Hong Kong Med J 2024 Aug;30(4):331.e1-3 | Epub 11 Jul 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Pseudo fat-saturation and orbital lipolysis in cancer cachexia: a diagnostic trap
SM Yu, MB, BS, FRCR; William KM Kwong, BAS, MHlthSc (MRS); Yan YY Law, BSc, MSc; Ann D King, MD, FRCR
Department of Imaging and Interventional Radiology, Prince of Wales Hospital, Hong Kong SAR, China
Corresponding author: Dr SM Yu (fayeyupwr@gmail.com)
A 59-year-old woman was diagnosed in June 2022
with locally advanced nasopharyngeal carcinoma.
She declined standard chemoradiotherapy and
opted to pursue traditional Chinese Medicine. In
May 2023, she presented with bilateral sixth nerve
palsy, poor oral intake, and progressive weight loss
from 32 kg to 20 kg over 6 months.
The restaging positron emission tomography–computed tomography showed that she was
extremely emaciated and had locoregionally
advanced nasopharyngeal carcinoma without
distant metastases (Fig 1). Magnetic resonance
imaging (MRI) of the head and neck revealed diffuse
loss of T1 hyperintense signal in the fat of the
subcutaneous and deep soft tissues and in the bone
marrow of the cervical spine and skull vault giving
the images a pseudo fat-saturated appearance (Fig 2). The scanning parameters were verified to ensure
the correct repetition time and echo time (568 ms and 7 ms, respectively) had been selected. Compared
with the earlier MRI performed in November 2022,
there was complete loss of normal T1-weighted
hyperintense signals in the retrobulbar fat with
development of diffuse oedema and enhancement
in the post-septal orbits (Fig 3); similar changes
with bilateral enophthalmos and diffuse symmetric
enhancement of post-septal orbits were seen on
computed tomography (Fig 4). Overall, this picture
was that of pseudo fat-saturation and orbital
lipolysis in a patient with cancer cachexia. Following
assessment, the patient agreed to undergo palliative
radiotherapy.
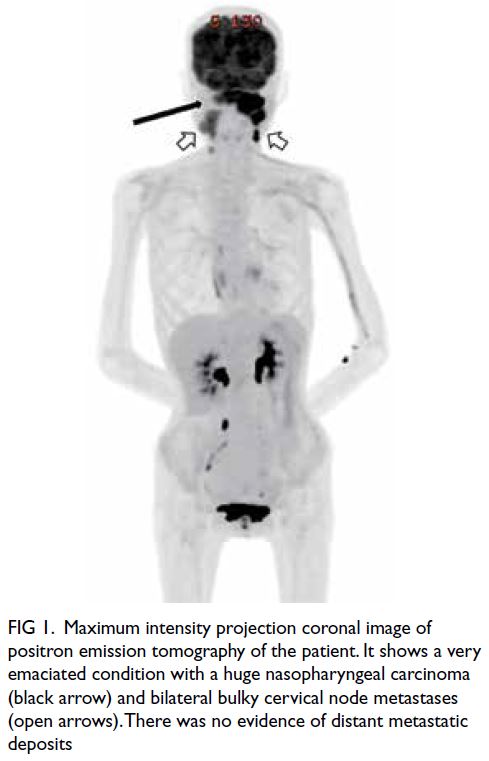
Figure 1. Maximum intensity projection coronal image of positron emission tomography of the patient. It shows a very emaciated condition with a huge nasopharyngeal carcinoma (black arrow) and bilateral bulky cervical node metastases (open arrows). There was no evidence of distant metastatic deposits
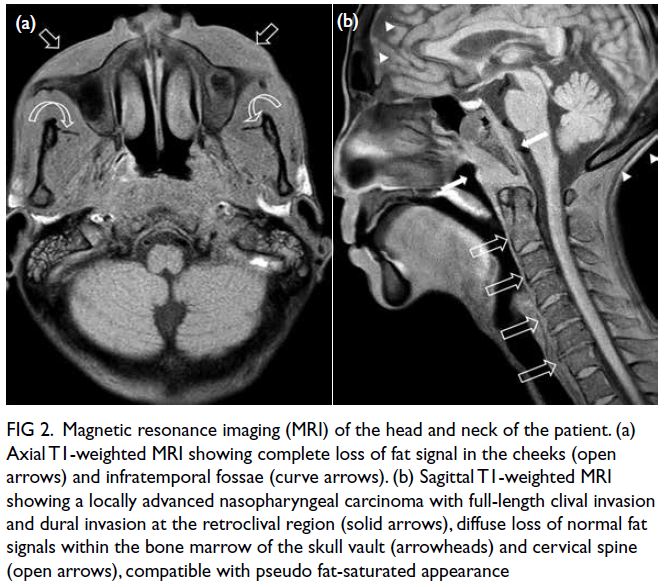
Figure 2. Magnetic resonance imaging (MRI) of the head and neck of the patient. (a) Axial T1-weighted MRI showing complete loss of fat signal in the cheeks (open arrows) and infratemporal fossae (curve arrows). (b) Sagittal T1-weighted MRI showing a locally advanced nasopharyngeal carcinoma with full-length clival invasion and dural invasion at the retroclival region (solid arrows), diffuse loss of normal fat signals within the bone marrow of the skull vault (arrowheads) and cervical spine (open arrows), compatible with pseudo fat-saturated appearance
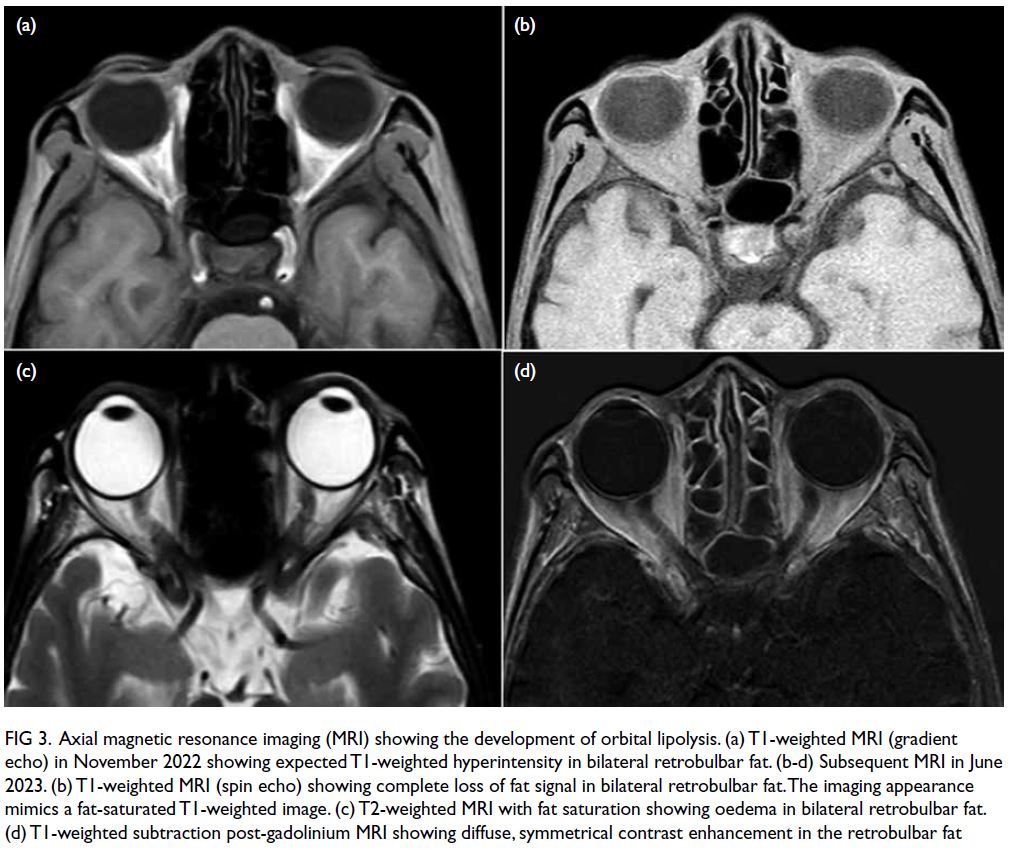
Figure 3. Axial magnetic resonance imaging (MRI) showing the development of orbital lipolysis. (a) T1-weighted MRI (gradient echo) in November 2022 showing expected T1-weighted hyperintensity in bilateral retrobulbar fat. (b-d) Subsequent MRI in June 2023. (b) T1-weighted MRI (spin echo) showing complete loss of fat signal in bilateral retrobulbar fat. The imaging appearance mimics a fat-saturated T1-weighted image. (c) T2-weighted MRI with fat saturation showing oedema in bilateral retrobulbar fat. (d) T1-weighted subtraction post-gadolinium MRI showing diffuse, symmetrical contrast enhancement in the retrobulbar fat
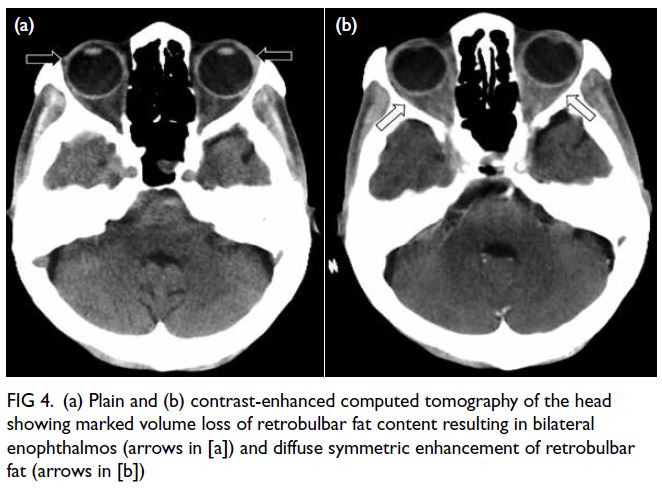
Figure 4. (a) Plain and (b) contrast-enhanced computed tomography of the head showing marked volume loss of retrobulbar fat content resulting in bilateral enophthalmos (arrows in [a]) and diffuse symmetric enhancement of retrobulbar fat (arrows in [b])
Long-term cachexia, a wasting syndrome
common in cancer patients, is marked by extreme
weight loss and malnutrition and can lead to severe
metabolic disturbances that cause excessive lipolysis
and lipid peroxidation. Characteristic imaging
features are often found in severe cases.1 2 3 4 Pseudo fat-saturated
appearance is seen on T1-weighted images
due to complete loss of subcutaneous adipose tissue,
similar to the fat-saturated T1-weighted image.1
Diffuse loss of normal T1-weighted hyperintense
bone marrow signal was a result of bone marrow
fat atrophy and deposition of extracellular
gelatinous substance, a process known as ‘gelatinous
transformation of bone marrow’.2 This loss of fat
signal gives the images an appearance similar to that
of a fat-saturated T1-weighted image. Orbital fat
is typically preserved until the late stages of severe
cachexia during which a condition called orbital
lipolysis may develop.3 4 This condition is related
to endothelial injury and increased permeability of
vessel walls resulting in diffuse oedema and contrast
enhancement in the post-septal orbits.
Cachexia is common in patients with
longstanding cancer and malnutrition. Doctors
should recognise this phenomenon to prevent
attributing these imaging findings to incorrect
scanning parameters or alternative diagnoses. The
diffuse hypointense T1-weighted bone marrow
signal might be misdiagnosed as widespread
metastatic disease or other bone marrow–infiltrating
diseases such as myelofibrosis or haematological
malignancies, while diffuse orbital oedema and
enhancement may be misdiagnosed as orbital
inflammatory conditions such as idiopathic orbital
inflammation.
Understanding the characteristic imaging
features of long-term cachexia is crucial for doctors to avoid diagnostic pitfalls and unnecessary additional investigations or invasive procedures.
Author contributions
All authors contributed to the concept or design, acquisition
of data, analysis or interpretation of data, drafting of the
manuscript, and critical revision of the manuscript for
important intellectual content. All authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki. The patient provided written informed verbal consent for the publication of this case report.
References
1. Jegatheeswaran V, Chan M, Kucharczyk W, Chen YA.
Pseudo fat-saturated appearance of magnetic resonance
head and neck images in 2 cachectic patients. Radiol Case
Rep 2020;15:2693-7. Crossref
2. Böhm J. Gelatinous transformation of the bone marrow:
the spectrum of underlying diseases. Am J Surg Pathol
2000;24:56-65. Crossref
3. Li J, Rajput A, Kosoy D, et al. Rapid orbital lipolysis
associated with critical illness and colectomy. Radiol Case
Rep 2021;16:2347-50. Crossref
4. Demaerel P, Dekimpe P, Muls E, Wilms G. MRI
demonstration of orbital lipolysis in anorexia nervosa. Eur
Radiol 2002;12 Suppl 3:S4-6. Crossref

