Hong Kong Med J 2014;20:67–9 | Number 1, February 2014
DOI: 10.12809/hkmj134028
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Transnasal penetrating intracranial injury with a chopstick
SK Chan, MB, BS; KY Pang, FRCS, FHKAM (Surgery); CK Wong, FRCS, FHKAM (Surgery)
Department of Neurosurgery, Pamela Youde Nethersole Eastern Hospital,
Chai Wan, Hong Kong
Corresponding author: Dr SK Chan (skc2009@hotmail.com)
Abstract
We report the first case of a transnasal penetrating
intracranial injury in Hong Kong by a chopstick. A
49-year-old man attempted suicide by inserting a
wooden chopstick into his left nose and then pulled
it out. The chopstick caused a transnasal penetrating
brain injury, confirmed by contrast magnetic
resonance imaging of the brain. He was managed
conservatively. Later he developed meningitis without
a brain abscess and was prescribed antibiotics for 6
weeks. He enjoyed a good neurological recovery.
This case illustrates that clinician should have a
high index of suspicion for penetrating intracranial
injury due to a nasally inserted foreign body, even
though it had already been removed. In such cases moreover, brain magnetic
resonance imaging is the imaging modality of choice,
as it can delineate the path of penetration far better
than plain computed tomography.
Case report
A 49-year-old Chinese man, who was a psychiatric
in-patient, self-inserted a wooden chopstick into his left nose and then pulled it out in November 2012. He
was subsequently assessed by an ear, nose and throat
surgeon. No nasal foreign body was seen and there
was no epistaxis. Brain computed tomography (CT)
6 hours after the injury showed a trace amount of
haemorrhage over the right gyrus rectus and a small
amount of pneumocephalus over the right anterior
fossa (Fig 1), and hence the neurosurgical unit was
consulted. Six hours after the incident his vital signs
were stable and he was afebrile; his Glasgow Coma
Scale score was E4M6V4. His speech appeared
confused, as if in a premorbid state. There was no
neurological deficit, and no cerebrospinal fluid (CSF)
rhinorrhoea upon stress testing. Contrast magnetic
resonance imaging (MRI) of the brain was performed
on the next day, which showed a long haemorrhagic
tract extending from right paramidline anterior skull
base, coursing postero-superiorly across medial
right frontal lobe, closely adjacent to the right
frontal horn, and ending at the vertex region (Fig 2), and a trace of intraventricular haemorrhage. On
the same day he developed fever. Lumbar puncture
yielded turbid CSF, with the presence of Gram-positive
cocci, as well as low CSF glucose and high CSF
protein concentrations. Conservative management
was adopted. On an empirical basis, intravenous
ceftriaxone, vancomycin, and metronidazole were
prescribed. Prophylactic anticonvulsant therapy
(phenytoin) was also given. The CSF culture grew
Staphylococcus aureus and Citrobacter koseri. The
antibiotic regimen was switched to intravenous
ceftriaxone and oral metronidazole. The patient’s
recovery was excellent, as reflected by normalisation
of body temperature and inflammatory markers. On day 14, contrast CT brain showed no abscess. He
was well after 6 weeks of antibiotic treatment.
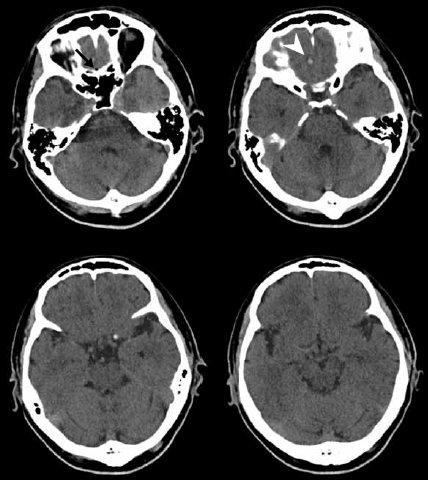
Figure 1. Plain computed tomographic scan of brain (axial cut) showing pneumocephalus (black arrow) and haemorrhage over right gyrus rectus (white arrowhead)
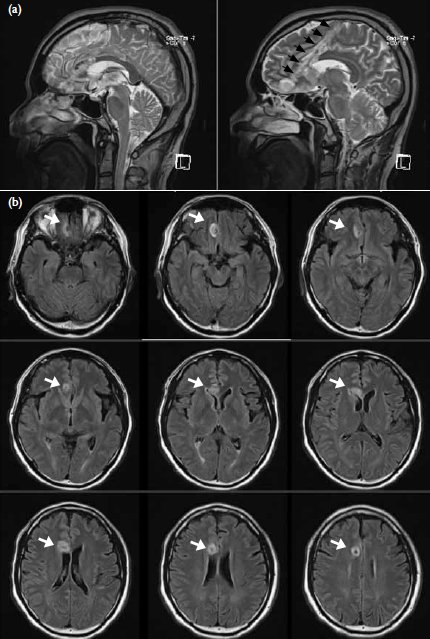
Figure 2. (a) T2-weighted magnetic resonance imaging (MRI) scan of brain (sagittal cut) showing transected track (black arrows). (b) T2-weighted MRI scan of brain in fluid-attenuated inversion recovery sequence (axial cut) showing transected track (white arrows)
Discussion
A literature search of the MEDLINE database
(using the key words "transnasal" and "penetrating
intracranial injury", or the other similar keywords)
was conducted. Approximately 10 case reports were
identified, indicating this was an exceedingly rare
condition. We report the first case of a transnasal
penetrating intracranial injury in Hong Kong by
means of a chopstick. The majority of patients with
this mechanism of injury were due to accidental falls
on objects that enter the nostril,1 while few were
due to attempted suicide. This mode of penetrating
intracranial injury can result in severe complications,
including CSF rhinorrhoea and infection (meningitis
and/or brain abscess).2 The source of the bacteria
could have been from the chopstick or the normal
flora in the nasal cavity/paranasal sinuses. Such injury
can also result in blindness or ophthalmoplegia,3
if the orbital cavity is involved. The most dreadful
complication is severe haemorrhage due to internal
carotid artery injury, which may lead to immediate
death.1 Although foreign body in the nose is a
common presentation, clinicians should always have
a high index of suspicion for possible transnasal
penetrating intracranial injury. Such vigilance
is especially necessary in patients who cannot
volunteer a clear history or complaint (eg children or
psychiatric patients), are febrile, have a neurological
deficit, or have continuous epistaxis.
All patients with penetrating brain
injury should have adequate neuroradiological
examinations.4 Plain CT brain is the initial
investigation of choice to explore for the presence
of any retained radio-opaque material. It can also
reveal presence of an intracranial haematoma or
air, or focal heterogeneous hypodensity suggestive
of brain abscess. Contrast MRI of the brain with
cerebral angiography is the best method of evaluating
penetrating brain injuries. Besides the previously
mentioned abnormal findings, it can also delineate
the track transected by the foreign body, even after it
has been removed, as in this case. Had contrast MRI
brain not been arranged for this patient, penetrating
brain injury would probably have been missed,
given the seemingly unalarming brain CT (Fig 1).
Brain abscess or vascular damage, if any, can also be
appreciated using brain MRI.
Management depends on patient’s condition
and whether a complication has developed.
Neuroendoscopy is a useful operative tool, which
can be employed to remove foreign body or repair
the dural defect causing CSF rhinorrhoea,5 whenever
conservative management fails. Craniotomy may be
warranted if there is a sizable abscess or cerebral
haemorrhage. Since the patient did not have these complications, he was managed conservatively.
Initially, he received empirical intravenous broad-spectrum
antibiotics, as for the treatment of a
bacterial cerebral abscess. The CSF should be
obtained and cultured if the patient has a fever.
Targeted antibiotics can then be used depending
on the sensitivity results. The patient was also
instructed to lie flat to prevent CSF leakage. Short-term
prophylactic anticonvulsant should also be
prescribed.
Conclusion
Herein we report the first patient with a transnasal
penetrating intracranial injury in Hong Kong
resulting from a chopstick. Such injuries confer
significant mortality or morbidity, for which
clinicians should always have a high index of
suspicion. The neuroimaging of choice involves
contrast MRI brain with cerebral angiography. Operative management can be considered for those
patients who have a foreign body in situ, a sizable
abscess or haemorrhage, or CSF rhinorrhoea.
References
1. Ihama Y, Nagai T, Ninomiya K, Fukasawa M, Fuke C, Miyazaki T. A transnasal intracranial stab wound by a plastic-covered umbrella tip. Forensic Sci Int 2012;214:e9-e11. Crossref
2. Hiraishi T, Tomikawa M, Kobayashi T, Kawaquchi T. Delayed brain abscess after penetrating transorbital injury [in Japanese]. No Shinkei Geka 2007;35:481-6.
3. Liu SY, Cheng WY, Lee HT, Shen CC. Endonasal transsphenoidal endoscopy-assisted removal of a shotgun pellet in the sphenoid sinus: a case report. Surg Neurol 2008;70 Suppl 1:S1:56-9.
4. Sharif S, Roberts G, Phillips J. Transnasal penetrating brain injury with a ball-pen. Br J Neurosurg 2000;14:159-60.
Crossref
5. Lee DH, Seo BR, Lim SC. Endoscopic treatment of
transnasal intracranial penetrating foreign body. J
Craniofac Surg 2011;22:1800-1. Crossref

