Hong Kong Med J 2023 Dec;29(6):524–31 | Epub 14 Sep 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Long-term trends in the incidence and management of shoulder dystocia in a tertiary obstetric unit in Hong Kong
Eric HL Chan, MB, ChB, MRCOG; SL Lau, MB, ChB, MRCOG; TY Leung, MD, FRCOG
Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof TY Leung (tyleung@cuhk.edu.hk)
Abstract
Introduction: Because there have been changes in
the management of macrosomic pregnancies and
shoulder dystocia in the past decade, this study was
conducted to compare the incidences of shoulder
dystocia and perinatal outcomes between the
periods of 2000-2009 and 2010-2019.
Methods: This retrospective study was conducted
in a tertiary obstetric unit. All cases of shoulder
dystocia were identified using the hospital’s
electronic database. The incidences, maternal and
fetal characteristics, obstetric management methods,
and perinatal outcomes were compared between the
two study periods.
Results: The overall incidence of shoulder dystocia
decreased from 0.23% (134/58 326) in 2000-2009
to 0.16% (108/65 683) in 2010-2019 (P=0.009),
mainly because of the overall decline in the
proportion of babies with macrosomia (from 3.3%
to 2.3%; P<0.001). The improved success rates of
the McRoberts’ manoeuvre (from 31.3% to 47.2%;
P=0.012) and posterior arm extraction (from 52.9%
to 92.3%; P=0.042) allowed a greater proportion of affected babies to be delivered within 2 minutes
(from 59.0% to 79.6%; P=0.003). These changes led
to a significant reduction in the proportion of fetuses
with low Apgar scores: <5 at 1 minute of life (from
13.4% to 5.6%; P=0.042) and <7 at 5 minutes of life
(from 11.9% to 4.6%; P=0.045).
Conclusion: More proactive management of macrosomic pregnancies and enhanced training
in the acute management of shoulder dystocia led
to significant improvements in shoulder dystocia
incidence and perinatal outcomes from 2000-2009
to 2010-2019.
New knowledge added by this study
- The incidence of shoulder dystocia decreased from 2000-2009 to 2010-2019, mainly because of a reduction in the proportion of babies with macrosomia.
- Perinatal outcomes in cases of shoulder dystocia were improved because of enhanced dystocia relief skills and an overall decline in birth weight.
- Proactive management in cases of suspected macrosomia (eg, early induction of labour) effectively reduced the incidence of shoulder dystocia.
- The incidence of shoulder dystocia was significantly greater among cases with birth weight ≥4200 g, which may be a reasonable threshold for considering elective caesarean section.
- Appropriate training (eg, using SOPHIE course) led to improvements in shoulder dystocia relief skills and better perinatal outcomes.
Introduction
Shoulder dystocia is an uncommon obstetric
emergency with an incidence that reportedly
ranging from 0.58% to 0.7%.1 2 3 It can result in severe
perinatal morbidities, including brachial plexus
palsies, clavicular fractures, humeral fractures,
hypoxic-ischaemic encephalopathy, cerebral palsy,
and even mortality soon after birth.1 2 3 4 5 6 Considering
the unpredictable and complex nature of shoulder
dystocia, many professional bodies have established
systematic approaches with routine training simulations and algorithms to improve fetal outcomes
in such cases.1 2 7 8 9 The most common approach is
represented by the HELPERR mnemonic, which
consists of a sequence of manoeuvres including
the McRoberts’ manoeuvre, suprapubic pressure,
rotational methods, posterior arm delivery, all-fours
position, and clavicular fracture.7 Although the McRoberts’ manoeuvre and suprapubic pressure are
often the preferred initial manoeuvres, their success
rates (56.0%) are lower than that of the rotational
methods (62.4%) and posterior arm delivery (86.1%).5 6 10 The Royal College of Obstetricians and Gynaecologists (RCOG) in 20121 and the American
College of Obstetricians and Gynecologists in
20172 revised their guidelines to indicate that
either posterior arm delivery or rotational methods
can be used after an unsuccessful attempt of the
McRoberts’ manoeuvre. Furthermore, a randomised
controlled trial published in 2015 demonstrated that
the induction of labour at 38 weeks in macrosomic
pregnancies could reduce the risk of shoulder
dystocia, compared with expectant management.11
The overall caesarean rate did not increase when
using this approach. Accordingly, early induction of
labour has become an option in cases of suspected
fetal macrosomia.
Considering changes in the management of
macrosomic pregnancies and shoulder dystocia in
the past decade, this study compared the incidences
of shoulder dystocia, the maternal and fetal
characteristics in such cases, and their obstetric
management methods and perinatal outcomes
between the periods of 2000-2009 and 2010-2019.
Methods
Study design
This retrospective study was conducted in a university tertiary obstetric unit that provided obstetric
services in the New Territories East Cluster of Hong
Kong. All consecutive cases of shoulder dystocia reported from 2000 to 2019 inclusive were identified
using the hospital’s electronic database.12 Shoulder
dystocia was objectively defined as the requirement
of an ancillary obstetric manoeuvre following failed
delivery of the anterior shoulder after downward
fetal neck traction or head-to-body delivery
interval (HBDI) >1 minute, as described in previous
reports.4 5 13 Multiple pregnancies, vaginal breech
deliveries, and known stillbirths before labour were
excluded. Our unit protocol for the management of
shoulder dystocia followed the RCOG Green-top
Guidelines for shoulder dystocia that was published
in 2005 and updated in 2012.1 Beginning in 2002,
hands-on training in shoulder dystocia relief was
routinely conducted using the ALSO (Advanced
Life Support in Obstetrics) program7; the PROMPT
(Practical Obstetric Multi-Professional Training)8
and the SOPHIE (Safe Obstetric Practice for High
risk and Emergency)9 training methods were added in 2011, after the publication of our articles
regarding shoulder dystocia.4 5 The McRoberts’
manoeuvre with or without suprapubic pressure was
usually the first manoeuvre performed, followed by
a rotational manoeuvre or posterior arm delivery
if the McRoberts’ manoeuvre was unsuccessful. A
midwife was designated to document each event,
including the personnel involved, usage and duration
of manoeuvres, and delivery times of the fetal head
and fetal body. Umbilical cord blood was collected
immediately after delivery for blood gas analysis
using a Bayer Rapidpoint 400 Blood Gas Analyzer
(Bayer HealthCare, Seattle [WA], United States), as
described in our previous reports.14 15 Delivery data,
including birth weight and perinatal complications,
were recorded immediately after delivery by the
attending staff, then crosschecked by another staff
member. Two to 3 months later, fetal outcomes were
subjected to further review and confirmation during
postnatal follow-up and monthly audit meetings. All
midwives and obstetricians attended annual training
sessions regarding the management of shoulder
dystocia.
Identified cases and corresponding medical
records were reviewed to collect maternal, fetal, and
obstetric characteristics. Advanced maternal age was
defined as ≥35 years at the estimated date of delivery.
Short stature was defined as maternal height <150 cm.
Maternal body weights at booking and delivery
were recorded to calculate the body mass index
(BMI) at each time point. Obesity was defined as
BMI >30 kg/m2, in accordance with World Health
Organization guidelines.16 17 Parity and diabetes
mellitus/gestational diabetes mellitus statuses were
noted. Obstetric and neonatal characteristics were
recorded, including delivery mode, fetal distress,
birth weight, HBDI duration, and the use and
sequence of manoeuvres. Macrosomia was defined
as birth weight ≥4000 g. Neonatal outcomes were also recorded, including the Apgar scores at 1 minute
and 5 minutes of life, cord arterial pH, and neonatal
complications (eg, subgaleal haemorrhage, hypoxic-ischaemic
encephalopathy, brachial plexus injury,
clavicular fracture, and humeral fracture).
Statistical analysis
The incidences of shoulder dystocia were calculated
for three groups: all singleton live pregnancies
(excluding multiple pregnancies and stillbirths),
all singleton live cephalic-presenting pregnancies
with spontaneous onset of labour (excluding cases
of fetal malpresentation and elective caesarean
deliveries), and all singleton live cephalic-presenting
pregnancies with successful vaginal delivery
(excluding emergency caesarean deliveries).12 The
incidences of shoulder dystocia were also calculated
for various birth weight ranges.
The incidences of shoulder dystocia, maternal
and fetal characteristics in each case, and perinatal
outcomes were compared between 2000-2009 and
2010-2019. Analyses were performed using SPSS
(Windows version 26.0; IBM Corp, Armonk [NY],
United States). The incidences of shoulder dystocia;
maternal, obstetric, and fetal characteristics; and
neonatal complications related to shoulder dystocia
during 2000-2009 and 2010-2019 were analysed
using the Chi squared test and Fisher’s exact test
for categorical variables, t test for parametric continuous variables, and Mann-Whitney U test for
non-parametric continuous variables. The threshold
for statistical significance was set at P<0.05.
Results
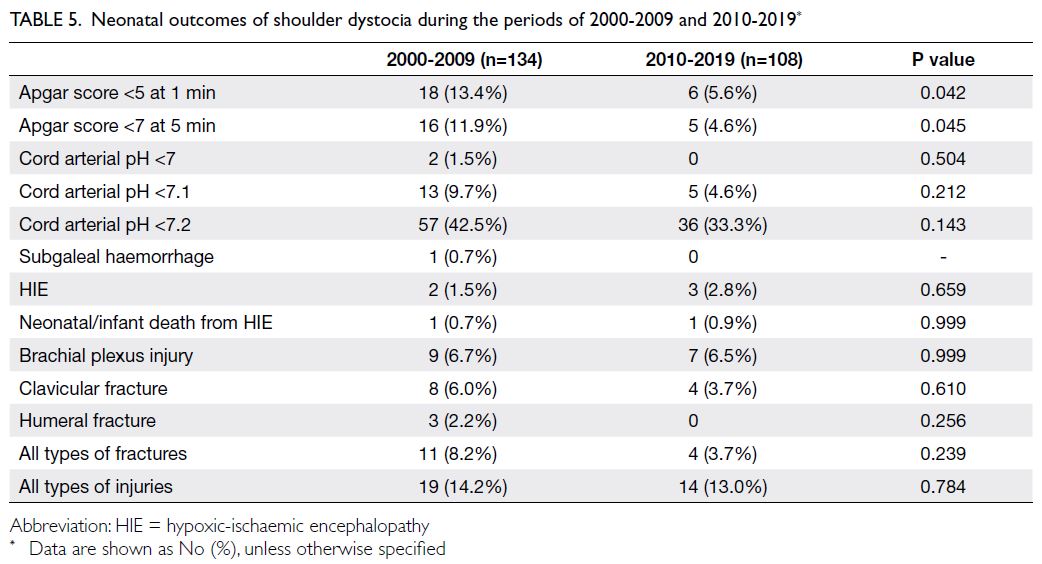
In total, this study included 242 cases of shoulder
dystocia in the study unit. Table 1 shows the
incidences of shoulder dystocia in each decade
according to type of birth and range of birth weight.
The overall incidence of shoulder dystocia among
all singleton live pregnancies decreased from
0.23% (134/58 326) during 2000-2009 to 0.16%
(108/65 683) during 2010-2019 (P=0.009). Similarly,
the incidence of shoulder dystocia among singleton
cephalic-presenting pregnancies with spontaneous
onset of labour decreased from 0.25% to 0.19%
(P=0.031), and the incidence of shoulder dystocia
among singleton cephalic-presenting pregnancies
with vaginal delivery decreased from 0.29% to 0.21%
(P=0.017). The incidences of shoulder dystocia were
generally similar across birth weight categories, but
the incidence considerably decreased in the 4200-4399 g group.
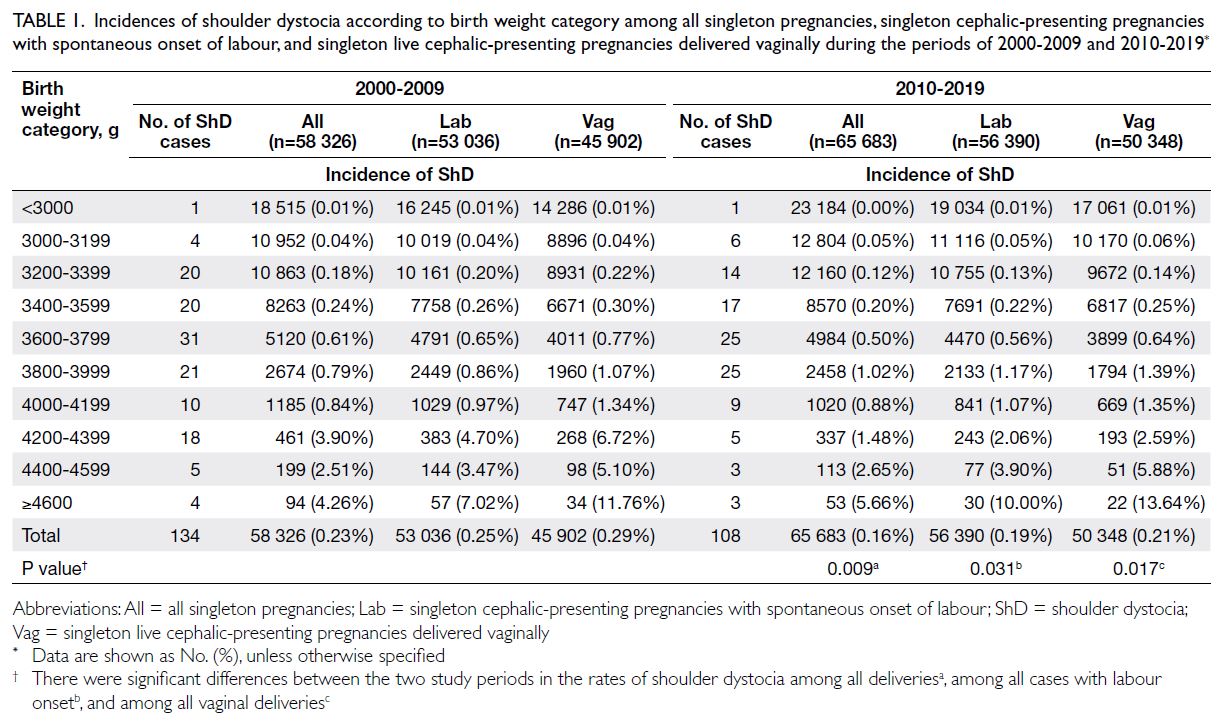
Table 1. Incidences of shoulder dystocia according to birth weight category among all singleton pregnancies, singleton cephalic-presenting pregnancies with spontaneous onset of labour, and singleton live cephalic-presenting pregnancies delivered vaginally during the periods of 2000-2009 and 2010-2019
Table 2 shows the birth weight distribution
for all singleton cephalic live pregnancies. The
mean birth weight decreased from 3180 ± 472 g
during 2000-2009 to 3132 ± 463 g during 2010-2019 (P<0.001). The proportion of babies weighing ≥4000 g was 3.3% during 2000-2009, whereas it was 2.3% during 2010-2019.
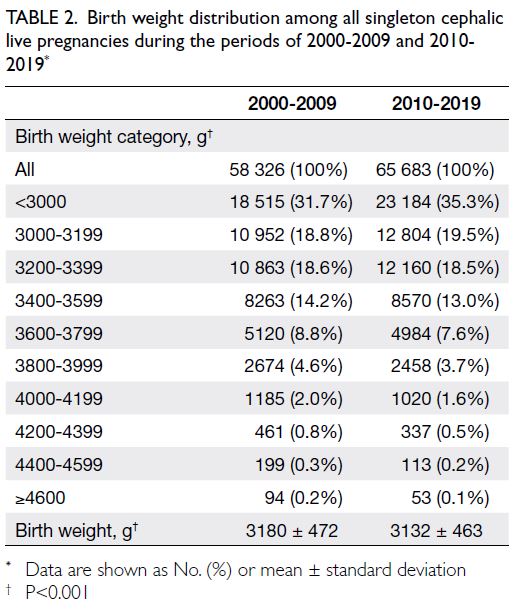
Table 2. Birth weight distribution among all singleton cephalic live pregnancies during the periods of 2000-2009 and 2010-2019
Table 3 illustrates the maternal and obstetric
characteristics in cases of shoulder dystocia during
each decade. There were no statistically significant
differences between the two decades in terms of
advanced maternal age, maternal age, maternal
height, maternal weight at booking and delivery, BMI at booking and delivery, obesity at delivery,
or nulliparity. However, the proportion of shoulder
dystocia cases involving maternal diabetes increased
from 9.0% during 2000-2009 to 19.4% during 2010-2019 (P=0.018). Additionally, the proportion of
shoulder dystocia cases involving instrumental
delivery decreased from 65.7% to 47.2% (P=0.004),
but there was no statistically significant difference in
the proportion of deliveries involving fetal distress.
Although there was no significant change in birth
weight, the proportion of babies with macrosomia
among shoulder dystocia cases tended to decrease
over time (from 27.6% to 18.5%; P=0.097).
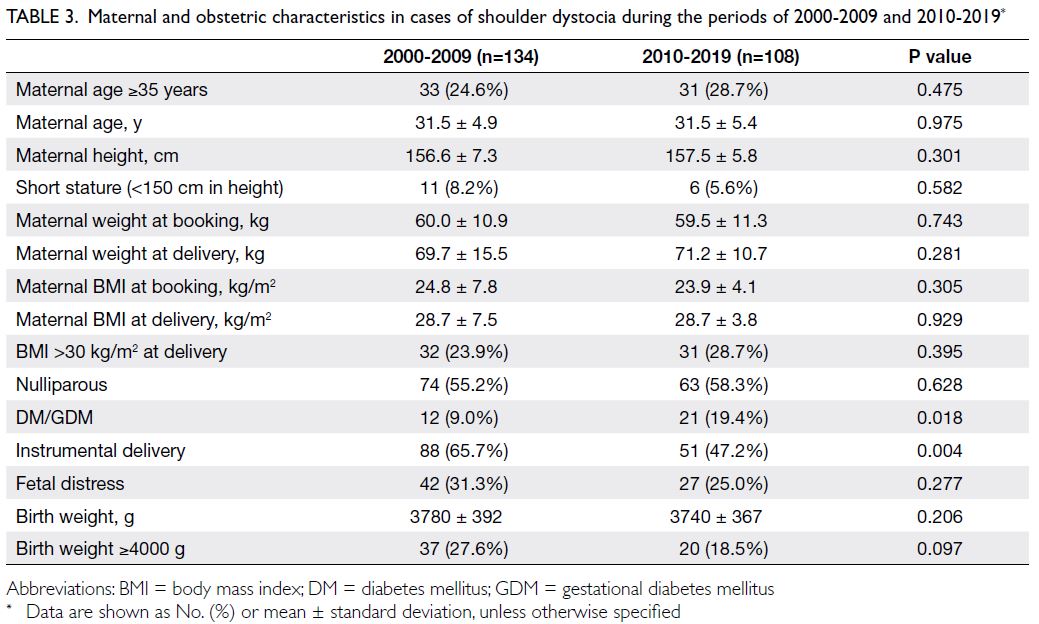
Table 3. Maternal and obstetric characteristics in cases of shoulder dystocia during the periods of 2000-2009 and 2010-2019
Table 4 shows the success rates of various
manoeuvres in terms of alleviating shoulder
dystocia. During 2010-2019, 79.6% of babies in cases
of shoulder dystocia had HBDI ≤2 minutes; 14.8%
and 5.6% of such babies had HBDI of 3-4 minutes
and ≥5 minutes, respectively. These proportions
were significantly better than the proportions during
2000-2009 (59.0%, 31.3%, and 9.7%, respectively;
P=0.003). The success rate of the McRoberts’
manoeuvre in terms of alleviating shoulder dystocia
increased from 31.3% to 47.2% (P=0.012) among all
vaginal deliveries, which was partially attributed
to the increased success rate among instrumental
deliveries (from 20.5% to 39.2%; P=0.017). Although
the rotational manoeuvre continued to be preferred
over posterior arm extraction (77.6% vs. 22.4%)
after failure of the McRoberts’ manoeuvre and
suprapubic pressure, the success rate of posterior
arm extraction increased from 52.9% in 2000-2009
to 92.3% in 2010-2019 (P=0.042). Table 5 shows the neonatal outcomes of shoulder dystocia. There
were significant reductions in the rates of low Apgar
scores: for an Apgar score <5 at 1 minute of life,
the rate decreased from 13.4% to 5.6% (P=0.042);
for an Apgar score <7 at 5 minutes of life, the rate
decreased from 11.9% to 4.6% (P=0.045). There were
no statistically significant changes in the rates of
other neonatal complications.
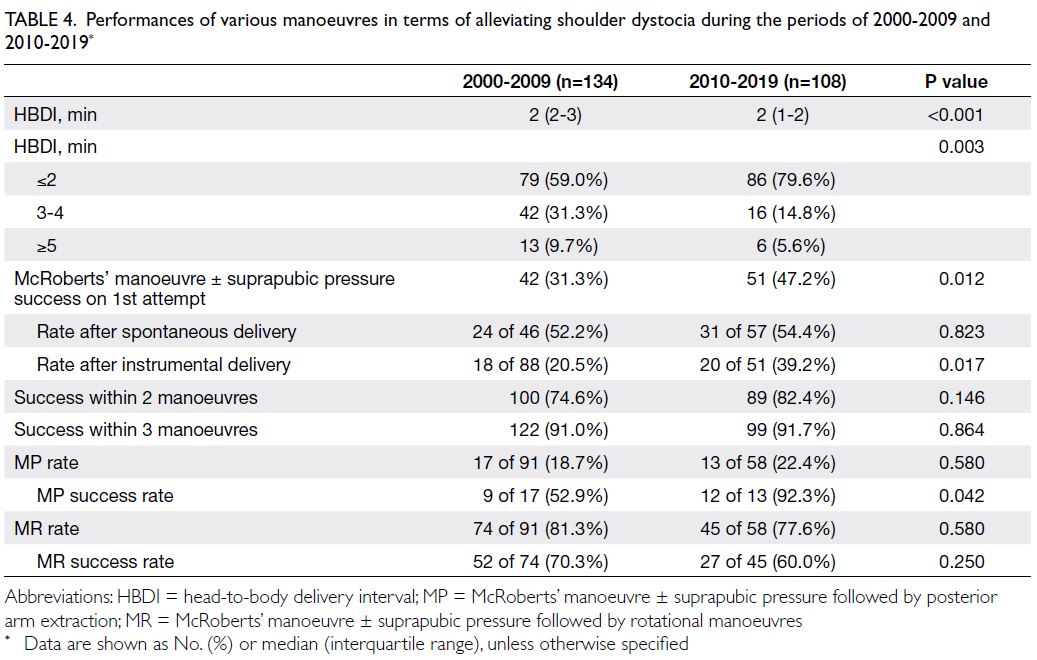
Table 4. Performances of various manoeuvres in terms of alleviating shoulder dystocia during the periods of 2000-2009 and 2010-2019
Discussion
Trend in the incidence of shoulder dystocia
This study revealed a significant reduction in the
overall incidence of shoulder dystocia over the past
two decades in a tertiary obstetric unit in Hong
Kong. One possible reason is the increased use of
caesarean delivery, in both elective and emergency settings, in cases of suspected macrosomia. This
hypothesis is supported by the decrease in the
incidences of shoulder dystocia among all births and
among all pregnancies with onset of labour in the
4200-4399 g subgroup during 2010-2019 (Table 1).
However, such decreases were not observed in other
subgroups with babies weighing ≥4000 g (4000-4199 g, 4400-4599 g, and ≥4600 g) [Table 1]. These
findings suggest that caesarean delivery in cases
of suspected macrosomia is not a major factor
contributing to shoulder dystocia prevention.
Furthermore, the absence of any change in
shoulder dystocia incidence among subgroups with
babies weighing <4200 g was consistent with our
departmental practice of using 4200 g, rather than
4000 g, as a threshold for offering caesarean delivery
to non-diabetic women. The use of a lower fetal
weight threshold (eg, 4000 g) in pregnant Chinese
women could lead to an unnecessary increase in
the rate of caesarean delivery.18 The practice of
early induction of labour in cases of suspected
macrosomia may be the main factor contributing to
the decrease in shoulder dystocia incidence.11 Since
2011, women with a fetal abdominal circumference or estimated fetal weight above the 97th percentile
(but <4200 g) have been counselled about the risk
of difficult labour, along with the benefits and risks
of inducing labour to prevent further macrosomia.
These approaches are consistent with the decreases
in overall mean birth weight and proportion of babies
≥4000 g from 2000-2009 to 2010-2019 (Table 2).
Improvements in the acute management of shoulder dystocia
Additionally, our study revealed improvements
in the acute management of shoulder dystocia. In
particular, the overall success rate of the McRoberts’
manoeuvre in terms of alleviating shoulder dystocia
improved from 31.3% during 2000-2009 to 47.2%
during 2010-2019; these results were consistent with
rates in published reports, which have considerably
varied from 23% to 70%.5 6 19 20 21 Our improved success
rate was mainly attributed to the increased success
rate among instrumental deliveries (from 20.5%
to 39.2%) [Table 4]. We previously speculated that
instrumental delivery increased the risk of shoulder
dystocia while reducing the likelihood of McRoberts’
manoeuvre success, presumably related to delayed
descent of the shoulders during instrumental
delivery.22 The SOPHIE training emphasises that proper performance of the McRoberts’ manoeuvre
should result in cephaloid rotation of the mother’s
pelvis, manifested by elevation of the mother’s
buttocks from the bed. To achieve this goal, the best
method for hyperflexion of the mother’s hips involves
grasping the back of the mother’s distal thigh and
pushing it in the direction of the mother’s head. By
leaning in the same direction, the clinician can use
their own weight to facilitate hip hyperflexion. A
common mistake is holding the mother’s knee and
pushing at the foot. The resulting force is reduced
and the mother may experience discomfort at the
ankle joint (Fig a and b).9
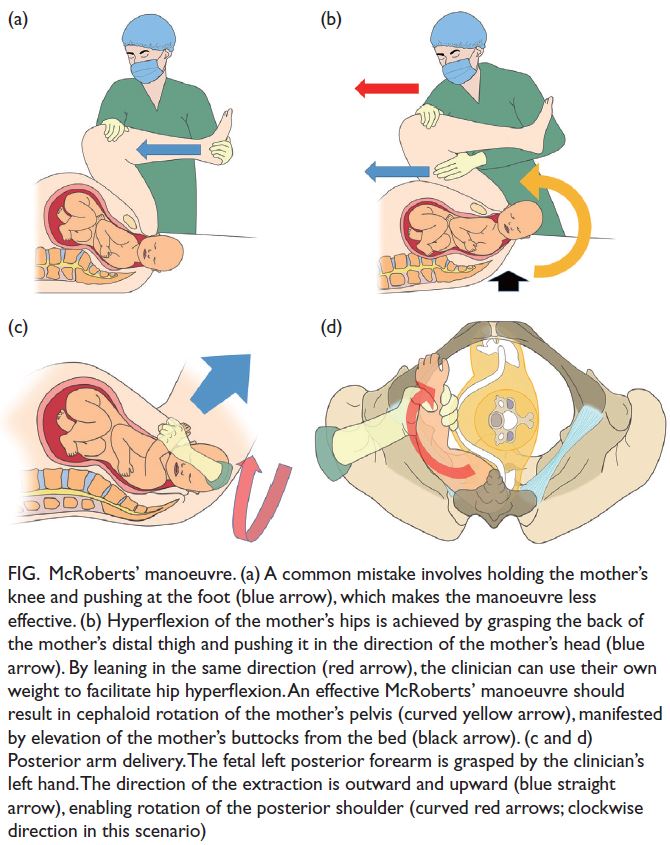
Figure. McRoberts’ manoeuvre. (a) A common mistake involves holding the mother’s knee and pushing at the foot (blue arrow), which makes the manoeuvre less effective. (b) Hyperflexion of the mother’s hips is achieved by grasping the back of the mother’s distal thigh and pushing it in the direction of the mother’s head (blue arrow). By leaning in the same direction (red arrow), the clinician can use their own weight to facilitate hip hyperflexion. An effective McRoberts’ manoeuvre should result in cephaloid rotation of the mother’s pelvis (curved yellow arrow), manifested by elevation of the mother’s buttocks from the bed (black arrow). (c and d) Posterior arm delivery. The fetal left posterior forearm is grasped by the clinician’s left hand. The direction of the extraction is outward and upward (blue straight arrow), enabling rotation of the posterior shoulder (curved red arrows; clockwise direction in this scenario)
Importantly, this study showed an increasing
trend in the utilisation of posterior arm delivery
during 2010-2019, which is consistent with the
updated practice guidelines from the RCOG
and the American College of Obstetricians and
Gynecologists during the same period.1 2 The success
rate of posterior arm delivery also substantially
increased (from 52.9% to 92.3%) [Table 4] and
humeral fracture (a complication associated with
posterior arm delivery) did not occur in any case
during 2010-2019. The improvement in the success
and safety may be related to the enhanced training
through the SOPHIE course, which emphasises that
the clinician should use the correct hand (ie, right
hand for a fetus facing the mother’s left side, and vice
versa); this hand should be inserted into the vagina
with sufficient depth to reach the fetal posterior
forearm, and extraction should be conducted by
grasping the forearm (rather than the elbow or upper arm). The direction of the extraction should
be outward and upward to generate a rotational
effect on the shoulders (Fig c and d).9 10
In addition to enhanced clinician skills,
improved management of shoulder dystocia may
have resulted from a decline in birth weight from
2000-2009 to 2010-2019, although the difference
was not statistically significant. Improvements in
the success rates of the McRoberts’ manoeuvre and
posterior arm delivery led to improved management
of shoulder dystocia, represented by a shorter HBDI
(Table 4). Among cases of shoulder dystocia, the
proportion of babies with an HBDI of ≤2 minutes
increased from 59.0% during 2000-2009 to 79.6%
during 2010-2019; conversely, the proportion of such
babies with HBDI ≥5 minutes decreased from 9.7%
to 5.6% (Table 4). Along with the improvement in
HBDI, fewer babies had a low Apgar score. However,
such improvements did not lead to significant
reductions in the incidences of severe fetal acidosis
and hypoxic-ischaemic encephalopathy, possibly
because of the small sample size. The management of
prenatally missed macrosomia with severe shoulder
dystocia remains a substantial challenge. Our group
recently reported a severe case of shoulder dystocia
in which the posterior shoulder was also lodged
in the middle of the pelvic cavity. The situation
was resolved by our modified posterior axillary
sling traction technique, which involved using a
ribbon gauze to form a sling, in combination with
long and slim right-angle forceps to facilitate sling
placement.23 In our report as well as in our recent
review, we emphasised that the sling primarily
functions by facilitating shoulder rotation to enable
delivery through the wider diagonal diameter of the
outlet of the birth canal.10
Strengths and limitations
The strengths of this study include its analysis
of a relatively large number of women over two
decades, the use of complete and audited outcomes
data, and the uniform management of pregnancy
complications in accordance with standard
guidelines and department protocols.12 However,
because this was a retrospective study, causal factors
underlying the findings could not be fully elucidated;
possible confounding factors included changes
in the management of pregnancy complications,
management of babies with macrosomia, and
management of shoulder dystocia, as well as changes
in the levels of skills and experience among clinical
personnel during the study period.
Conclusion
More proactive management of macrosomic
pregnancies led to decreases in the overall
proportion of babies with macrosomia and incidence of shoulder dystocia from 2000-2009 to 2010-2019.
Improvements in shoulder dystocia relief skills were
demonstrated by increases in the success rates of
manoeuvres (eg, the McRoberts’ manoeuvre and
posterior arm delivery), as well as decreases in HBDI
and Apgar scores.
Author contributions
All authors contributed to the concept or design of the study, acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content. All authors
had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Conflicts of interest
The corresponding author is the programme director for the Safe Obstetric Practice for High risk and Emergency
(SOPHIE) course. Other authors have disclosed no conflicts
of interest.
Acknowledgement
The authors thank the creators of the SOPHIE course (https://www.obg.cuhk.edu.hk/training-education/sophie-course/) and Ms Catherine Chan at the Department of Obstetrics
and Gynaecology, The Chinese University of Hong Kong for
contributing to the illustrations.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethical approval was obtained from the Joint Chinese
University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (Ref No.: CRE 2017.442).
Informed patient consent was waived by the Committee due
to the retrospective nature of the study.
References
1. Royal College of Obstetricians and Gynaecologists. Shoulder Dystocia. Green-Top Guideline No. 42. 2nd
Edition. London: Royal College of Obstetricians and
Gynaecologists. 2012. Available from: https://www.rcog.org.uk/media/ewgpnmio/gtg_42.pdf. Accessed 14 Aug 2023.
2. Practice Bulletin No 178: Shoulder Dystocia [editorial]. Obstet Gynecol 2017;129:e123-33. Crossref
3. Leung TY, Chung TK. Severe chronic morbidity of childbirth. Best Pract Clin Res Obstet Gynaecol 2009;23:401-23. Crossref
4. Leung TY, Stuart O, Sahota DS, Suen SS, Lau TK, Lao TT. Head-to-body delivery interval and risk of fetal acidosis and hypoxic ischaemic encephalopathy in shoulder dystocia: a retrospective review. BJOG 2011;118:474-9. Crossref
5. Leung TY, Stuart O, Suen SS, Sahota DS, Lau TK, Lao TT. Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG 2011;118:985-90. Crossref
6. Hoffman MK, Bailit JL, Branch DW, et al. A comparison of obstetric maneuvers for the acute management of shoulder dystocia. Obstet Gynecol 2011;117:1272-8. Crossref
7. American Academy of Family Physicians. Advanced Life Support in Obstetrics (ALSO®). Available from: https://www.aafp.org/cme/programs/also.html. Accessed 7 Jan 2022.
8. PROMPT Maternity Foundation. Practical Obstetric Multi-Professional Training. Available from: https://www.promptmaternity.org. Accessed 7 Jan 2022.
9. Department of Obstetrics and Gynaecology, The Chinese
University of Hong Kong & Prince of Wales Hospital.
SOPHIE Course–Safe Obstetric Practice for High risk and
Emergency Course. Available from: https://www.obg.cuhk.edu.hk/training-education/sophie-course/. Accessed 14 Aug 2023.
10. Lau SL, Sin WT, Wong L, Lee NM, Hui SY, Leung TY. A critical evaluation of the external and internal maneuvers
for resolution of shoulder dystocia. Am J Obstet Gynecol. In press. Crossref
11. Boulvain M, Senat MV, Perrotin F, et al. Induction of labour versus expectant management for large-for-date fetuses: a randomised controlled trial. Lancet 2015;385:2600-5. Crossref
12. Wong ST, Tse WT, Lau SL, Sahota DS, Leung TY. Stillbirth rate in singleton pregnancies: a 20-year retrospective study from a public obstetric unit in Hong Kong. Hong Kong
Med J 2022;28:285-93. Crossref
13. Spong CY, Beall M, Rodrigues D, Ross MG. An objective definition of shoulder dystocia: prolonged head-to-body
delivery intervals and/or the use of ancillary obstetric
maneuvers. Obstet Gynecol 1995;86:433-6. Crossref
14. Leung TY, Lok IH, Tam WH, Leung TN, Lau TK. Deterioration in cord blood gas status during the second
stage of labour is more rapid in the second twin than in the first twin. BJOG 2004;111:546-9. Crossref
15. Leung TY, Tam WH, Leung TN, Lok IH, Lau TK. Effect of twin-to-twin delivery interval on umbilical cord blood gas in the second twins. BJOG 2002;109:63-7. Crossref
16. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-63. Crossref
17. Leung TY, Leung TN, Sahota DS, et al. Trends in maternal obesity and associated risks of adverse pregnancy outcomes
in a population of Chinese women. BJOG 2008;115:1529-37. Crossref
18. Cheng YK, Lao TT, Sahota DS, Leung VK, Leung TY. Use of birth weight threshold for macrosomia to identify fetuses at risk of shoulder dystocia among Chinese populations. Int J Gynaecol Obstet 2013;120:249-53. Crossref
19. McFarland MB, Langer O, Piper JM, Berkus MD. Perinatal outcome and the type and number of maneuvers in shoulder dystocia. Int J Gynaecol Obstet 1996;55:219-24. Crossref
20. Gherman RB, Goodwin TM, Souter I, Neumann K, Ouzounian JG, Paul RH. The McRoberts’ maneuver for the
alleviation of shoulder dystocia: how successful is it? Am J
Obstet Gynecol 1997;176:656-61. Crossref
21. Spain JE, Frey HA, Tuuli MG, Colvin R, Macones GA, Cahill AG. Neonatal morbidity associated with shoulder dystocia maneuvers. Am J Obstet Gynecol 2015;212:353.e1-5. Crossref
22. Lok ZL, Cheng YK, Leung TY. Predictive factors for the success of McRoberts’ manoeuvre and suprapubic pressure in relieving shoulder dystocia: a cross-sectional study. BMC Pregnancy Childbirth 2016;16:334. Crossref
23. Kwan AH, Hui AS, Lee JH, Leung TY. Intrauterine fetal death followed by shoulder dystocia and birth by modified posterior axillary sling method: a case report. BMC Pregnancy Childbirth 2021;21:672. Crossref