
film evaporation.2 Air leakage can be visualised
by the frequent fogging of glasses when using a
loosely fitted mask or N95 respirator. Consistent
with this hypothesis, there was increased rates of
conjunctivitis, corneal ulcers, tear evaporation, and
ocular irritation among patients with obstructive
sleep apnoea who received continuous positive
airway pressure with an ill-fitting mask.18 A study
also revealed that high airflow from supplementary
oxygen reduces TBUT, TMH, and tear meniscus
area.19 Consequently, taping of the upper mask edge
could potentially reduce air leaks and ensure a more
stable ocular surface.
In addition to MADE, face mask use has been
associated with microbial keratitis20 and chalazion,21
both of which are inflammatory conditions; there
is now evidence to support a pro-inflammatory
environment associated with mask use. Dry eye
disease itself has a strong immunological component;
thus, it is reasonable to anticipate altered ocular
surface stability after mask use. In eyes with DED,
the lack of tear growth factors and immunoglobulins
disrupts normal barrier function, further promoting
microbial infections.
Although the association between mask
use and dry eye symptoms does not outweigh the
protective benefits of masks against communicable
diseases, ophthalmologists should emphasise the
importance of proper mask fit and use; they should
also educate the public about this association.
Alternative strategies to prevent disease spread
during pandemic period, such as vaccination,
should be advocated along with universal masking.
Lubricating eye drops can help restore the tear film, especially in individuals with additional risk factors
(eg, recent ophthalmic surgery or preexisting DED).
Based on their experience with the SARS-CoV-2
pandemic, members of the public are mentally
prepared and knowledgeable about mask use as a
component of personal protection. Face masks will
remain essential for most healthcare workers, and
mask-associated changes in the ocular surface will
continue to be an important topic when SARS-CoV-2
is no longer a public health concern.
Limitations
Our systematic review was limited by the quality
of the primary evidence. The confounding effect
of co-existing ophthalmic conditions could
not be completely eliminated; this may hinder
assessments regarding the effects of mask use
on the ocular surface. Information concerning
ocular surface parameters before the SARS-CoV-2
pandemic was often unavailable, and the inclusion
of a non-mask wearing control group during the
pandemic was impractical in most studies.3 4 5 6 7 13 14 15 16
Additionally, all studies assessed the effect of mask
use on ocular surface parameters without blinding.
Furthermore, there was no information regarding
the type of mask used or whether fit testing had
been performed.4 5 6 7 9 11 13 14 15 Most studies did not
specify the mask-wearing environment or the
environment in which ocular surface parameters
were measured.5 6 10 13 15 Among studies that included
individuals with DED, the type and number of
lubricants used by participants were not specified or
controlled.5 10 14 Many studies utilised an inadequate
wash-out period before measuring ocular surface
parameters in a new condition (either mask-on or
mask-off).3 6 11 13 14 15 17 Finally, highly variable results
were evident for all outcome measurements across
studies, with statistically significant heterogeneity
(I2 values ranged from 74% to 93%; all Q test P
values <0.05). Any mask-associated changes in
ocular surface parameters should be prospectively
investigated using larger, well-characterised sample
populations.
Conclusion
Face mask use was associated with worsened ocular
symptoms, tear film instability, and a marginal
decrease in STT-1 values. Mask use may reduce
NI-TBUT and TMH, depending on the assessment
methods.
Author contributions
Concept or design: All authors.
Acquisition of data: VTT Chan, KW Kam.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: VTT Chan, KW Kam.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Koh S, Rhee MK. COVID-19 and dry eye. Eye Contact
Lens 2021;47:317-22. Crossref
2. Moshirfar M, West WB Jr, Marx DP. Face mask–associated ocular irritation and dryness. Ophthalmol Ther 2020;9:397-400. Crossref
3. Bostanci Ceran B, Ozates S, Arifoglu HB, Tasindi E.
Does facial mask use make our eyes dry? Change in tear
meniscus measurements and conventional dry eye tests
during facial mask use. Eur Eye Res 2022;2:25-9. Crossref
4. D’Souza S, Vaidya T, Nair AP, et al. Altered ocular surface
health status and tear film immune profile due to prolonged
daily mask wear in health care workers. Biomedicines
2022;10:1160. Crossref
5. Scalinci SZ, Pacella E, Battagliola E. Prolonged face mask
use might worsen dry eye symptoms. Indian J Ophthalmol
2021;69:1508-10. Crossref
6. Aksoy M, Simsek M. Evaluation of ocular surface and
dry eye symptoms in face mask users. Eye Contact Lens
2021;47:555-8. Crossref
7. Esen Baris M, Guven Yilmaz S, Palamar M. Impact of
prolonged face mask wearing on tear break-up time and dry
eye symptoms in health care professionals. Int Ophthalmol
2022;42:2141-4. Crossref
8. Giannaccare G, Pellegrini M, Borselli M, Senni C, Bruno A,
Scorcia V. Diurnal changes of noninvasive parameters
of ocular surface in healthy subjects before and after
continuous face mask wearing during the COVID-19
pandemic. Sci Rep 2022;12:12998. Crossref
9. Krolo I, Blazeka M, Merdzo I, Vrtar I, Sabol I, Petric-Vickovic I. Mask-associated dry eye during COVID-19 pandemic—how face masks contribute to dry eye disease
symptoms. Med Arch 2021;75:144-8. Crossref
10. Mastropasqua L, Lanzini M, Brescia L, et al. Face mask–related
ocular surface modifications during COVID-19
pandemic: a clinical, in vivo confocal microscopy, and
immune-cytology study. Transl Vis Sci Technol 2021;10:22. Crossref
11. Shalaby HS, Eldesouky ME. Effect of facemasks on the tear
film during the COVID-19 pandemic. Eur J Ophthalmol
2023;33:145-51. Crossref
12. Tatti F, Mangoni L, Pirodda S, et al. Ocular surface changes
associated with face masks in healthcare personnel during
COVID-19 pandemic. Life (Basel) 2022;12:1491. Crossref
13. Alanazi MA, El-Hiti GA, Al-Tamimi R, et al. Assessment
of the effect of wearing a surgical face mask on tear film in
normal eye subjects. J Ophthalmol 2022;2022:2484997. Crossref
14. Arriola-Villalobos P, Burgos-Blasco B, Vidal-Villegas B, et al.
Effect of face mask on tear film stability in eyes with
moderate-to-severe dry eye disease. Cornea 2021;40:1336-9. Crossref
15. Bilici S, Toprak A, Buyukuysal C, Ugurbas SH. The effect
of day-long mask wearing on non-invasive break-up time.
Graefes Arch Clin Exp Ophthalmol 2022;260:3313-9. Crossref
16. Marta A, Marques JH, Almeida D, José D, Sousa P, Barbosa I.
Impact of COVID-19 pandemic on the ocular surface.
World J Clin Cases 2022;10:9619-27. Crossref
17. Schargus M, Zimzik EM, Fuhrmann L, Geerling G. Influence
of short-term face mask wear on semiautomatically
measured tear film parameters in dry eye patients and
healthy volunteers. Graefes Arch Clin Exp Ophthalmol
2023;261:1045-54. Crossref
18. Matossian C, Song X, Chopra I, Sainski-Nguyen A,
Ogundele A. The prevalence and incidence of dry eye
disease among patients using continuous positive airway
pressure or other nasal mask therapy devices to treat sleep
apnea. Clin Ophthalmol 2020;14:3371-9. Crossref
19. Koh S, Tung C, Kottaiyan R, Zavislan J, Yoon G, Aquavella J.
Effect of airflow exposure on the tear meniscus. J
Ophthalmol 2012;2012:983182. Crossref
20. Tang YF, Chong EW. Face mask–associated recurrent corneal erosion syndrome and corneal infection. Eye
Contact Lens 2021;47:573-4. Crossref
21. Silkiss RZ, Paap MK, Ugradar S. Increased incidence
of chalazion associated with face mask wear during
the COVID-19 pandemic. Am J Ophthalmol Case Rep
2021;22:101032. Crossref