Hong Kong Med J 2023 Dec;29(6):564–5 | Epub 23 Aug 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
LETTER TO THE EDITOR
Survival of out-of-hospital cardiac arrest following a return of spontaneous circulation beyond 30 minutes
KL Hon, MB, BS, MD1; Karen KY Leung, MB, BS, MRCPCH1; KL Chan, MB, ChB, MRCPCH1; WF Hui, MB, ChB, MRCPCH1; KT Chau, MB, BS, FRCPCH1; SY Qian, MD2
1 Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong SAR, China
2 Pediatric Intensive Care Unit, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Corresponding author: Dr KL Hon (ehon@hotmail.com)
To the Editor—There was a local blog report in Hong Kong of a 5-year-old girl who experienced
out-of-hospital cardiac arrest (OHCA) with return
of spontaneous circulation (ROSC) after 31 minutes
and was discharged with an implantable cardioverter
defibrillator.1 However, ROSC within 30 minutes is
usually required for a favourable outcome.2 3
We performed a literature search to determine
the longest time to ROSC and survival rates of OHCA
in children (Table). Out-of-hospital cardiac arrest
in children has a poor prognosis and prolonged
in-hospital resuscitation beyond 30 minutes does
not improve survival.3 Predictors of survival to
discharge include witnessed arrest (P=0.012),
delivery of bystander cardiopulmonary resuscitation
(P=0.003), and duration of resuscitation (P=0.028).
However, none who received more than 30 minutes
of in-hospital resuscitation survived.4 A prospective
study found that no patients who required >2 doses
of adrenaline or in-hospital resuscitation for longer
than 20 minutes survived to discharge.5 However, it
is possible that ROSC beyond 30 minutes has not
been reported, or that this case is an exception.
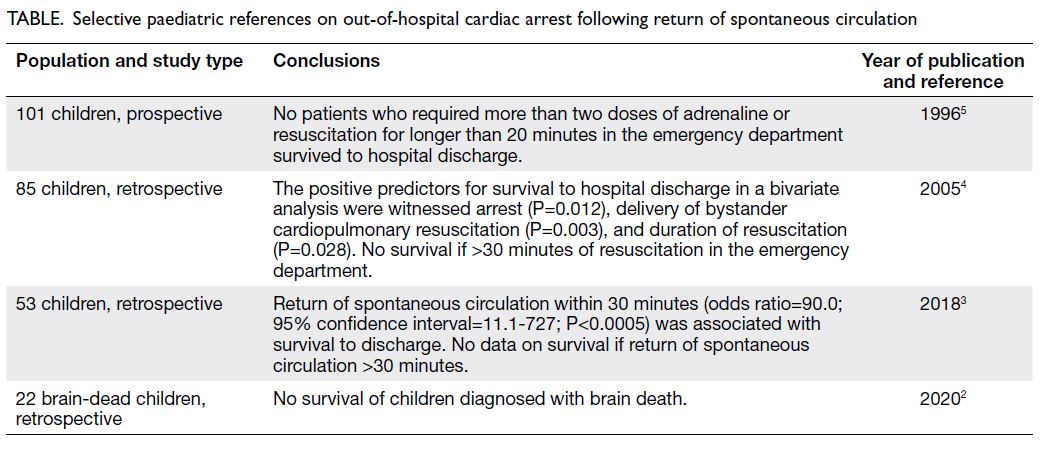
Table. Selective paediatric references on out-of-hospital cardiac arrest following return of spontaneous circulation
Evidence suggests that either death or a poor
outcome is inevitable if OHCA occurs more than 30
minutes from the nearest healthcare facility or the
resuscitation exceeds 30 minutes.6 7 A 2017 study
reported that the survival rate to discharge in Hong
Kong was only 2.3%, which was considerably lower
than the global survival rate in adults (8.8%).8 9 As OHCA in children has not been evaluated in Hong Kong until 2018,3 and prospective evaluation of OHCA in children has not yet been conducted, we concur with Wu10 who suggested the establishment of an OHCA registry.
Many parents and family members who are
present during a resuscitation attempt would want
to be in attendance if their child were likely to die,
and this experience can help with later grieving
without impacting on the resuscitation process. If
appropriate, family-centred care should be practised
and parents should be involved in the decision-making
process.6 As paediatricians, although our
patient is the child, his/her family members are also
important—after all, if the child passes away, it is
the family who must shoulder the lifelong emotional
burden.
In summary, OHCA in children has a poor
prognosis and prolonged resuscitation does not
improve survival or outcome.
Author contributions
All authors contributed to the drafting of the letter and critical revision for important intellectual content. All
authors approved the final version for publication and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have disclosed no conflicts
of interest.
Funding/support
This letter received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Philip. 死去31分鐘的女兒 [in Chinese]. Available from: https://todecidenow.wordpress.com/2021/01/31/死去31分鐘的女兒!/. Accessed 24 Jul 2023.
2. Hon KL, Tse TT, Au CC, et al. Brain death in children: a retrospective review of patients at a paediatric intensive care unit. Hong Kong Med J 2020;26:120-6. Crossref
3. Law AK, Ng MH, Hon KL, Graham CA. Out-of-hospital cardiac arrest in the pediatric population in Hong Kong: a 10-year review at a university hospital. Pediatr Emerg Care 2018;34:179-84. Crossref
4. Tham LP, Chan I. Paediatric out-of-hospital cardiac arrests: epidemiology and outcome. Singapore Med J 2005;46:289-96.
5. Schindler MB, Bohn D, Cox PN, et al. Outcome of out-of-hospital cardiac or respiratory arrest in children. N Engl J Med 1996;335:1473-9. Crossref
6. American College of Surgeons Committee on Trauma; American College of Emergency Physicians Pediatric
Emergency Medicine Committee; National Association
of EMS Physicians; American Academy of Pediatrics
Committee on Pediatric Emergency Medicine; Fallat ME.
Withholding or termination of resuscitation in pediatric
out-of-hospital traumatic cardiopulmonary arrest.
Pediatrics 2014;133:e1104-16. Crossref
7. American Heart Association. Highlights of the 2020 American Heart Association Guidelines for CPR and ECC. 2020. Available from: https://cpr.heart.org/-/media/cpr-files/cpr-guidelines-files/highlights/hghlghts_2020_ecc_guidelines_english.pdf. Accessed 3 Apr 2021.
8. Fan KL, Leung LP, Siu YC. Out-of-hospital cardiac arrest in Hong Kong: a territory-wide study. Hong Kong Med J 2017;23:48-53. Crossref
9. Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care 2020;24:61. Crossref
10. Wu WY. Out-of-hospital cardiac arrest: the importance of a registry. Hong Kong Med J 2019;25:176-7. Crossref

